To investigate the effects of underwater ultrasound (US) therapy in 48 patients with moderately active rheumatoid arthritis (disease activity score in 28 joints [DAS28]>3.2 and<5.1).
MethodsPatients randomly assigned to the ultrasound group (n=25) received underwater continuous ultrasound therapy to both wrists and hands for 7min per session with an intensity of 0.7W/cm2 for 10 sessions. The control group (n=23) received sham treatment under the same conditions. At baseline, at the end of treatment (end of Week 2) and at the follow-up visit (Week 14), the following outcomes were evaluated: disease activity (erythrocyte sedimentation rate [ESR], C-reactive protein [CRP], tender and swollen joint counts, pain on a visual analog scale, DAS28, hand function (fist making, wrist extension and flexion, hand grip strength) and quality of life (Health Assessment Questionnaire [HAQ]).
ResultsA significant decrease in C-reactive protein at the end of Week 2 and Week 14 compared to control group (mean between-group difference at 2 weeks=−5.77, 95% CI=−10.86 to −0.68, mean between-group difference at 14 weeks=−5.07, 95% CI=−10.13 to −0.01), and non-significant decrease in DAS28 was observed. By the end of treatments at the end of week 2, ultrasound alleviated pain significantly (mean between-group difference at two weeks=−8.35 95% CI=−16.12 to −0.58), as well as improved left wrist extension compared to the control group (mean between-group difference at 14 weeks=4.35, 95% CI=1.09–7.60).
ConclusionUnderwater ultrasound therapy was better than sham treatment at the end of 2 weeks of treatment, but not at long term (14 weeks) in patients with rheumatoid arthritis.
Clinical trial registration number: NCT02706028 (https://clinicaltrials.gov/ct2/show/NCT02706028)
Rheumatoid arthritis (RA) is an autoimmune inflammatory disease affecting multiple joints (mainly the wrists and small joints of the hand) with a prevalence of about 0.5–1.0%.1 RA is most common in middle-aged people.2 Without adequate treatment and care, RA may lead to joint damage and disability. A decrease in the ability to make a closed fist and hand grip strength can occur in the hands; subluxation and limitation of flexion and extension may develop in to the wrists.
Non-pharmacological treatment options such as physical therapy along with chemical and biological disease modifying anti-rheumatic drugs (DMARDs) can be used to preserve physical function and improve quality of life in addition to reducing pain and inflammation.
Ultrasound (US) therapy has been used for medical purposes for more than 70 years. Its biological effects are still not exactly known. The effectiveness of ultrasonic therapy is influenced by its application parameters such as intensity, frequency, continuous or pulsed current, time of irradiation, and type of coupling agent.3 As air reflects almost 100% of the ultrasonic beam on the transducer/air interface, a suitable coupling medium has to be utilized to allow an effective transmission.4,5 Casarotto et al.3 investigating the transmission properties of four coupling agents (gel, degassed water, mineral oil and petrolatum) found, that gel and water had the highest transmission coefficient and the lowest reflection. Water as a coupling agent is preferable when irregular body parts and bony prominences with little soft tissue coverage are treated, such as small joints of the hand. Compared to contact mode of treatment, in case of underwater US should be used at a higher intensity to achieve the same tissue temperature.6 When calculating the intensity, the distance of the transducer from the treated surface should be taken into consideration.7
Previous research results have already confirmed the effects of US therapy on pain and function in a range of musculoskeletal disorders.8–11 For example Mehmet et al.8 observed benefits in patients with temporomandibular joint disorder. Similarly, Boyaci et al. found positive results in patients with knee osteoarthritis9 by using ultrasound therapy. Unlike pain and physical function, there has not been any evidence that ultrasound treatment can alter inflammation.
The aim of this clinical trial was to determine the effects of underwater US therapy in patients with RA; analgesic and anti-inflammatory effects (primary endpoint), effects on joint function and quality of life (secondary endpoint). It was decided to treat the wrists and the small joints of the hands, since they are the most prevalent, but not equally affected joints during the disease.
MethodsThis randomized, placebo-controlled, assessor- and patient-blinded trial was conducted in accordance with the ethical principles of the Helsinki Declaration and the guidelines of the International Conference on Harmonization of Good Clinical Practice. The study was approved by the Regional Research Ethics Committee, Győr, Hungary (approval number: 76-1-7/2013) and registered in ClinicalTrials.gov (registration number: NCT02706028). Patients were informed verbally about the study procedures, read the Patient Information Sheet and asked to sign an Informed Consent Form.
