Sacroiliac joint manipulation can alter joint and muscle control mechanisms through local and remote effects. Postural balance is controlled by supraspinal (rambling) and spinal–peripheral (trembling) mechanisms. A manipulation may interfere with postural control in quiet standing.
ObjectivesTo evaluate the immediate effects of sacroiliac joint manipulation on postural control in patients with (1) sacroiliac dysfunction and (2) to determine whether rambling and trembling are affected by sacroiliac joint manipulation.
Methods32 patients aged between 20 and 50 years old were selected by convenience after confirmation of sacroiliac joint dysfunction by clinical examination. These patients were randomly allocated either to manipulation or sham manipulation group. Displacement, velocity and frequency of the center of pressure, rambling and trembling in the anterior–posterior and medial–lateral directions were our primary outcomes and analyzed immediately before and after the intervention in quiet standing. The physical therapists who performed the physical, biomechanical and statistical examinations, were all blinded to the patients’ grouping.
ResultsNo differences were found between the two groups but trembling velocity (0.14 and −0.11 for intervention and sham group, respectively) and frequency (0.17 and 0.11 for intervention and sham group respectively) increased after intervention in the treatment group in the anterior–posterior direction.
ConclusionGenerally, sacroiliac joint manipulation had no superiority than sham treatment regarding postural control as measured by rambling–trembling analysis of center of pressure. Manipulation may increase muscle activation in the treatment group due to increased trembling parameters.
Trial number: IRCT2014072715932N8 – http://www.irct.ir/searchresult.php?keyword=%D8%B3%D9%88%DB%8C%D9%87&id=15932&field=#ber=8≺t=13&total=10&m=1.
Sacroiliac (SI) joint dysfunction is considered one of the possible sources of chronic mechanical low back pain.1 Stability of the SI joint is provided by the surrounding muscles, ligaments and the unique shape of the joint.2 The SI joints play an important role in force transmission between the trunk and lower extremities, so any dysfunction in these joints may alter weight distribution at the feet.3 Anker et al.4 showed that greater weight-bearing asymmetry may lead to increased postural instability. Baruah et al.5 showed that patients with SI joint dysfunction had deficits in balance and postural control. It has been reported that SI joint manipulation can decrease pain, redistribute peak pressure between the feet,3 and improve disability6 and gait symmetry7 in patients with SI dysfunction.
The effects of SI manipulation have been proposed to be related to spinal and supraspinal mechanisms.8 Research published to date, however, is controversial regarding the spinal mechanisms of SI manipulation. In some studies, SI manipulation increased muscle activity9–11 whereas in others, it decreased alpha motor neuron activity12 or had no effect at all.13 Few studies have evaluated supraspinal and cortical mechanisms in spinal manipulation. Alterations in excitability and metabolism after spinal manipulation have been reported in corticospinal tracts, limbic, cerebellar and sensorimotor areas.12,14,15
In patients with low back pain, center of pressure (CoP) parameters have been used conventionally to evaluate postural control.16,17 Rambling (Rm) and trembling (Tr) have been shown to be more sensitive parameters for analyzing postural control during quiet standing.18,19 According to the main hypothesis of the rambling–trembling process, the higher spinal centers control the CoP at instant equilibrium points. The net effect of external torques acting on the body is equal to zero at these points, and the CoP coincides with the gravity line extending from the body's center of mass. Rambling component is composed of interpolation of these points. If the body loses the equilibrium state, restoring forces try to return it to an upright stance.20 Trembling is therefore viewed as oscillation of the CoP around the equilibrium points, which can be calculated as the differences between CoP and rambling.21,22 Therefore, any modulation in muscle responses or spinal reflexes may change trembling.
