Many studies have investigated the relationship between soft tissue tightness and shoulder kinematics. However, there is a lack of information on the dynamic properties responsible for side-to-side differences such as scapular asymmetry.
ObjectiveTo determine the relationship between a deficit in soft tissue flexibility and scapular asymmetry.
MethodsA total of 58 individuals (29 patients with shoulder pain and 29 asymptomatic participants) were enrolled. Bilateral shortening of the pectoralis minor muscle and posterior shoulder tightness were assessed. Additionally, side-to-side flexibility deficit was calculated. Scapular kinematics were measured with an electromagnetic tracking device while individuals were standing in a resting position and during arm elevation. The symmetry angle was calculated to quantify scapular asymmetry.
ResultsThe pectoralis minor and the posterior capsule flexibility deficit showed a significant positive relationship with the symmetry angle in the resting position separately for both asymptomatic (r=0.47, r=0.37 relatively) and symptomatic groups (r=0.58, r=0.38 relatively), indicating that the increased deficit in the pectoralis minor and posterior capsule flexibility were associated with increased scapular asymmetry. However, no significant relationship was found between flexibility deficit and scapular asymmetry during arm elevation and lowering for both asymptomatic and symptomatic groups.
ConclusionThe findings of the study provided information on the relationship of a flexibility deficit on the scapular position and orientation in asymptomatic and symptomatic populations.
It is widely accepted that the scapula plays an important role in providing mobility and stability for the shoulder joint complex.1,2 During shoulder elevation, the scapula moves through upward rotation, posterior tilt, and internal or external rotation.3 Abnormal movement alterations in these scapular movements are known as scapular dyskinesis.4 Kinematic alterations and side-to-side kinematic asymmetry in the shoulder complex across symptomatic and asymptomatic populations have been previously reported.5–8 Although there are several factors that might affect scapular kinematics, research till date has shown that pectoralis minor and posterior capsule tightness may be potential mechanisms for the development of kinematic alterations in the shoulder complex with movement dysfunctions, such as impingement symptoms.9
Borstad and Ludewig10 categorized healthy shoulders as having a short or long pectoralis minor resting length. They reported that tightness in the pectoralis minor muscle resulted in significantly less scapular posterior tilt and greater scapular internal rotation during arm elevation. Similarly, forward shoulder posture with the protraction of the scapula was also related to soft tissue tightness of the pectoralis minor muscle,11 which was regarded as a contributing factor to shoulder impingement.12
The posterior capsule of the glenohumeral joint has a complex structure,13 and its tightness has been associated with altered scapular kinematics.14 Borich et al.14 conducted a study on asymptomatic shoulders with posterior capsular tightness and reported that the posterior capsule tightness resulted in increased scapular anterior tilt when the humerus moved toward internal rotation. In a cadaveric study, Harryman et al.15 showed that the tightening of the posterior capsule also resulted in significant superior translation of the humerus on the glenoid.
A recent study has shown that both involved and non-involved shoulders have alterations in scapular kinematics in individuals with shoulder impingement.16 Additionally, these symptomatic individuals had increased scapular asymmetry when compared to asymptomatic individuals.16,17 Although there are many investigations conducted on the relationship between soft tissue tightness and shoulder kinematics, there is a lack of information concerning the dynamic properties responsible for side-to-side differences such as scapular asymmetry.10,14,15 It is not yet clear whether side-to-side pectoralis minor and posterior capsule flexibility deficits have an effect on the observed scapular asymmetry in asymptomatic and symptomatic individuals.
This study investigated the relationship between pectoralis minor and posterior capsule flexibility deficits and scapular asymmetry in the resting position and during arm elevation in asymptomatic and symptomatic individuals. We hypothesized that there would be a positive relationship between soft tissue flexibility deficits and scapular asymmetry.
MethodsA total of 58 individuals participated in the study, including both symptomatic individuals with unilateral shoulder pain in the dominant arm lasting more than six weeks (n=29) and asymptomatic individuals (n=29). Symptomatic individuals with unilateral shoulder pain were selected from a group of patients who were diagnosed with unilateral rotator cuff tendinopathy. The symptomatic individuals recruited for the current study met at least two of the following criteria: (1) painful arc during flexion or abduction, (2) a positive Neer18 or Hawkins-Kennedy test,19 and (3) painful resisted external rotation or painful Jobe's test.20 Asymptomatic individuals were selected among age-matched controls who had no history of shoulder pain or injury related to the upper extremities. They were included in the present study if they had 180° of shoulder flexion and abduction, 90° external rotation, and 70° internal rotation measured with a universal goniometer.21 We excluded participants if they regularly participate in any overhead sports and patients with a rotator cuff tear >5cm, a tendon tear in the long head of biceps, or degenerative joint disease based on magnetic resonance imaging or ultrasound findings. The Institutional Review Board (186-35, Hacettepe University, Ankara, Turkey) approved the protocol for this study, and all volunteers were informed about the nature of the study and signed a written consent form.