PatientsInclusion criteria: Patients over 18 years of age (mean: 62.94±9.27 years) with mild-to-moderate (DAS28>3.2 and <5.1) rheumatoid arthritis meeting the American College of Rheumatology (ACR) diagnostic criteria were enrolled into the study. Further inclusion criterion was a stable-dose pharmacotherapy (DMARDs therapy, Non-steroidal Antiinflammatory Drugs – NSAIDs, steroids) given for at least 2 months. Patients were not allowed to receive physical therapy treatments for 1 month prior to starting the study.
Exclusion criteria included other concomitant autoimmune diseases, stable-dose pharmacotherapy for less than 2 months, and conditions contraindicating US therapy (infection; fever; osteomyelitis).
Study proceduresThe study was conducted at the Physiotherapy Division of the Rheumatology Outpatient Clinic of Petz Aladár County Teaching Hospital in Hungary.
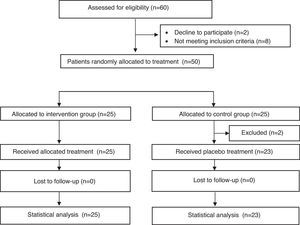
Sixty patients were screened and 50 patients were enrolled into the trial. Eight patients did not meet inclusion criteria, and two patients refused to sign the Informed Consent Form. All 50 eligible patients were randomly allocated into two groups (ultrasound group and control group). The allocation was concealed by using seales, opaque envelopes.
Patients in the ultrasound group received 10 applications (10 working days) of continuous underwater US therapy (35–36 Celsius degree tap water; with the transducer at a distance of 2cm from the treated surface) intensity of 0.7W/cm2 SATA (spatial average – temporal average [continuous]), for 7min to the palmar and dorsal aspects of each hand and wrist using a 830kHz ULTRON home OE-302 device with treatment head size of 4.2cm2 (BNR: max.5:1, energy: 1234.8J, power: 2.94W). Each side of the hand and the wrist were treated in the same treatment period. The control group received sham treatment (the US device was not turned on) during the 10 sessions for 7min per session.
The study was considered completed and data were analyzed, if the patient participated in at least 80% of the treatment sessions and attended the follow-up visits. During the 3-month follow-up period, patients were asked not to have any physical therapy treatment or to change their medication. (The analgesic or anti-inflammatory drugs were documented). The outcome parameters were recorded by 1 blinded rheumatologist before the initiation of treatment (at Week 0 – Outcomes Testing 1), immediately after the 10 treatment sessions (at the end of Week 2 – Outcomes Testing 2), and 3 months later (at Week 14 – Outcomes Testing 3).
Randomization and blindingA concealed allocation random assignment of the enrolled patients to the treatment groups was performed (using an Excel computer program) by an independent investigator who had never met the patients and was not otherwise involved in the study procedures. The study was double-blinded, as neither the study participants nor the testing investigator (a rheumatologist) knew the treatment assignments. The statistician was not involved in the randomization procedures.
Outcome parametersAt inclusion, the age and gender of patients as well as duration of the disease and DMARD therapy (in years) were recorded. Inflammatory laboratory parameters (i.e. erythrocyte sedimentation rate [ESR], C-reactive protein [CRP] – these are the most current used parameters for inflammation considering their costs), disease activity (measured using Disease Activity Score in 28 Joints [DAS28]), quality of life (measured using Health Assessment Questionnaire [HAQ]), number of painful and swollen joints, severity of pain at rest recorded on a 100mm visual analog scale for pain (VASp), and duration of morning joint stiffness (in minutes) were assessed at each of the 3 Outcomes Measure Testing sessions (Week 0 [before treatment}, 2 [after last treatment session], and 3 months later). Physical function was assessed by measuring range of motion in the wrists (in degrees), degree of fist making (based on nail tilting, 3 grades were used: 0: insufficient, 1: incomplete, 2: complete); and hand grip strength (in kg) was measured with a JAMAR dynamometer. At the end of treatment period (Outcome Measure 2) and at the Month 3 follow-up visit (Outcome Measure 3), patients evaluated their own condition on a 4-grade scale (1: significantly improved, 2: improved, 3: unchanged, 4: worsened).
Statistical analysisStatistical analysis was performed by using the IBM SPSS 20 software. The statistical power was 60%. Normality was verified with the Kolmogorov–Smirnov test. The difference between the groups was expressed using mean differences and 95% confidence interval (95% CI). Chi-squared test was used for categorical data. Missing data was imputed using the Last Observation Carried Forward (LOCF) method. We did not use an intention to treat analysis approach.
