Educational programs designed for specific populations to improve regular physical activity need to be tested.
ObjectivesTo evaluate the effectiveness of an educational program, when compared to usual care, on improving physical activity 5 to 7 months after hospital discharge in adult patients undergoing their first percutaneous coronary intervention.
MethodsRandomized controlled trial with two groups: usual care (n = 56) and educational program (n = 53) interventions. Data on sociodemographic and clinical characteristics were collected and the Baecke-Habitual Physical Activity Questionnaire, Self-efficacy Scale for Physical Activity, and Hospital Anxiety and Depression Scale were administered at baseline and follow-up. Participants in the educational program received an intervention based on Social Cognitive Theory, focused on physical activity, followed by three telephone calls. The usual care group received the hospital routine information. Unadjusted and adjusted differences between the two groups in mean score changes (with 95% confidence intervals [CI]) were calculated for all outcomes.
ResultsAt follow-up, the educational program group showed higher mean ± standard deviation scores than the usual care group for practice of physical activity (7.94 ± 1.84 vs. 6.90 ± 1.89) and for self-efficacy (3.98 ± 3.75 vs. 2.52 ± 3.12). Adjusting for baseline outcome, the difference in mean change between groups was 0.89 (95% CI: 0.32, 1.46) for physical activity and 2.30 (95% CI: 1.12, 3.49) for self-efficacy. There were no statistical differences between groups in symptoms of anxiety and depression.
ConclusionThe educational program may be an effective intervention in increasing habitual physical activity and self-efficacy for physical activity in individuals with coronary artery disease.
The practice of regular physical activity contributes to primary and secondary prevention of cardiovascular diseases1–3 and should be encouraged. Researchers have found that the use of educational material with telephone follow-up increases the level of physical activity in people with coronary artery disease (CAD).4,5 E-health, delivered through the internet and related technologies, including telephone follow-ups, has been used by health professionals in the transition of patients from hospital to home care.6,7
In Brazil, there are barriers to access rehabilitation centers, such as long distances between home and place of care and/or lack of transportation.8–10 Also, there is lack of effective communication between healthcare services, resulting in failures to refer patients to rehabilitation programs.10,11 The limited availability of cardiac rehabilitation programs in public and private services also contributes to the absence or low referral rate for these programs.8 Telephones or other communication technologies could be used as strategies to overcome those barriers.6,12–15 While the access to the internet from computers or smartphone is not common among Brazilian older adults with low education and income, the use of messages by mobile and landline telephones is highly prevalent.16
Some authors successfully tested educational programs based on Social Cognitive Theory (SCT),17 using telephone text messaging18 or e-mail,19 in Brazilian populations. Strategies based on SCT that promote empowerment of individuals with CAD have been shown to improve the quality of life and the practice of physical activities, leading to changes in lifestyle and decreases in the number of hospital re-admissions.6 SCT postulates that individuals behave according to their interest in reaching their desired outcome. Self-efficacy, one of the main constructs of SCT, is defined as an individual's conviction to successfully perform the behavior necessary to produce a given result.16 The practice of physical activity might reflect the individual's confidence in the health benefits of this practice.
Although physical activity is recommended for secondary prevention, we found no published studies that tested a comprehensive educational program based on SCT, focusing on improving physical activity in Brazilians undergoing percutaneous coronary intervention (PCI), and that included face-to-face and telephone follow-ups. A clinical trial that compared the effects of a comprehensive cardiac rehabilitation with a physical activity-based rehabilitation program in Brazilian patients with CAD found significant improvement in functional capacity for the group that received the comprehensive approach.20 However, a recent review of cardiac rehabilitation programs in Brazil showed that there is limited availability of cardiac rehabilitation programs in public and private services and most of them are based solely on physical activity. In general, Brazilian cardiac rehabilitation programs have limited team of professionals (in terms of quantity and quality) and depend on scarce public resources.11 Therefore, there is a need to test innovative programs that can increase availability of cardiac rehabilitation programs without requiring high costs to the health system and to the patient.
The aim of this study was to evaluate the effectiveness of an educational program, which included general guidelines on cardiac rehabilitation with emphasis on physical activity and telephone follow-up to reinforce the guidelines (educational program group), compared to routine guidelines offered at hospital discharge (usual care group), in patients undergoing their first PCI. We expected that participants in the educational program group would have higher levels of habitual physical activity than the usual care group at the end of a period of five to seven months after hospital discharge (final follow-up). The secondary objectives were to compare the levels of self-efficacy for the practice of physical activity and the symptoms of anxiety and depression between the two groups, at the final follow-up.