It has been claimed that rambling represents supraspinal processes whereas trembling reflects spinal reflexes and mechanical properties of the muscles and joints.23,24 Research into rambling and trembling can distinguish different spinal and supraspinal mechanisms behind postural control,25 as shown in a number of studies. Freitas et al.26 evaluated the effect of joint immobilization on postural control, and found increased anterior–posterior (AP) and decreased medial–lateral (ML) trembling displacement and velocity in quiet standing with various lower extremity constraints. They proposed that body sway was controlled by two distinct neuromuscular mechanisms involving ankle and hip strategies.26 Solnik et al.27 evaluated postural sway in different pointing tasks and found that rambling and trembling components of postural sway involved different neurophysiological mechanisms. VanderHill et al.28 evaluated the flexibility of the central nervous system in performing different dual task activities, and found that a suprapostural task altered velocities of rambling, trembling and CoP in both AP and ML directions. Rambling and trembling can also reveal adaptive changes in the sensory system over time. For example, whole body vibration has been found to change Rm-Tr paths of body sway in long-term evaluations.18 Another study by Sarabon et al.29 showed that aging had a strong effect on rambling parameters. These studies showed that the evaluation of postural control by studying rambling and trembling could shed light on new aspects of postural balance that conventional analysis of CoP was unable to detect.
Although research to date has evaluated different neurophysiological aspects of SI joint manipulation, there is no evidence to date of a definite effect of spinal manipulation on postural control by supraspinal and spinal mechanisms. The aim of this clinical trial was to evaluate the effect of SI joint manipulation on balance in patients with SI joint dysfunction. Based on previous studies, our first hypothesis was that SI joint manipulation would change balance parameters in quiet standing. Our second hypothesis was that SI joint manipulation would have a stronger effect on trembling than on rambling.
MethodsParticipantsFor this 2-arm double blinded randomized clinical trial, 78 male and female patients (age range: 20–50 years old) were initially recruited. The patients had lower back pain of 3 months’ duration, and were recruited from rehabilitation clinics affiliated with Shiraz University of Medical Sciences, Shiraz, Iran. They entered the study if they had a Numeral Rating Scale score of 6 or lower and an Oswestry Disability Index of 20–4030 with no history of treatment during the previous 6 months. Patients were excluded if they had any history of spinal surgery, hip pathology, vestibular pathology, arthritis, or neurological central nervous system pathology. Sacroiliac dysfunction was verified by the patient's history and physical examination. The patient's history consisted of pain location, pain with postures/activities that might stress the SI joint (e.g. turning in bed, getting out of the bed, stepping up with the affected leg, standing from sitting) and any direct/indirect trauma to SI joint (e.g. stepping of a curb, fall on buttocks, strain and twisting maneuvers).31 For the physical examination, an expert physical therapist evaluated all patients. The presence of SI joint dysfunction was confirmed by a group of different tests (i.e. Yeoman's test, Gaenslen's sign, the FABER test, the compression test and thigh thrust) with high reliability and validity.32–36 If at least 3 of the tests were positive, then the patient was entered into the study6 after he or she signed an informed consent form developed by the Medical Ethics Committee of Shiraz University of Medical Sciences, Shiraz, Iran (approval number CT_P_91_4512). This trial was prospectively registered at www.irct.ir, trial registration number # IRCT2014072715932N8.
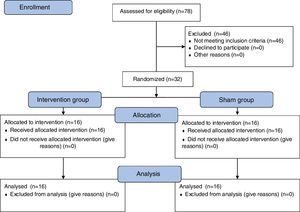
Based on work by Byl and Sinnott37 and considering a 4-mm between-group difference and SD=3.1, sample size was calculated as 14 patients in each group for 90% statistical power and an alpha error of 0.05. A convenience sample of 32 patients (17 women and 15 men) were entered in the study. They were assigned to one of two groups of 16 patients (i.e. intervention or sham group) with computerized blocked randomization using the Randomizer program.38 Allocation was concealed as the Randomizer program performed the randomization. Patients were not aware of the other group. Male/female ratio in the intervention and sham group was 8/8 and 7/9 respectively. The CONSORT flowchart (Fig. 1) summarizes information about the study population, sample and analysis. All procedures were conducted according to the Declaration of Helsinki.