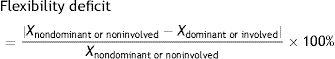
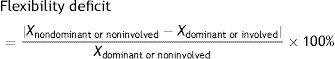
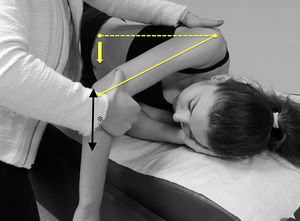
Bilateral indirect measurement of shortening of the pectoralis minor muscle was assessed using the pectoralis minor length test described by Lewis and Valentine22 [intraclass correlation coefficients (ICC) ranging from 0.90 to 0.97]. Posterior shoulder tightness was assessed using measurements suggested by Tyler et al.23 (ICC values ranging from 0.92 to 0.95). For the pectoralis minor length test (Fig. 1), the linear distance from the treatment table to the posterior aspect of the acromion was measured for each individual in a supine position.22 The posterior shoulder tightness measurement was made with each individual in a side-lying position (Fig. 2).23,24 During this measurement, the assessor first stabilized the scapula, and then the humerus was slowly lowered to a horizontally adducted position. The limit of posterior shoulder flexibility was considered as the onset of scapular movement or humerus rotation out of neutral. The distance from the treatment table to the medial epicondyle of the humerus was measured in centimeters. The side-to-side flexibility deficit for pectoralis minor and posterior capsule in percentages was further separately analyzed. To calculate the flexibility deficit, the following formula was used:
- (1)
If (Xnondominant or noninvolved>Xdominant or involved), the following equation was substituted:
- (2)
If (Xnondominant or noninvolved<Xdominant or involved), the following equation was substituted:
The lower value of flexibility deficit indicates less flexibility deficit for the related structure.
Three-dimensional kinematic data were collected bilaterally and simultaneously by the first author (E.T.) with a Flock of Birds electromagnetic tracking device (Ascension Technology Corporation, Shelburne, VT), interfaced with the Motion Monitor software program (Innovative Sports Training, Inc., Chicago, IL). For kinematic data recordings, five sensors were attached directly to the skin; the thoracic sensor was located over the T1 spinous process, the scapular sensors were applied over the flattest aspect of each acromion and the humeral sensors were applied over the posterior aspect of each arm.25 Individuals stood with their arms relaxed while specific bony landmarks were digitized.26 During recordings, firstly, all individuals were asked to maintain comfortable resting position for 5s. Secondly, all individuals were asked to perform bilateral, full arm elevation using two wooden poles as a guide for the scapular plane at a speed matching the beat of a metronome using 3s for elevation and 3s for lowering. Data on scapular orientation at rest and at 30°, 60°, 90°, and 120° of humerothoracic elevation and lowering were obtained. Scapular rotations were represented using the Y–X′–Z″ sequence, in which the first rotation defined the amount of the internal–external rotation, the second upward–downward rotation, and the last anterior–posterior tilt. Humeral rotations were represented using the Y–X′–Y″ sequence of humerothoracic elevation, in which the first rotation defined the plane of elevation, the second the amount of humerothoracic elevation, and the third the amount of axial rotation.
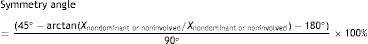
The method suggested by Zifchock et al.27 was used to define symmetry angle, to be able to quantify scapular asymmetry throughout arm elevation (at rest and at 30°, 60°, 90°, 120° of elevation, and at 120°, 90°, 60°, 30° of lowering) between involved and non-involved shoulders of the asymptomatic group or dominant and non-dominant shoulders of the asymptomatic group. The symmetry angle was calculated with the data obtained from each scapular kinematics variable identified previously at the same humerothoracic elevation angle by using the previously described formulae16,25:
- (1)
If (45°−arctan (Xnondominant or noninvolved/Xdominant or involved))<90°, the following equation was substituted:
- (2)
If (45°−arctan (Xnondominant or noninvolved/Xdominant or involved))>90°, the following equation was substituted:
Furthermore, the symmetry angle obtained through the scapular internal/external rotation, the upward/downward rotation, and the anterior/posterior tilt at the each specific humerothoracic elevation angle was then averaged. The symmetry angle value of 0% indicated perfect symmetry while 100% indicated that the two values were equal and opposite in magnitude.