MethodsStudy designThis study was a randomized controlled clinical trial, conducted in a public teaching hospital in Brazil. The study followed the protocol registered in the ClinicalTrials.gov and it was reported according to the Consolidated Standards of Reporting Trials.21
This study was approved by the Research Ethics Committee of the Universidade de São Paulo, Ribeirão Preto College of Nursing (Protocol 51805715.0.0000. 5393) and of the Ribeirão Preto Clinical Hospital (Protocol 51805715.0.3001.5440). All participants signed an informed consent before data collection.
ParticipantsAll individuals scheduled to receive their first PCI between July 17, 2017 and December 12, 2018 were invited to participate in the study. Inclusion criteria were: individuals 18 years or older, regardless of sex, undergoing their first PCI, and who had a fixed/mobile phone. Exclusion criteria were individuals: with prescription for restricted physical activity or presenting symptoms limiting/impeding performance of physical activities, reporting difficulty talking on the phone (such as hearing impairment), needing oxygen, having cognitive impairment, or already participating in a cardiac rehabilitation program or another intervention study. The cognitive status of the patient was evaluated in the waiting room, before the PCI, using the questions: current date, day of the week, place where the patient was, age, and place of birth. Individuals who answered more than two questions incorrectly were not enrolled in the study. Due to the logistics in the clinic, the individuals were randomized to one of the two interventions before the PCI. However, individuals whose PCI was subsequently cancelled or for whom the procedure was deemed by the medical team as a failure were excluded from further participation in the study, as they were not part of the population of interest.
Sample size calculation was based on the primary outcome of interest measured by the Baecke-Habitual Physical Activity Questionnaire (BHPAQ, described below), which was the only instrument validated for Brazilian Portuguese that measured the construct of interest at the time of the study. The minimal detectable change (MDC) and the minimal clinically important difference (MCID) of the BHPAQ have not been established, therefore, sample size was calculated based on a similar study in Brazilian patients with CAD treated in an outpatient clinic.13 In that study, at the end of two months, the BHPAQ mean ± standard deviation score was 7.2 ± 0.9 and 7.7 ± 0.8 for the usual care and educational program groups, respectively. Based on those results, we assumed that a difference of 0.5 points in the mean scores between groups would be a reasonable initial difference to test the effectiveness of the proposed intervention. The following parameters were used for sample size calculation: 0.80 power, 0.05 significance level, a difference of 0.50 points in the means of total BHPAQ score, standard deviation of 1.0 for both groups (based on mentioned study), and t-test for independent samples, resulting in 64 individuals in each group. With an estimated loss of participants throughout the study at 17% (based on similar study performed in this population14), we aimed to recruit 155 individuals. G*Power 3.1 was used for the calculations.
RandomizationUsing Statistical Package for the Social Sciences (SPSS) version 22.0, a research team member (not involved in data collection) generated the randomization list in blocks and inserted each assignment in opaque, sealed, and sequentially numbered envelopes. At the end of the first interview, the first author opened the envelope and allocated the participant to the group indicated.
InterventionsUsual Care. This group received information according to the hospital protocol. At admission, a member of the clinical team provided verbal information about the PCI procedure, including hospitalization routine, recovery after the procedure, medications prescribed, and date for outpatient return.
Educational program. At admission, participants in this group received the same information as the usual care group, plus an educational cardiac rehabilitation program, based on SCT. The educational program was provided both orally and in written forms,14,22 and follow-up provided with three monthly telephone calls to reinforce the information. The program included: patient assessment, nutritional guidelines, management of risk factors for CAD, smoking cessation, psychosocial support, and importance of physical activity. In the educational program, we used four booklets, of which three were tested by other authors14 (“Percutaneous Transluminal Coronary Angioplasty”, “Going home after your coronary angioplasty”, and “How to take care of your heart and your health”), and a fourth, called "How to practice physical activity”, which has been described in a previous publication.22
Participants of the educational program group read the booklets with the researcher. When reading the fourth booklet, participants were evaluated for their ability to perform the proposed exercises. If any difficulty was identified, the exercise was marked as “exercise not recommended.” Three follow-up phone calls were made (between first and second week after hospital discharge, fourth and fifth week, and eleventh and twelfth week). Using the concept of persuasion,17 during the phone calls, the researcher used words to motivate the individual to comply with the recommended physical activities and lifestyle changes. Following SCT principles, the researcher sought to increase the individual's conviction in their ability to succeed in performing the recommended activities.17 Participants and researcher discussed factors that could hinder the desired changes, and how to overcome those barriers. Prior to the study, this intervention was tested in a pilot study with 20 patients with the same inclusion criteria used in this study.
