Forward head posture (FHP) is a forward positioning of the head relative to the trunk in the sagittal plane. This posture is one of the most prevalent poor postures in patients with head and neck pain. Rehabilitative Ultrasound Imaging (RUSI) is a reliable method to objectively evaluate muscle thickness and function.
ObjectiveTo compare thickness of cervical muscles that control both head and neck posture between asymptomatic women with and without FHP.
MethodsSeventy asymptomatic women aged between 20 and 40 years, with and without FHP (35 in each group), participated in the study. The thickness of the cervical muscles (rectus capitis posterior – RCP, oblique capitis superior – OCS, semispinalis capitis – SSC, sternocleidomastoid – SCM, and longus coli – LCo) was measured using RUSI and the data was compared between the two groups.
ResultsThe comparison of cervical muscle thickness between women with and without FHP revealed significant difference only with regard to the muscle thickness of the SCM muscle (mean difference: 0.7mm, 95% confidence interval of the difference: 0.14, 1.26mm, p value: 0.014). The thickness of this muscle was greater in women with FHP.
ConclusionTonic contraction of the SCM muscle can lead to greater thickness of this muscle in subjects with FHP.
Forward head posture (FHP) is defined as a forward projection of the head relative to the trunk in the sagittal plane.1 Prolonged sitting position in front of computers, for example, can lead to this poor posture.2 FHP is one of the most prevalent abnormal postures in patients with neck disorders.3 This poor posture has been linked to many musculoskeletal disorders such as headache, shoulder pain, neck pain, craniofacial pain, and temporomandibular disorders.4–7 Previous studies have demonstrated a correlation between FHP and disability in patients with neck disorders.8 Increase in the time spent working on a computer in sitting positions has increased the prevalence of this poor posture.
The main function of the cervical spine is to orient the head against the force of gravity.9 Some cervical muscles such as the longus colli (LCo), sternocleidomastoid (SCM), semispinalis capitis (SSC), rectus capitis posterior (RCP), and oblique capitis superior (OCS) are important muscles to control the posture of the head and neck.8,10,11 Biomechanical changes in FHP induce extra flexor torque and permanent contraction of the dorsal cervical muscles.12 These biomechanical changes may result in thickness changes in cervical muscles and disrupt their function.
Evaluation of muscle thickness can indicate muscle function and strength.13 Magnetic Resonance Imaging (MRI), Computed Tomography (CT) scan, and Rehabilitative Ultrasound Imaging (RUSI) are common methods which are used to measure muscle thickness. Nevertheless, MRIs and CT scans are expensive and the CT scan entails X-ray radiation, while RUSI is considered an accessible, cost effective, and reliable method of evaluation of muscle thickness.14
Although some previous studies have evaluated cervical muscle thickness in participants with FHP, to the best of our knowledge, no previous studies have compared the thickness of all cervical muscles controlling head and neck posture between participants with and without FHP. Therefore, we aimed to compare the thickness of these muscles in women with and without FHP. This study can promote a better understanding of the changes in thickness of these muscles in participants with FHP.
MethodsParticipantsSeventy asymptomatic women, aged between 20 and 40 years, participated in the present study. Participants were assigned into two groups (with and without FHP, 35 in each group) according to the craniovertebral angle (CVA) measured by photographic images.
The inclusion criteria for both groups were female participants aged between 20 and 40 years. Participants with a CVA greater than 48° were included in the group without FHP and participants with a CVA less than 48° were included in the group with FHP.5 The exclusion criteria for both groups were as follows: neck or shoulder pain, radicular pain of the upper extremity, history of cervical surgery, severe thoracic kyphosis, history of musculoskeletal or neuromuscular diseases, history of neck and shoulder pain in the previous 6 months, previous or current injuries of the neck/shoulder area, history of facial surgery or trauma, participation in sports activities, any hearing impairment requiring the use of a hearing aid, recurrent middle ear infections in the previous 5 years, persistent respiratory difficulties over the last 5 years that interfered with daily activities, any visual impairment not corrected by glasses, central nervous system disorders, and temporomandibular disorders.1
ProceduresEvaluation of CVAAt the onset of the study, the aims and procedures of the study were explained to the participants and they were asked to sign an informed consent form prior to data collection. The study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran (SBMU.REC.2015.529, 1/4/2015).