ProcedureIn the pre-intervention phase, patients stood barefoot on a force platform with their eyes open for 3 trials of 30s in an upright quiet stance. To eliminate bias, another therapist who was an expert in the field of biomechanics measured balance and analyzed the data without the knowledge of patients’ grouping. Center of pressure parameters along with force data were recorded during quiet standing on a Kistler 400mm×600mm force platform (Kistler 9286 A, Kistler Co, Winterthur, Switzerland). The system was calibrated before data capture based on standard instructions from the manufacturer, using a Cartesian x–y–z coordinate system. Signals were acquired at a sampling rate of 120Hz with Qualisys Tracking Manager software (version 2.0.325 (Qualisys Inc., Göteborg, Sweden), and the data were analyzed with custom-made software developed in LabVIEW 2011 (National Instruments Co., Austin, TX, USA)). Pre-processing consisted of two separate filters of the acquired signals, one for net horizontal force signals (10Hz low-pass second-order Butterworth) and another for the two components of CoP projection (0.04–10Hz band-pass second-order Butterworth). The two components of CoP (AP and ML) in rambling and trembling were decomposed according to Zatsiorsky and Duarte.22
Then in the intervention group, a high-velocity, low-amplitude thrust was applied to the affected SI joint by an expert physical therapist. The patient lay supine and the therapist stood contralateral to the manipulation side. The patient passively curled toward the side to be manipulated, with his or her fingers locked behind the head. Then the therapist rotated the patient toward himself and applied a quick thrust to the anterior superior iliac spine in a posterior and inferior direction on the affected side. The technique was repeated up to 3 times if no audible pop was heard.6 Patients in the control group (i.e. sham treatment) were positioned similar to the treatment group but no thrust force was applied. The duration of the real or sham manipulation was equal in both groups. The therapist who performed the manipulation was the one who physically assessed patients during the examination process. In the post-manipulation phase, CoP was measured the same way as in the pre-intervention phase.
Outcome measuresRambling and trembling were quantified with parameters used previously in other studies and were our primary outcomes: mean velocity, amplitude as the root mean square, and mean frequency. All evaluations were performed at the Center for Human Motion Science Research of Shiraz University of Medical Sciences.
Statistical analysesData was analyzed based on the fact that all subjects received the treatment or sham condition as planned (intention to treatment approach). Statistical analyses were performed using SPSS version 18 software (SPSS Inc., Chicago, IL, USA). The Shapiro–Wilk test was used to test the normal distribution of the variables measured, and a log-transformation test was used to correct non-normally distributed variables. An independent-sample t-test was used to identify differences before and after treatments. Analysis of variance was used to identify variations between the two groups, and between the two trials within each group. Higher values of F indicated a greater likelihood of statistically significant differences between the groups. Bonferroni correction was used to adjust for potential alpha value inflation. The level of statistical significance was set at p<0.05.
ResultsThe patients’ anthropometric characteristics, mean of pre-test and post-test differences are shown in Table 1, and the results of descriptive statistics are summarized in Table 2. No significant differences in the ML direction were found. Time, group and interaction effects in the AP direction were found and are summarized below.
Summary of participants’ baseline characteristics in the 2 groups of patients.
| Variable | Manipulation group (n=16 patients) Mean (SD) | Sham (n=16 patients) group Mean (SD) |
|---|---|---|
| Age (years) | 23.44 (9.00) | 24.19 (15.12) |
| Weight (kg) | 62.11 (78.88) | 62.28 (53.40) |
| Height (cm) | 170.00 (40.00) | 171.06 (40.00) |
| Oswestry Disability Index | 30.00 (5.00) | 30.00 (4.00) |
| Numeral Rating Scale | 3.00 (0.00) | 3.00 (1.00) |
Results of within and between-group comparisons for all outcome measures in the 2 groups of patients.