Outcome measuresPrimary outcomeBaecke-Habitual Physical Activity Questionnaire (BHPAQ). Originally developed in English,23 this instrument has been validated for Brazilian Portuguese.24 The 16 items are distributed in three domains: occupational physical activity (OPA, eight items), physical exercise in leisure (PEL, four items), and leisure and locomotion activities (LLA, four items). Some of the BHPAQ items require the calculation of energy expenditure to be classified according to a compendium of physical activity.25 Details on the scale and the calculation of scores can be found in the original English version23 and in the Portuguese version.26 The total score ranges from three (inactive or sedentary) to 15 (very active). Reliability of the original version of the BHPAQ, using test-retest with three months between measurements, yielded a correlation of 0.88 for OPA, 0.81 for PEL, and 0.74 for LLA.23 Reproducibility of the Brazilian Portuguese version had statistically significant intraclass correlation coefficients of 0.69 for PEL; 0.80 for LLA, and 0.77 for total BHPAQ score.24
Secondary outcomesSelf-efficacy Scale for Physical Activity. This Brazilian Portuguese version27 was an adaptation of a specific self-efficacy instrument for physical activity.28 This scale contains two dimensions: self-efficacy for light activity (walking) and self-efficacy for moderate to vigorous physical activity (MVPA), with five items in each. Light activities are part of the everyday life of individuals without physical limitations, while vigorous activities require greater physical exertion. The instrument asks about the ability to practice activities in various circumstances, such as when the person is tired or feeling cold, for example. Answers are dichotomous and scored 0 for negative answers (no) or 1 for affirmative answers (yes). Total scores range from 0 to 5 in each dimension and from 0 to 10 for the total score. Higher scores indicate greater self-efficacy for physical activity. In a study, internal consistency measured by Cronbach's alpha was 0.83 for walking and 0.90 for MVPA.27
Hospital Anxiety and Depression Scale – HADS. Originally developed in English29 and validated and adapted to Brazilian Portuguese,30 HADS evaluates symptoms of anxiety and depression. The scale consists of 14 questions, divided into two subscales: anxiety and depression. Each subscale has seven items with scores ranging from 0 to 3, for a total score ranging from 0 to 21. Higher scores indicate more symptoms of anxiety or depression. In the Brazilian version, Cronbach's Alpha was 0.68 for the anxiety and 0.77 for the depression subscales.30
Other data collectedSociodemographic and clinical data included: dates of interview, birth, and PCI, years of education, monthly family income, sex, marital status, work status (active vs. inactive), smoking status, presence of comorbidities (“yes” or “no” for arterial hypertension, dyslipidemia, and diabetes), and type of medication prescribed and/or used by patients.
Data collection and blindingOn the day of a scheduled PCI, the first author and two research assistants recruited participants and checked for eligibility in the waiting room. Data on sociodemographic and clinical history, BHPAQ, HADS, and Self-Efficacy Scale for Physical Activity were collected from those who agreed to participate. Individuals randomized to the educational program group received the educational material and were reminded about the three times the researcher would call them after hospital discharge, in the next three months. Participants assigned to the usual care group, were informed that a member of the clinical team would provide the discharge information after the PCI.
At five to seven months after hospital discharge, one week before the expected date of return, the researcher called all participants to remind them of the upcoming outpatient visit. The final follow-up interview was conducted in the waiting room of the cardiology outpatient clinic. All instruments were completed at two time points: baseline (during hospitalization) and five to seven months after discharge.
Due to the nature of the interventions and the cardiology outpatient clinic logistics, blinding of the participants and of the first author was not possible. To minimize possible biases due to lack of blinding, participants self-reported all instruments, researchers who participated in data collection followed the same protocol, and a researcher not involved in data collection performed the statistical analysis.
Data analysisData were analyzed according to the intent-to-treat principle, where participants were analyzed in their allocated group. One individual was lost to follow-up due to death.
Descriptive analysis was performed for all collected variables. Mean ± standard deviation scores of the primary (BHPAQ) and secondary outcomes (self-efficacy and HADS), and their subdomains were compared between the two groups at final follow-up, using confidence intervals (CI) for difference in means (bootstrapping method with 1000 bootstrap samples). This method accounts for possible departures from the Gaussian distribution. Similarly, we calculated means of the changes in scores within the groups with their respective 95% CI.
Using analysis of covariance (ANCOVA), we compared the changes in scores for the outcomes as response variable, with intervention group as main factor, and baseline values as covariates.
Significance level for confidence intervals was 95% for all tests without adjustment for multiple comparisons. Data were analyzed using IBM SPSS Statistics for Mac, version 26.0 (Armonk, NY: IBM Corp.).