After collecting demographic information, a digital camera (Sony, DSC WX80, Japan) was used to measure head and neck postures in a standing position. The camera was placed at a specified area at a distance of 1.5m from the participant on a fixed base and its height was adjusted to the level of the participant's shoulder.5 The participant was instructed to stand in a natural standing position she felt comfortable with and to distribute her body weight evenly between her feet, maintaining that position throughout the assessment.1
To standardize the participant's head and neck posture, a self-balanced position procedure was followed. The participant was asked to move her head and neck into full flexion and extension and reduce the range of motion gradually to stop movement and keep the head and neck in their habitual posture.5
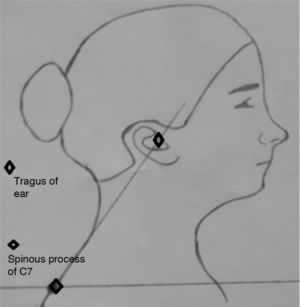
To measure the CVA, the examiner marked the C7 spinous process as well as the tragus of the ear. Three pictures of the lateral view of the two sides of the participants were taken. Images were transferred to computer and Image J software was used to measure the CVA (Fig. 1).15
The CVA was measured between a horizontal line passing through the C7 spinous process and a line connecting the C7 to the tragus of the ear.5 If the average CVA calculated from the two sides was less than 48°, the participants were considered to have FHP.5 There is no clear cut-off value for the CVA to identify the presence of FHP. Since many of the previous studies consider the CVA less than 48–50° as FHP, we considered CVAs less than 48° as FHP in the present study.5
Ultrasound imagingIn the present study, attempts were made to measure the thickness of the RCP, OCS, SSC, SCM, and LCo muscles. Images of the cervical muscles were taken using a RUSI device (Ultrasonic scanner, HS 2100, Honda Electronic Co., Japan) with a 7cm linear probe in B-mode (7.5MHz). The examiner was a Ph.D. candidate in physical therapy trained for 1 year by a musculoskeletal ultrasonography researcher.
The seated position was maintained for visualization of the cervical muscles using RUSI. The participants were asked to sit in the relaxed state on a chair, keep their knees and hips at 90° of flexion, and maintain their head and neck in the neutral position. Participants were asked to keep their upper arms in the resting position by their sides, forearms and hands on the thigh. Because any change in position would change muscle thickness, the participant's position was checked during ultrasonography.
To obtain images of the RCP, OCS, and SSC muscles using RUSI, the examiner placed the probe transversely on the C2 spinous process. Next, the examiner moved the probe laterally to identify the lamina of the C2 and vertically to identify the C1 lamina. To identify the RCP muscle, the examiner moved the probe upward or downward. For visualization of the OCS muscle, the examiner moved the probe further laterally at the same level as used for measuring the RCP. At this level, the image of the SSC muscle was also obtained (Fig. 2).16
To visualize the LCo muscle using RUSI, the probe was placed transversely at the C6 level. The reason for using this level was the fact that it has no overlap between the LCo and the longus capitis muscle.17 In order to obtain the images of the SCM muscle at this level, the examiner placed the probe transversely on the SCM muscle between its origin and insertion (Fig. 3).
To obtain each image, the probe was removed and repositioned at the same level. Three images of each muscle were frozen and stored for future analysis. All participants were right-handed and images of the cervical muscles were taken only on their right side. The thickness of the aforementioned muscles was measured using RUSI on each image. We did not include the facial outline to measure the thickness of the muscles and placed the cursor on the inside edge of the superior fascia at the thickest portion of the muscle, drawing a vertical line to the inside edge of the inferior fascia.18 The average thickness value of the three ultrasound images was used for the statistical analysis.
It should be mentioned that prior to the main study, the reliability of RUSI for measuring the thickness of the aforementioned muscles was evaluated and the results showed that RUSI is a reliable method (Intraclass Correlation Coefficient >0.8 for all muscles).
Statistical proceduresData were analyzed using SPSS version 16. The normality of the variables was verified using the Shapiro–Wilk test. The results showed normal distribution for thickness of all muscles except for the RC muscle. The Mann–Whitney U test was used to compare the RC thickness between groups. The thickness of the other muscles was compared between the two groups using the independent-samples t test. The level of significance was set as p<0.05.
ResultsTable 1 includes the demographic characteristics and the CVA of the participants. A summary of the results of cervical muscle thickness in women with and without FHP is shown in Table 2. Cervical muscle thickness was greater in women with FHP than in the control group, except for the LCo muscle which was greater in the control group than in the FHP group (7.6mm in control group vs 7.4mm in FHP group). The results of the present study demonstrated that only the thickness of the SCM was significantly different between the two groups, with greater SCM thickness in the FHP group than in the control group (8.7mm in FHP group vs 8.05mm in control group) (p=0.014).
Mean (SD) of demographic characteristics and CVA of the participants (n=35 in each group).
| Variable | Control group | FHP group |
|---|---|---|
| Age (year) | 25.18 (5.52) | 24.94 (5.13) |
| Height (m) | 1.63 (0.04) | 1.63 (0.06) |
| Weight (kg) | 60.72 (10.09) | 60.17 (9.35) |
| BMI (kg/m2) | 22.81 (3.7) | 22.6 (3.59) |
| CVA | 54.26° (1.88) | 43.76° (1.55) |
FHP, forward head posture; BMI, body mass index; CVA, craniovertebral angle; SD, standard deviation.