| Intervention group | Sham group | Adjusted mean difference | 95% CI | p | |||
|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||||
| ML | |||||||
| CoPF (Hz) | 0.29 (0.08) | 0.26 (0.10) | 0.31 (0.07) | 0.30 (0.07) | 0.03 | −0.08 to 0.01 | 0.14 |
| RmF (Hz) | 0.20 (0.04) | 0.18 (0.06) | 0.20 (0.05) | 0.18 (0.05) | 0.01 | −0.02 to 0.02 | 0.79 |
| TrF (Hz) | 0.57 (0.25) | 0.59 (0.20) | 0.54 (0.17) | 0.49 (0.19) | −0.08 | −0.05 to 0.19 | 0.27 |
| CoPRMS (mm) | 1.15 (0.33) | 1.30 (0.38) | 1.48 (0.74) | 1.38 (0.57) | −0.03 | −0.51 to 0.11 | 0.20 |
| RmRMS (mm) | 1.17 (0.47) | 1.32 (0.50) | 1.49 (0.84) | 1.37 (0.47) | −0.03 | −0.53 to 0.16 | 0.29 |
| TrRMS (mm) | 0.71 (0.38) | 0.70 (0.42) | 0.96 (0.69) | 0.91 (0.36) | 0.16 | −0.51 to 0.05 | 0.08 |
| CoPV (mm/s) | 2.54 (0.66) | 2.49 (0.68) | 2.90 (0.81) | 2.94 (0.96) | 0.13 | −0.94 to 0.13 | 0.13 |
| RmV (mm/s) | 1.35 (0.42) | 1.27 (0.32) | 1.48 (0.46) | 1.36 (0.54) | 0.00 | −0.40 to 0.18 | 0.47 |
| TrV (mm/s) | 2.16 (0.58) | 2.10 (0.57) | 2.43 (0.71) | 2.50 (0.77) | 0.17 | −0.78 to 0.11 | 0.19 |
| AP | |||||||
| CoPF (Hz) | 0.22 (0.05) | 0.24 (0.07) | 0.23 (0.06) | 0.23 (0.05) | 0.01 | −0.04 to 0.03 | 0.84 |
| RmF (Hz) | 0.17 (0.04) | 0.18 (0.05) | 0.17 (0.04) | 0.18 (0.04) | 0.10 | −0.02 to 0.02 | 0.93 |
| TrF (Hz)** | 0.87 (0.32) | 1.04 (0.39) | 0.62 (0.20) | 0.73 (0.34) | 0.23 | 0.07 to 0.48 | 0.00** |
| CoPRMS (mm) | 2.73 (1.17) | 2.95 (2.22) | 2.75 (1.09) | 2.87 (1.02) | 0.05 | −0.94 to 1.01 | 0.80 |
| RmRMS (mm) | 2.68 (1.26) | 2.87 (2.08) | 2.63 (0.91) | 2.71 (0.98) | 0.03 | −0.82 to 1.03 | 0.92 |
| TrRMS (mm) | 0.97 (0.64) | 0.89 (0.48) | 1.29 (0.84) | 1.08 (0.59) | 0.17 | −0.67 to 0.15 | 0.19 |
| CoPV (mm/s) | 5.59 (1.11) | 5.83 (1.19) | 5.17 (1.53) | 5.10 (1.15) | −0.17 | −0.26 to 1.41 | 0.13 |
| RmV (mm/s) | 2.62 (0.52) | 2.83 (0.91) | 2.47 (1.03) | 2.71 (0.71) | 0.08 | −0.38 to 0.65 | 0.43 |
| TrV (mm/s)* | 4.96 (1.22) | 5.10 (1.03) | 4.29 (1.14) | 4.18 (1.06) | 0.15 | 0.03 to 1.55 | 0.03* |
ML, medial–lateral direction; AP, anterior–posterior direction; Rm, Rambling; Tr, Trembling; V, mean velocity; RMS, amplitude; F, mean frequency; Pre, pre-intervention measurements; Post, post-intervention measurements.
Root Mean Square (RMS) of the variables of CoP were on average higher for AP than for ML (CoP: 2.83 vs. 1.33mm, Rm: 2.72 vs. 1.34mm; Tr: 1.06 vs. 0.82mm). Similarly, mean velocities were on average higher for AP than for ML (CoP: 5.42 vs. 2.72mm/s, Rm: 2.66 vs. 1.37mm/s; Tr: 4.63 vs. 2.30mm/s). Mean frequencies were similar for AP and ML (CoP: 0.23 vs. 0.29Hz; Rm: 0.18 vs. 0.19Hz; Tr: 0.82 vs. 0.55Hz).
No interaction effects (group×time) were detected for any of the parameters (p>0.05). Statistically significant within group differences were detected only in the treatment group for trembling frequency (F(1,30)=7.87, p<0.01, η2=0.208) and velocity in the AP direction (F(1,30)=4.90, p<0.05, η2=0.140) (Fig. 2) (Table 2).