ResultsFifty rheumatoid arthritis patients receiving care at the Rheumatology Outpatient Clinic were involved in the study, which was conducted between 2013 and 2014. Forty-eight patients completed the study i.e. attended at least 80% of the treatment sessions. Two patients did not start treatment and were excluded from the analysis (i.e. an intention to treat analysis was not performed – Fig. 1).
The US group and the control group included 25 and 23 patients, respectively. Regarding demographic data, disease duration, and background therapy duration, the groups were similar at baseline (Table 1).
Demographic data, disease duration, and background therapy duration in the two study groups to show the effects of underwater ultrasound therapy on pain, inflammation, hand function and quality of life in patients with rheumatoid arthritis.
| Variable | Ultrasound group (n=25) | Control group (n=23) |
|---|---|---|
| Age (years) | 63.24 (11.04) | 62.83 (7.25) |
| Disease duration (years) | 13.04 (9.30) | 14.03 (13.49) |
| DMARD therapy duration (years) | 10.67 (8.60) | 12.35 (12.91) |
| Male | 6 (24) | 4 (17) |
| Female | 19 (76) | 19 (83) |
Continuous data is expressed as mean (SD), categorical data is expressed as n (%).
Inflammatory parameters, including ESR and CRP decreased in the US group at each successive outcomes measure testing session compared to baseline. In the ultrasound group, only CRP levels showed a significant improvement (i,e. a decrease) immediately after treatment (Outcome Measure 2) and at the follow-up visit (Outcome Measure 3) when compared to the control group (CRP: mean between-group difference visit 2–1=−5.77, 95% CI=−10.86 to −0.68, mean between-group difference visit 3–1=−5.07, 95% CI=−10.13 to −0.01). Disease activity index decreased in both groups at the end of treatment (Outcome Measure 2) and at Month 3 (Outcome Measure 3) compared to baseline, but the difference between the groups was not significant (DAS28: mean between-group difference visit 2–1=−0.18, 95% CI=−0.61 to 0.25, mean between-group difference visit 3–1=−0.37, 95% CI=−0.84 to 0.09). Pain sensation decreased in both groups compared to baseline, and this decrease was significant in the US group at the end of Week 2 (Outcome Measure 2) (VAS: mean between-group difference visit 2–1=−8.35, 95% CI=−16.12 to −0.58). No substantive changes were observed in the duration of morning joint stiffness, the number of tender and swollen joints in any of the groups at any outcome test session, and no difference was found between the groups. Quality of life measured using HAQs improved in the US group, but the difference between the two groups was not significant. Extension and flexion of the wrists improved non-significantly from baseline in the US group and did not change in the control group. In the ultrasound group, only left wrist extension showed a significant improvement at Week 2 (Outcome Measure 2) when compared to the control group (mean between-group difference Outcome Measure 2−1=4.35, 95% CI=1.09–7.60). The degree of fist making did not show any changes in any of the groups. Hand grip strength slightly increased in the US group, but the difference between the two groups was not statistically significant. Patients of both the US group and the control group considered their own condition improved at the end of treatment (Outcome Measure 2) and at the Month 3 follow-up visit (Outcome Measure 3). Changes in the studied parameters and statistical data are shown in Tables 2 and 3. No adverse events were observed during the study.
Means±SD at baseline, at end of Week 2 and Week 14 for the two study groups (treated group: patients receiving underwater ultrasound and control group: receiving sham treatment) and between-group differences at end of Week 2 and Week 14 to show the effects of underwater ultrasound therapy on pain, inflammation, hand function and quality of life in patients with rheumatoid arthritis.
