Hip motion in the transverse plane is coupled with foot motion in the frontal plane during closed kinematic activities, such as gait. Considering that movement patterns and bone alignment might influence passive mechanical properties of joints in the long term, it is possible that hip passive stiffness and foot complex stiffness and alignment are related to each other.
ObjectivesTo investigate whether hip passive stiffness, midfoot passive stiffness and shank-forefoot alignment are related to each other.
MethodThirty healthy adult individuals with a mean age of 25.4 years participated (18 women and 12 men). The Foot Torsimeter was used to measure midfoot stiffness, and hip stiffness and foot alignment were measured using clinical measures. Pearson and Spearman correlation coefficients were calculated to test the associations between each pair of variables, with α = 0.05.
ResultsHip stiffness was positively correlated with midfoot absolute stiffness (r = 0.41, p = 0.02), indicating that increased hip stiffness is associated with increased midfoot stiffness. There were no associations between shank-forefoot alignment and the other variables.
ConclusionsIn clinical settings, individuals with reduced hip passive stiffness may also have reduced midfoot passive stiffness, and vice versa. Shank-forefoot alignment is not linearly associated with hip or midfoot passive stiffness.
Passive mechanical properties of the lower limb joints are related to the movement patterns of the joints during closed kinematic activities, such as gait.1,2 For example, reduced passive mechanical resistance to internal rotation of the hip is associated with increased hip and knee internal rotation and foot pronation during the stance phase of gait.2 In addition, Souza et al.3 demonstrated that hip internal rotation stiffness predicts peak rearfoot eversion during the stance phase of walking. Thus, modification of the passive mechanical properties of hip joint tissues, such as hip external rotator stiffness, seems to influence not only hip movement patterns but also knee and foot motion during gait.
Foot complex characteristics may also influence lower limb movement patterns during gait.4 Previous studies have shown that increased varus forefoot alignment is associated with increased foot pronation and increased shank and hip internal rotation during gait.5,6 In addition, recent studies have demonstrated that reduced passive mechanical resistance of the midfoot is associated with increased foot pronation, increased knee internal rotation, and increased hip range of motion (ROM) in the transverse plane during gait.1,2 Thus, alterations of the mechanical properties of the foot complex, such as midfoot stiffness, might also influence lower limb movement patterns during gait.
Healthy adults walk between 4000 and 18,000 steps per day.7 Therefore, the movement pattern of the lower limb joints during gait may modify the passive mechanical properties of these joints in the long term, locally and nonlocally. For example, increased foot pronation due to increased shank-forefoot alignment and/or reduced midfoot passive stiffness may increase shank and hip internal rotation and, in the long term, lead to reduced hip passive stiffness because of repetitive increased hip internal rotation.8 Similarly, increased hip internal rotation due to reduced hip passive stiffness might increase hip and shank internal rotation and consequently increase foot pronation, leading to reduced midfoot stiffness in the long term.2 Thus, this study investigated the relationship between hip passive stiffness, midfoot passive stiffness, and shank-forefoot alignment. Our hypothesis was that reduced midfoot stiffness would be associated with reduced hip stiffness and that reduced hip and midfoot stiffness would be associated with greater shank-forefoot alignment.
MethodsParticipantsThis is a cross-sectional observational study. Asymptomatic adult of both sexes participated in this study. The sample size was determined using the software G*Power with the following input data: a bivariate normal correlation model, a desired statistical power of 80%, a significance level of 0.05, and an expected correlation of 0.5, which resulted in 30 participants. They were recruited through posters displayed across university buildings and through direct contacts with students in the laboratory. The recruitment and data collection occurred between January and March 2018.
The inclusion criteria were as follows: age between 18 and 44 years; body mass index less than 25 kg/m² (to allow proper muscle palpation during hip passive stiffness measurement); no neurological or orthopedic health conditions; no history of injuries or surgery in the lower limbs or in the lumbar-pelvic complex in the last year; no physical activities on the day of data collection; a minimum ROM of 20° of hip internal rotation; and not using foot orthoses in the last year. The exclusion criteria were inability to perform the procedures or report of discomfort or pain during data collection, but none of the participants were excluded. All the participants signed a consent form approved by the Universidade Federal de Minas Gerais’s Ethical Research Committee (CAAE: 78785717.7.0000.5149).
Instruments and proceduresAll procedures were performed at the Movement Analysis Laboratory of the Univesidade Federal de Minas Gerais. First, participants' mass and height were measured, with an anthropometric weight balance (Filizola, MIC200, Brazil). Then, foot alignment was measured following the procedures described by Mendonça et al.9 The left lower limb data were collected because the equipment designed to measure midfoot mechanical resistance (ie, The Foot Torsimeter) was designed to assess the left side. The participant remained in the prone position, and the leg was positioned neutrally in the transverse plane so that the calcaneus was uppermost, the medial malleoli were aligned with the inferior edge of an examination table, and the knee of the contralateral limb was flexed. The individual was stabilized to the examination table with a Velcro strap attached to the pelvis. A rod was fixed with Velcro under the metatarsal heads, and a bisection line was drawn on the posterior side of the shank. The participant's ankle was then passively positioned at 0° dorsiflexion, and the participant was asked to actively hold the ankle in this position. Three pictures were taken from a top view using a digital camera (Nikon D-SLR D5000; Nikon Inc, Melville, NY), as described by Mendonça et al.9 The shank-forefoot alignment was measured with a goniometer as the angle between the rod attached to the forefoot and the bisection line drawn on the posterior side of the shank (Fig. 1A). The mean angle in degrees of the three pictures was used for analysis. In a pilot study with 10 participants, this measure had test-retest intraclass correlation coefficient (ICC3,3) of 0.87; 95% confidence interval (CI): 0.48 to 0.97; standard error of measurement (SEM): 1.91°.