Statistical analysisDescriptive statistics were reported as mean and standard deviation or counts and percentages. The baseline characteristics including flexibility deficit and scapular asymmetry were analyzed using a Student's t-test or Chi-square test. Statistical analysis of the relationship between scapular asymmetry and flexibility deficit was performed using a Spearman correlation coefficient (r) test separately for individuals with and without shoulder pain as the data was not normally distributed. The relationship was defined as positive or negative based on the value of r and classified as ‘strong’ (r>0.5), ‘medium’ (0.5≥r≥0.3), or ‘weak’ (r<0.3).28 Statistical significance was set to p<0.05. All analyses were performed using SPSS Statistics, version 21 (IBM Corporation, Armonk, NY).
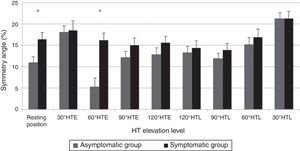
ResultsThe baseline characteristics of the asymptomatic and symptomatic groups are presented in Table 1. The mean pectoralis minor flexibility deficit was 11.06% [standard deviation (SD); 10.2%] for the asymptomatic group and 12.2% (SD; 8.9%; p=0.65) for the symptomatic group. Also, the mean posterior capsule flexibility deficit was 9.8% (SD; 9.4%) for the asymptomatic group and 16.5% (SD; 11.9%; p=0.02) for the symptomatic group. For both study groups, during shoulder elevation, the scapula moved toward internal rotation, upward rotation, and posterior tilt, and during shoulder lowering the scapula, moved toward external rotation, downward rotation, and anterior tilt. The symmetry angle ranged from 10.9% to 21.1% for the asymptomatic group and from 13.9% to 21.3% for the symptomatic group depending on humerothoracic elevation level (Fig. 3).
Characteristics of the asymptomatic and symptomatic shoulder groups.
| Asymptomatic group | Symptomatic group | p | |
|---|---|---|---|
| n=29 | n=29 | ||
| Age (years) | 26.1 (3.8) | 27.2 (6.4) | 0.42 |
| Body mass index (kg/m2) | 25.4 (2.7) | 23.6 (4.3) | 0.06 |
| Sex (n) | 11 female | 13 female | 0.78 |
| 18 male | 16 male |
Note: Data given as mean and standard deviation for age and body mass index.
Exact p-values are based on Student's t-test for age and body mass index, and Chi-square test for sex.
The pectoralis minor flexibility deficit had a significant positive relationship with the symmetry angle in the resting position for the asymptomatic group (r=0.47, p=0.008) and for the symptomatic group (r=0.58, p=0.001; Table 2). Similarly, the posterior capsule flexibility deficit had a significant positive correlation with the symmetry angle in the resting position for the asymptomatic group (r=0.37, p=0.04) and for the symptomatic group (r=0.38, p=0.03) (Table 2). However, there was no significant relationship between the soft tissue flexibility deficit and the scapular asymmetry during dynamic humeral elevation and lowering (p>0.05) (Table 2).
Correlation between flexibility deficit and symmetry angle for asymptomatic and symptomatic shoulder groups.
| Groups | Resting position | 30° HTE | 60° HTE | 90° HTE | 120° HTE | 120° HTL | 90° HTL | 60° HTL | 30° HTL |
|---|---|---|---|---|---|---|---|---|---|
| Asymptomatic group | |||||||||
| PM | |||||||||
| r | 0.47 | 0.08 | −0.26 | 0.18 | 0.25 | 0.25 | 0.12 | −0.12 | 0.21 |
| p | 0.008* | 0.6 | 0.1 | 0.3 | 0.1 | 0.1 | 0.5 | 0.5 | 0.2 |
| PC | |||||||||
| r | 0.37 | 0.27 | 0.16 | −0.007 | −0.007 | −0.03 | 0.2 | 0.3 | −0.1 |
| p | 0.04* | 0.1 | 0.4 | 0.9 | 0.9 | 0.8 | 0.1 | 0.1 | 0.8 |
| Symptomatic group | |||||||||
| PM | |||||||||
| r | 0.58 | −0.12 | −0.028 | −0.05 | −0.24 | −0.20 | −0.23 | −0.21 | 0.1 |
| p | .001* | 0.5 | 0.8 | 0.7 | 0.2 | 0.2 | 0.2 | 0.2 | 0.5 |
| PC | |||||||||
| r | 0.38 | 0.35 | 0.25 | 0.25 | −0.01 | −0.1 | 0.15 | −0.04 | 0.03 |
| p | 0.03* | 0.05 | 0.1 | 0.1 | 0.9 | 0.6 | 0.4 | 0.8 | 0.8 |
PM, pectoralis minor; PC, posterior capsule; HTE, humerothoracic elevation; HTL, humerothoracic lowering.