| Group | Outcome Measure 1 (Week 0) | Outcome Measure 2 (end of Week 2) | Outcome Measure 3 (Week 14) | Mean between group differences at visit 2–1 (95% CI) | Mean between group differences at visit 3–1 (95% CI) | |
|---|---|---|---|---|---|---|
| mean±SD | mean±SD | mean±SD | ||||
| ESR (mm/h) | Treated | 23.64±18.06 | 22.00±18.07 | 19.16±12.81 | −4.59 (−11.44 to 2.26) | −5.05 (−11.15 to 1.06) |
| Control | 22.30±12.20 | 25.26±16.38 | 22.87±12.50 | |||
| CRP (mg/l) | Treated | 11.12±9.38 | 7.49±9.85 | 6.00±8.35 | −5.77 (−10.86 to 0.68) | −5.07 (−10.13 to 0.01) |
| Control | 6.17±7.84 | 8.31±8.97 | 6.12±7.59 | |||
| DAS28 | Treated | 3.98±0.67 | 3.35±0.96 | 3.29±1.09 | −0.18 (−0.61 to 0.25) | −0.37 (−0.84 to 0.09) |
| Control | 4.10±0.65 | 3.66±0.70 | 3.78±0.88 | |||
| HAQ | Treated | 1.35±0.80 | 1.26±0.91 | 1.12±0.85 | −0.19 (−0.55 to 0.17) | −0.22 (−0.49 to 0.04) |
| Control | 1.36±0.50 | 1.45±0.56 | 1.35±0.63 | |||
| Morning stiffness (min) | Treated | 20.08±29.10 | 17.48±19.67 | 18.76±27.46 | −1.73 (−11.21 to 7.75) | 1.11 (−18.52 to 20.75) |
| Control | 20.17±37.60 | 19.30±37.57 | 17.74±28.16 | |||
| Tender joint count | Treated | 3.32±2.12 | 3.06±2.70 | 2.68±3.35 | 1.17 (−0.57 to 2.91) | 0.01 (−1.80 to 1.83) |
| Control | 4.43±3.51 | 3.00±2.89 | 3.78±3.41 | |||
| Number of swollen joints | Treated | 1.32±1.44 | 0.70±1.13 | 0.68±1.52 | −0.10 (−0.81 to 0.61) | −0.47 (−1.53 to 0.60) |
| Control | 1.04±1.40 | 0.52±0.90 | 0.87±1.52 | |||
| VAS | Treated | 52.80±20.26 | 38.80±22.42 | 44.00±26.85 | −8.35 (−16.12 to 0.58) | −4.89 (−18.02 to 8.25) |
| Control | 48.91±15.30 | 43.26±16.21 | 45.00±13.22 | |||
| Right wrist extension (degree) | Treated | 57.40±16.36 | 60.52±17.47 | 59.08±17.95 | 5.12 (−0.03 to 10.27) | 2.38 (−3.60 to 8.35) |
| Control | 58.91±22.41 | 56.91±23.46 | 58.22±24.33 | |||
| Right wrist flexion (degree) | Treated | 46.84±14.40 | 48.52±12.12 | 49.16±14.96 | 0.81 (−4.68 to 6.30) | 1.75 (−4.73 to 8.24) |
| Control | 43.04±22.47 | 43.91±20.31 | 43.61±20.31 | |||
| Left wrist extension (degree) | Treated | 59.96±18.95 | 63.96±17.80 | 64.72±16.87 | 4.35 (1.09 to 7.60) | 5.93 (−0.05 to 11.92) |
| Control | 64.96±22.66 | 64.61±23.30 | 63.78±24.96 | |||
| Left wrist flex. (degree) | Treated | 46.96±16.90 | 47.92±17.50 | 49.96±17.06 | 0.70 (−4.86 to 6.27) | 2.96 (−2.35 to 8.27) |
| Control | 51.43±18.07 | 51.70±17.61 | 51.48±15.79 | |||
| Hand grip strength, right (kg) | Treated | 12.60±7.19 | 14.13±8.25 | 14.52±9.03 | 1.87 (−0.47 to 4.20) | 0.93 (−2.18 to 4.05) |
| Control | 13.30±7.31 | 12.94±6.59 | 14.28±7.71 | |||
| Hand grip strength, left (kg) | Treated | 13.55±6.97 | 14.14±7.86 | 14.81±8.34 | 0.21 (−1.51 to 1.93) | 0.52 (−2.16 to 3.19) |
| Control | 12.57±6.80 | 12.94±6.59 | 13.32±6.91 |
ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; DAS28, disease activity score in 28 joints; HAQ, Health Assessment Questionnaire; VASp, visual analog scale – pain.
Where confidence intervals of different parameters do not contain 0 (zero), there are statistically significant differences between groups.
Changes in degree of fist making and patients’ impression in the study groups to show the effects of underwater ultrasound therapy on pain, inflammation, hand function and quality of life in patients with rheumatoid arthritis.