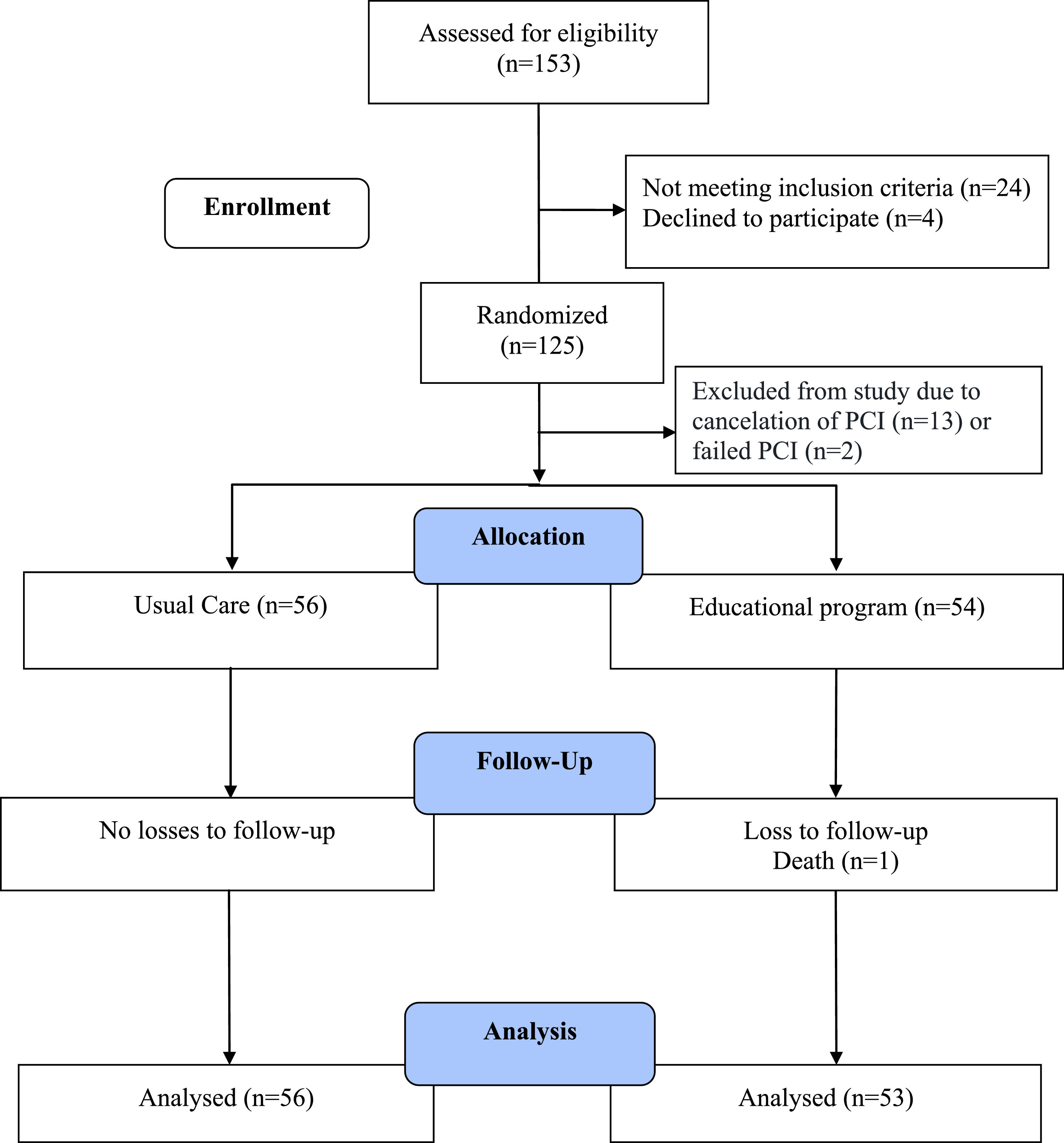
ResultsFig. 1 shows the flow diagram of the study. Of 153 individuals invited to participate in the study, 24 did not meet inclusion criteria and four refused to participate. Of the 125 remaining individuals, 62 were randomized to the usual care and 63 to the educational program groups, but 13 had their procedure cancelled and the PCI failed for two patients. Therefore, 15 patients were not considered as eligible for the study. One individual from the educational program group died before the final follow-up evaluation. The final analysis included all randomized individuals (56 in the usual care and 53 in the educational program groups).
Sociodemographic and clinical characteristics of the participants who completed the study are described in Table 1. Table 2 provides the results of the study.