DiscussionThe aim of this study was to evaluate the effect of SI joint manipulation on rambling and trembling parameters of CoP during quiet standing in patients with SI dysfunction. Our results indicated that generally sacroiliac joint manipulation was not superior to sham treatment regarding postural control.
Because of the nature of trembling, which originates from the moment of the ankle joint,21,22 the inverted pendulum theory appears to offer useful avenues to explain alterations in the trembling component in this study. When the ankle strategy is used, movements upon a wide base of support are compensated by muscles around the ankle joint, especially in the sagittal plane. Our findings showed that SI joint manipulation mainly affects body sway parameters in the AP direction. Because the evaluation was performed in quiet standing (i.e. not on a narrow base of support or with external perturbations), we observed no hip strategy mechanism was observed based on load–unload mechanisms26 (i.e. no changes in the ML variables) after SI joint manipulation.
Previous studies have shown that patients with SI joint dysfunction have deficits in balance control,5 and that altered muscle control is an important factor in balance deficits.8,39 Spinal manipulation has reported to change both peripheral control mechanisms (i.e. somatosomatic (muscle) reflexes and central information processing).22 Previous studies have shown altered muscle activity in multiple muscles (e.g. multifidus, quadratus lumborum, gluteals) following manipulation.9 Higher trembling velocities are associated with increased muscle activity.40 Therefore, significantly higher trembling frequency and velocity may be a result of a change in the CoP by muscle activation due to manipulation. Although no previous studies were found that were directly comparable to the present report, our findings are consistent with the results of Freitas et al.26 and Solnik et al.,27 who inferred that increased trembling velocity in the AP direction may be due to increased muscle contraction. The increase in trembling frequency and velocity supports our suggestion that trembling may be a result of spinal reflexes and/or the intrinsic properties of muscles.
Rambling parameters did not change after SI joint manipulation in our manipulation participants. One explanation is that whole-body movements occur according to predetermined controlling schemes containing orders for muscle and joint positions. These schemes may change in response to peripheral conditions.28 Earlier studies reported some alterations in the central processing of sensory information with spinal manipulation.22 However, these alterations appear not to change the main balance controlling scheme from upper centers. No changes in CoP parameters were found in any direction after SI manipulation. This finding may arise as a result of shifting CoP along the rambling trajectory.22 In other words, our study showed that the upright standing control strategy may not change with SI joint manipulation, because neither the trajectory nor the velocity of the equilibrium points changed. As manipulation does not change equilibrium points (Rm), it had no adverse effect on balance. On the other hand, short time effects of muscle activation with manipulation could be the first step for clinical improvement of muscles function related to SI joint dysfunction. Neuromuscular training programs used after manipulation may continue muscle activation over time and could be used as part of a treatment program as previous studies supported this treatment over exercise alone in neck pain patients.41 This combination may produce greater short-term effect and long-term changes.
Our study had some limitations. Injection in the SI joint is the gold standard method to evaluate SI dysfunction. The main limitation of this study was that most patients declined SI joint injection. To resolve this issue, we used a group of 5 different tests with high reliability and validity rates.32–36 Another limitation of this study is that we did not measure pain and function after intervention. Although all of the patients reported pain reduction after manipulation, we did not record the pain level. Challenging conditions (i.e. sensory and motor challenges) were not evaluated, because they might have affected the results of the study.
Future studies should investigate the long-term effects of SI joint manipulation with a follow-up (longitudinal) design. Also, pain measurement after manipulation may reveal additional aspects of postural control that are of clinical importance. In addition, sensory challenges such as performing the balance tasks with eyes closed or while standing on a foam-lined mat would yield more information about the effect of manipulation on postural control mechanisms.
Generally sacroiliac joint manipulation had no superiority to sham treatment in terms of postural control. Manipulation may increase muscle activation in the treatment group due to increased trembling parameters.
Conflicts of interestThe authors declare no conflicts of interest.
We thank K. Shashok (AuthorAID in the Eastern Mediterranean) for improving the use of English in the manuscript.