The current study investigated the relationship between a soft tissue (pectoralis minor) flexibility deficit and scapular asymmetry at rest and during arm elevation and depression. For asymptomatic and symptomatic shoulders, our findings showed that increased pectoralis minor and increased posterior capsule flexibility deficits were associated with increased scapular asymmetry while the arms were in a relaxed position. However, the soft tissue flexibility deficit did not reveal any relationship with the scapular symmetry during arm elevation or depression. Therefore, for both asymptomatic and symptomatic groups, the hypothesis of this study was only supported regarding the resting position.
The pectoralis minor muscle and the posterior capsule are anatomical structures directly attached to the scapula29; therefore, it was naturally expected that any tightness of these structures could affect the scapular position or orientation. Previous experimental studies reported the potential effect of tightness of these structures on scapular kinematics,10,14 and the current findings also separately showed the effect of tightness on scapular asymmetry for asymptomatic and symptomatic individuals. Although individuals with shoulder pain showed greater flexibility deficit in pectoralis minor and more scapular asymmetry when compared to asymptomatic controls, both groups demonstrated a certain amount of flexibility deficit and scapular asymmetry. Therefore, it was concluded that such variability in flexibility and posture may be normal.30
Interestingly, independent of shoulder pain, both asymptomatic and symptomatic groups revealed a relationship between soft tissue flexibility deficit and scapular asymmetry during static posture but not during dynamic movement. Therefore, factors such as pectoralis minor and posterior capsule tightness should be assessed and addressed in the clinical setting.31–35 These findings suggested that the presence of soft tissue flexibility deficit and scapular asymmetry might not be a relevant impairment for those with shoulder pain during activity. Dynamic movements require neuromuscular control and sensorimotor system integration to be able to correctly place the hand in the space.8,30 Therefore, neural control of the movement including motor unit recruitment properties, muscular activation levels, and timing may have an important role, and the static tension of the pectoralis minor and posterior capsule may have a relatively less important role during humeral elevation and depression.
Additionally, the assessment methods should be considered when interpreting our findings. In this study, tightness measurements were performed in a static position to assess a specific group of anatomical structures. Therefore, it is possible to observe the relationship between a flexibility deficit and scapular asymmetry while individuals are standing in resting position.
There are also some limitations of the current study. For the symptomatic group, the findings were obtained only from individuals with rotator cuff tendinopathy and subacute or chronic unilateral shoulder pain. Therefore, these findings do not represent other shoulder pathologies such as frozen shoulder or shoulder injuries in other populations such as those occurring in athletes in overhead sports. In this study, the 2 groups were comprised of individuals who did not regularly participate in any overhead sports. It is widely accepted that athletes in overhead sports demonstrate increased tension on the posterior shoulder because of high levels of eccentric muscular activity during the throwing.36,37 Therefore, further studies need to focus on different populations across various activity levels. Furthermore, the clinical methods for soft tissue flexibility examinations are always challenging because pectoralis minor tightness cannot be selectively isolated from the tightness of other structures attached to the corocoid process, such as the coracobrachialis or the short head of biceps. This is also true for the inability to isolate posterior capsule tightness from the tightness of the posterior rotator cuff and posterior deltoid muscles. In this study, an indirect measurement of pectoralis minor shortening was used that may have been influenced by posterior shoulder tightness in other structures. It must also be noted that posterior capsule tightness was measured using a horizontal adduction in side-lying position. Some previous studies have shown that this measurement seems to be more related to posterior muscles tightness.38–40 Therefore, the findings of this study should be cautiously interpreted owing to the lack of validation of the assessments used. Additionally, there is no widely accepted and validated definition of soft tissue tightness.
ConclusionsIn conclusion, shortening of the pectoralis minor muscle, posterior capsule flexibility deficit, and scapular asymmetry have been found in both asymptomatic individuals and individuals with shoulder pain. For asymptomatic and symptomatic groups, increased flexibility deficit of the pectoralis minor and the posterior capsule result in increased scapular asymmetry while arms are in a relaxed position. However, the soft tissue flexibility deficit did not influence scapular position and orientation during arm elevation or depression.
Conflicts of interestThe authors declare no conflicts of interest.