Hip stiffness was operationally estimated as the position of first detectable resistance.10 With the participant lying in the prone position on an examination table, a belt fastening the pelvis, the right knee was extended, and the left knee was flexed at 90°. The left hip was passively rotated in the transverse plane three times by the examiner for hip soft tissue viscoelastic accommodation. The examiner, holding the left knee at 90° of flexion but without limiting or forcing hip movement, allowed passive hip internal rotation to occur until the tension of the hip passive structures stopped this movement. Thus, the “position of first detectable resistance” or hip stiffness was defined as the joint position in which the torque produced by the shank and foot weights became equal to the passive resistant torque generated by the hip external rotator structures. This position was measured using an analog inclinometer placed at the anterior border of the tibia, 5 cm distal to the previously marked tibial tuberosity (Fig. 1B). This measurement was performed three times, and the mean angle value in degrees was considered for analysis. The greater the amount of hip internal rotation, the lesser the hip stiffness. Finally, this value was multiplied by -1 so that lower values correspond to lower stiffness and higher values correspond to greater stiffness. In the pilot study with 10 participants, this measure had test-retest ICC 3,3 of 0.98; 95% CI: 0.86, 1.00; SEM: 0.07°.
The Foot Torsimeter was used to measure the midfoot mechanical resistance.11 This instrument has two supports: one to rest and stabilize the participant's shank and rearfoot through rigid straps and adjustable clamps and another applied to the forefoot with a height-adjustable clamp to stabilize the forefoot region. In addition, it has a potentiometer and torque meter that measure the forefoot torsion angle in the frontal plane and the midfoot resistance to inversion, respectively.
For the midfoot passive stiffness measurement, the participant sat on a chair with the left shank, rearfoot, and forefoot fixed to the Foot Torsimeter and the potentiometer axis aligned with the second metatarsal bone. The hip was in a neutral position in the frontal and transverse planes, the thigh was parallel to the ground, and the shank had 45° of inclination relative to the ground. The examiner asked the participant to keep the shank and foot completely relaxed during data collection. Then, the participant's forefoot ROM was determined. The examiner passively moved the forefoot up to approximately 20° of eversion and 50° of inversion (Fig. 1C). This measurement was performed at an angular velocity of approximately 2°/s, with only trials in which the average velocity was between 1.8°/s and 2.2°/s accepted. The velocity was displayed on the computer screen for real-time feedback. This slow angular velocity was determined in a previous study11 to avoid muscle contractions. First, three trials were performed for viscoelastic accommodation, and then three valid trials were performed. In a pilot study with 10 participants, this measure had test-retest ICC of 0.98; 95% CI: 0.93, 0.99; SEM: 0.01 Nm/°.
Data reductionFor passive midfoot stiffness, only the torque-angle data between 20˚ and 50˚ of forefoot eversion—inversion were filtered with a Chebyshev 3rd order low-pass filter with a 4 Hz cutoff frequency.11 Then, a smoothness analysis was conducted for each angle time series to identify and rule out trials with notable irregularities. The slopes between the frames of each time series were calculated (Nm/degree). Slope change rates were presented as a percentage of the slope from frame-to-frame interval. To define time series with high slope change rates, a quartile analysis was performed for all change rate values obtained from all participants and trials. The highest accepted change rate was defined as the third quartile (75% percentile), which represented 18% of the slope change. Thus, time series with change rates greater than 18% were excluded from the analysis. Of the 99 time-series obtained, three from each participant, 83 were retained for analysis—at least one time series from each participant. Then, the average midfoot passive stiffness was obtained, calculated as the maximum instantaneous inclination of the angular time series using the 4th order polynomial method.1,11
Data analysisFor sample characterization, descriptive statistics were used for all variables. Data were tested for normal distributions using the Shapiro-Wilk test. Only midfoot passive stiffness was not normally distributed. Then, Pearson correlation coefficients were used to test the association between hip passive stiffness and shank-forefoot alignment, and Spearman correlation coefficients were used to test the association between midfoot passive stiffness and hip passive stiffness and shank-forefoot alignment data. The significance was set at α = 0.05. The strength of the correlations was interpreted as follows: small if r < 0.3; moderate if 0.3 ≤ r < 0.5; and high if 0.5 ≤ r ≤ 1.12 SPSS 24.0 software (SPSS Inc., Chicago, IL) was used for all analyses.