| Outcome Measure 1 | Outcome Measure 2 | Outcome Measure 3 | Outcome Measure 1 pa | Outcome Measure 2 pa | Outcome Measure 3 pa | ||
|---|---|---|---|---|---|---|---|
| Degree of fist making, right hand (3 grades) | Treated | 5/11/9 | 3/12/10 | 5/10/10 | 0.64 | 0.28 | 0.51 |
| Control | 7/10/6 | 7/8/8 | 8/7/8 | ||||
| Degree of fist making, left hand | Treated | 6/9/10 | 5/8/12 | 5/8/12 | 0.85 | 0.95 | 0.87 |
| Control | 4/9/10 | 5/8/10 | 4/9/10 | ||||
| Patient impression (1–4) | Treated | 2.24±0.78 | 2.40±0.76 | 0.51 | 0.83 | ||
| Control | 2.39±0.66 | 2.39±0.66 | |||||
In this randomized, double-blinded, placebo-controlled trial both the primary endpoint parameters (i.e. pain and inflammation) and the secondary endpoint parameters (HAQ and hand function) showed significant improvement in the short term in patients with RA treated with ultrasound. Pain measured on a VAS also decreased, although to a lesser extent, in the control group, which could be due to placebo effect.12 The anti-inflammatory effect could be supposedly due to vasodilation caused by the thermal effect. Cruz et al. found, that 1MHz continuous (0.4W/cm2 SATA), or pulsed (20% duty cycle, 0.08W/cm2 SATA) ultrasound therapy improved endothelial function in humans, which has an anti-inflammatory vascular effect. They postulated that a mechanical effect, which stimulated nitrogen-monoxid production resulting in vasodilation.13 According to Watson, the overall influence of US in the inflammed tissue was pro-inflammatory, which enablesd tissue repair.4 This could explain the results of Hashish et al.14 testing the value of US for reducing postoperative inflammation. They described a placebo-mediated mechanism with maximum anti-inflammatory effect in the placebo group.14 In the present study, the decrease of CRP in the control group could have been due to the normal tissue repair, which was enhanced by the therapy in the ultrasound group. Based on the meta analysis of Robertson and Baker15 in 2001, the randomized controlled trials evaluating US therapy are heterogenous in terms of the investigated parameters and the dosage of US. In the majority of the studies, no significant differences were found in outcomes between humans treated with ultrasound or placebo US.15 In case of underwater therapy, water is a coupling medium that allows ultrasound transmission to the biological tissue. Underwater treatment has the advantage of enabling the treatment of small joints of the hand simultaneously and effectively. Clinical studies have confirmed the beneficial effects of underwater US therapy in RA. The Ottawa Methods Group found level “A” evidence for pain relief, and level “C” evidence for the decrease in joint swelling and morning joint stiffness.16 Hawkes et al.17 compared three treatment groups, all including 10 patients: exercises and wax baths, exercises with ultrasound, and exercises with ultrasound and faradic hand baths. The 3MHz continuous ultrasound with an intensity of 0.250W/cm2 was applied in water to the palmar aspect of the hand for 3minutes, five times a week, for 3 weeks. These authors did not find significant differences between the three groups with regard to pain, grip strength, proximal interphalangeal joint circumference, articular index, range of motion or level of activity.17 In the study by Konrád,18 the effects of underwater US therapy were compared to placebo treatment in 50 RA patients. US was applied to the dorsal and palmar aspects of the hand, at 0.5W/cm2 continuously, for ten minutes on alternate days for 3 weeks. Significant improvement in the number of tender and swollen joints, joint stiffness, and dorsiflexion of wrists were reported in patients receiving ultrasound therapy, as compared to sham treatment.18
Considering secondary endpoint parameters, a significant change in wrist extension and quality of life was observed in the US group when compared to the control group. Wrist extension improved more than flexion, which is explained by the nature of the disease (i.e. impairment of extension is more pronounced during the course of the disease). Favorable changes in quality of life were only short-term. In 2002, based on data gathered from the Cochrane Database, Casmiro et al.19 found that in rheumatoid arthritis, US therapy increased hand grip strength, to a lesser degree decreased the tender and swollen joint counts, morning hand stiffness and improved wrist dorsal flexion. US therapy combined with other physical therapy methods was not better than US therapy alone.19 In the present study, no significant changes in hand grip strength were found, which could be explained by the long (more than 10 years) disease duration. Krawczyk-Wasielewska et al. have confirmed that in cases of longer RA disease duration, the primary effect of physical therapy was pain relief, while range of motion of the joints improved to a lesser extent.20 In rheumatoid arthritis, a decrease in pain and improvement in function both have a beneficial effect on quality of life in the long term.
Limitations of the studyThe weakness of our study was the small sample size and lack of intention to treat analysis. We are planning to extend our study and involve more patients even in a multicenter setting, which may increase the power of the study and provide more precise results.
ConclusionSimilar to previous results, our randomized trial has shown favorable short-term effects of underwater US therapy on pain, quality of life, and joint function in patients with rheumatoid arthritis but in the long-term it was not superior to sham treatment.
Conflicts of interestThe authors declare no conflicts of interest.