Mean (SD) of cervical muscle thickness in women with and without FHP (n=35 in each group).
| Muscle | Group | Muscle thickness (mm) | 95% confidence interval of the difference (mm) | p value |
|---|---|---|---|---|
| RCP | Control | 4.03 (0.59) | (−0.03, 0.64) | 0.07 |
| FHP | 4.3 (0.81) | |||
| OCS | Control | 6.96 (0.57) | (−0.19, 0.34) | 0.58 |
| FHP | 7.03 (0.56) | |||
| SSC | Control | 8.01 (0.8) | (−0.34, 0.38) | 0.9 |
| FHP | 8.03 (0.71) | |||
| SCM | Control | 8.05 (1.02) | (0.14, 1.26) | 0.01 |
| FHP | 8.7 (1.3) | |||
| LCo | Control | 7.6 (0.9) | (−0.66, 0.34) | 0.53 |
| FHP | 7.4 (1.1) | |||
SD, standard deviation; FHP, forward head posture; RCP, rectus capitis posterior; OCS, oblique capitis superior; SSC, semispinalis capitis; SCM, sternocleidomastoid; LCo, longus coli.
The aim of the present study was to clarify whether there is significant a difference in terms of cervical muscle thickness between women with and without FHP. The results of our study demonstrated a statistically significant difference in muscle thickness only for the SCM muscle between women with FHP and controls, with a greater thickness in the participants with FHP. The mean difference in SCM thickness between two groups was greater than the standard error of measurement of this muscle (0.7mm vs 0.33mm) and it revealed a clinically significant difference between the two groups.
The greater thickness of the SCM muscle can be attributed to disuse of the deep cervical flexor (DCF) muscles, dominance of the superficial neck flexors (such as the SCM muscle) in neck flexion movements, tonic contraction of the SCM muscle, sustained neck flexion movements, and shortening of this muscle. In addition, structural changes in this muscle, such as fatty infiltration, may also be possible reasons for greater thickness of this muscle in women with FHP.
The greater thickness of the SSC muscle in participants with FHP, compared to controls, can be attributed to the greater stress on the dorsal cervical muscles in FHP, however this difference was not observed to be significant. This insignificant difference was consistent with the results reported by Goodarzi et al.2 They compared the thickness of the cervical extensor muscles (multifidus, semispinalis cervicis, SSC, splenius capitis, and upper trapezius) between participants with and without FHP at the level of the fourth cervical vertebra. The results of their study showed no significant differences regarding the thickness of the cervical extensor muscles between the two groups.2
In the present study, the thickness of the RCP and OCS muscles was greater in participants with FHP compared to the controls, yet this difference was not significant. This difference may be attributed to the fact that, in our study, participants with FHP had a moderate degree of FHP (mean CVA: 43.76°) and the shortening of these muscles may be a late consequence of FHP to keep a neutral visual line. Furthermore, a significant difference in the thickness for these muscles may be apparent in subjects with chronic or severe degree of FHP.
In the current study, no significant difference was observed regarding LCo thickness between the two groups. The smaller thickness of the LCo muscle in women with FHP was consistent with the findings reported by Ishida et al.,6 who measured the CVA and DCF thickness in healthy men. The results indicated that men with smaller CVAs had smaller DCF muscle thickness. Smaller LCo thickness in women with FHP may be the result of disuse of the DCF muscles in the sitting posture in daily activities with the head translated forward.8
Jung et al.19 compared the effects of the initial head position on the thickness of the deep and superficial neck flexor muscles during craniocervical flexion (CCF) in participants with and without FHP. The participants performed CCF in two head positions: horizontal head position (HHP) and relaxed head position (RHP). The results of their study indicated a significant difference in the thickness of the SCM muscle between two groups (with and without FHP). Thickness increased significantly during CCF in the HHP in the participants with FHP compared to those without FHP. The change in the thickness of the SCM was not significantly different between two positions in the participants without FHP. Additionally, there was no significant change in the thickness of the LCo muscle during the CCF according to the initial position in both groups.
It should also be mentioned that, although the current study was one of the first studies to compare cervical muscle thickness between women with and without FHP, it has some limitations which should be taken into account when generalizing the findings. First, our study was conducted only on asymptomatic women with a moderate degree of FHP; therefore, the results cannot be generalized to symptomatic women or women with severe FHP. In addition, only female participants were included in the present study, therefore the results may not be generalizable to men with FHP. We suggest an evaluation of muscle thickness at other levels of the cervical spine to better understand thickness changes of the cervical muscles in participants with FHP.
In conclusion, the results of the present study only showed a significant difference in SCM muscle thickness between women with and without FHP. This significant difference can be the result of insufficient activity of the DCF muscles, tonic contraction of the SCM, muscle shortening, or fatty infiltration of this muscle.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank the participants of the study for their helpful contribution.