ResultsThirty healthy adults participated in this study (18 women, 12 men). They had a mean ± standard deviation age of 25.4 ± 4.39 years, height of 170 ± 0.09 cm, and body mass of 63.03 kg ± 9.86 kg. Means and standard deviations for hip internal rotation ROM, hip stiffness, midfoot stiffness, and shank-forefoot alignment were 69.76 ± 2.21°, 35.36 ± 9.69°, 0.22 ± 0.07 Nm/º, and 16.88 ± 4.17°, respectively.
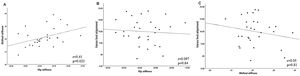
Table 1 presents the results of the correlation analysis. Hip stiffness was positively correlated with midfoot stiffness with moderate strength (r = 0.41; p = 0.02). There were no associations between shank-forefoot alignment and the other variables. The scatter plot for the relationship between hip stiffness and midfoot stiffness is shown in Fig. 2.
DiscussionThis study investigated the relationship between hip stiffness, midfoot stiffness, and shank-forefoot alignment. The results are partially in agreement with our initial hypotheses, since less hip stiffness was associated with less midfoot stiffness. However, there was no association between shank-forefoot alignment and the other variables. The relationship between hip stiffness and midfoot stiffness might be explained by the functional relationship between foot motion in the frontal plane and hip motion in the transverse plane during closed kinematic activities, such as walking.13
Hip stiffness being positively associated with midfoot stiffness can be explained by the fact that foot pronation is coupled with hip internal rotation during the stance phase of gait.14–16 In addition, more recent studies demonstrated that less midfoot mechanical resistance is related to increased foot pronation and hip internal rotation during the stance phase of gait.1,2 In this context, increased hip internal rotation caused by reduced midfoot stiffness might act as a stretching force to the hip external rotator tissues.2,8 Over time and with use, the increased hip internal rotation, with lack of proper hip muscle performance,17 might increase the length and flexibility of the hip external rotators and consequently reduce their stiffness.
Similarly, but from a proximal to distal joint direction, reduced hip stiffness might also modulate midfoot stiffness.18 More specifically, reduced hip stiffness has been related to increased foot pronation,2 which, in the long term, might contribute to loosening of the midfoot tissues and consequently reduce their stiffness. The relationship between hip and midfoot stiffness demonstrated by the present study should be considered in clinical settings during the assessment and implementation of interventions designed to modify these tissues’ mechanical properties and related movement patterns, because injuries such as patellofemoral and hip osteoarthritis can be influenced by distal and proximal factors at the hip and foot.1,2,19–21 For example, hip strengthening has been used to reduce foot eversion during running and step down.22,23 However, hip strengthening did not modify hip and knee movement pattern in the frontal and transverse planes during gait. Therefore, future studies should consider the findings of the present study to further develop and test hip interventions designed to modify lower limb motion, such as hip external rotators strengthening in the extended or shortened position, which might modify hip stiffness and consequently hip and ankle motion during different activities, such as gait.24 Moreover, future studies could investigate whether interventions designed to increase hip or midfoot stiffness, such as hip and intrinsic foot muscle strengthening, are also able to modify this relationship. Finally, other variables, such as generalized laxity, sex, hormones, and level of physical activity, may influence this relationship and can be considered in future studies.
The present study demonstrated that hip stiffness and midfoot stiffness were not associated with shank-forefoot alignment. This result can be explained by the fact that while the midfoot and hip measurements refer to passive tissue stiffness, the shank-forefoot measurement provides information about bone segment alignment. This finding is not in accordance with a previous study demonstrating a negative correlation between varus foot alignment and midfoot mechanical resistance with moderate strength.25 This difference can be explained by the fact that our study used midfoot stiffness to represent mechanical midfoot resistance, while Paes et al.25 used mean torque and mean torque normalized by body mass, and although these variables are correlated, they might represent different midfoot tissue mechanical properties.
The method used to assess hip stiffness might be a limitation of this study, since it may not be appropriate for individuals with femoral retroversion. Nevertheless, this is a valid measure10 in which the examiner presented excellent reliability. In addition, although the method we used to measure shank-forefoot alignment is reliable and has been previously used in different studies,3,23,25,26 there are no data about its concurrent validity with radiographic measurement. Moreover, we only used one of the measures of midfoot passive mechanical resistance provided by the Foot Torsimeter.11 Therefore, other variables related to midfoot passive mechanical resistance might have different relationships with hip stiffness and shank-forefoot alignment. Finally, the present study investigated the relationship between hip and midfoot passive stiffness in healthy and young individuals, which might not reflect the relationship between hip and midfoot stiffness in individuals with injuries and during functional tasks, such as walking and running, since during movement there is an active modulation of stiffness by means of muscular contraction.27
ConclusionThis study showed that hip stiffness and midfoot stiffness are positively correlated, with moderate strength. Therefore, reduced hip stiffness is related to reduced midfoot stiffness. However, shank-forefoot alignment was not related to hip stiffness and midfoot stiffness measures.
Conflicts of interestThe authors have no conflicts of interest.
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001. We are also thankful to the State of Minas Gerais Funding Agency FAPEMIG [grant number APQ-01139-15] and to the Brazilian Funding Agency CNPQ [grant number 428735/2018-5].