Sociodemographic and clinical characteristics at baseline, by group allocation.
| Sociodemographic and clinical characteristics | Usual Care Group (n = 56) | Educational Program Group (n = 54) |
|---|---|---|
| Age in years, | 61.1 ± 9.5 | 66.9 ± 10.4 |
| 59.6 (42.5-81.3) | 67.9 (38.9-88.1) | |
| Years of education | 4.9 ± 3.3 | 4.2 ± 3.5 |
| 4 (0-15) | 4 (0-15) | |
| Family income (Reais)*, | 2547 ± 1588 | 2067 ± 1133 |
| 2000 (200-7632) | 1908 (600-6000) | |
| Sex | ||
| Male | 35 (62.5%) | 36 (66.7%) |
| Female | 21 (37.5%) | 18 (33.3%) |
| Marital status | ||
| Single, divorced, or widow(er) | 41 (73.2%) | 40 (73.6%) |
| Married or living with a partner | 15 (26.8%) | 14 (26.4%) |
| Work status | ||
| Retired | 38 (67.9%) | 36 (66.7%) |
| Active | 18 (32.1%) | 18 (33.3%) |
| Smoking | ||
| Never Smoked | 13 (23.2%) | 21 (38.9%) |
| Smoked, but not currently smoking | 22 (39.3%) | 20 (37.0%) |
| Still smoking | 21 (37.5%) | 13 (24.1%) |
| Presence of comorbidity: | ||
| Hypertension | 49 (87.5%) | 48 (88.9%) |
| Dyslipidemias | 25 (44.6%) | 30 (55.6%) |
| Diabetes Mellitus | 25 (44.6%) | 29 (53.7%) |
| Anxiety and depression medications (yes) | 12 (21.4%) | 14 (25.9%) |
Data are mean ± standard deviation, frequency (proportion) or median (minimum value - maximum value)
Comparison of habitual physical activity, self-efficacy for physical activity, and anxiety and depression symptoms between usual care and educational program groups, at baseline and final follow-up (5-7-months after hospital discharge).
| Outcome measures | Usual care (n = 56) | Educational program (n = 53) | Unadjusted difference in means between groups (95% CI)⁎⁎ | Adjusted Difference in mean changes between groups (95% CI)⁎⁎⁎ |
|---|---|---|---|---|
| Total BHPAQ | ||||
| Baseline | 6.50 ± 1.78 | 6.75 ± 1.61 | Educational Program: SSBaseline Score: SSDiff: 0.89 (0.32, 1.46) | |
| Follow-up | 6.90 ± 1.89 | 7.94 ± 1.84 | 1.04 (0.34, 1.69) | |
| Change in Score* | 0.40 ± 1.57 | 1.19 ± 1.73 | 0.80 (0.20, 1.43) | |
| BHPAQ domains | ||||
| OPA | ||||
| Baseline | 2.72 ± 0.94 | 2.86 ± 0.96 | Educational Program: NSBaseline Score: SSDiff: 0.10 (−0.12, 0.32) | |
| Follow-up | 2.47 ± 0.82 | 2.64 ± 0.62 | 0.16 (−0.14, 0.43) | |
| Change in Score * | −0.25 ± 0.65 | −0.22 ± 0.87 | 0.03 (−0.30, 0.31) | |
| PEL | ||||
| Baseline | 1.69 ± 0.89 | 1.67 ± 0.80 | Educational Program: SSBaseline Score: SSDiff: 0.66 (0.33, 0.99) | |
| Follow-up | 2.08 ± 1.00 | 2.74 ± 0.97 | 0.66 (0.27, 1.00) | |
| Change in Score * | 0.40 ± 0.94 | 1.07 ± 1.02 | 0.67 (0.32, 1.02) | |
| LLA | ||||
| Baseline | 2.09 ± 0.83 | 2.21 ± 0.66 | Educational Program: NSBaseline Score: SSDiff: 0.16 (−0.13, 0.44) | |
| Follow-up | 2.34 ± 0.92 | 2.56 ± 0.79 | 0.22 (−0.10, 0.52) | |
| Change in Score * | 0.25 ± 0.82 | 0.35 ± 0.86 | 0.10 (−0.21, 0.43) | |
| Total Self-efficacy for PA | ||||
| Baseline | 1.64 ± 2.55 | 1.96 ± 2.72 | Educational Program: SSBaseline Score: SSDiff: 2.30 (1.12, 3.49) | |
| Follow-up | 2.52 ± 3.12 | 4.98 ± 3.75 | 2.46 (1.16, 3.67) | |
| Change in Score * | 0.88 ± 3.40 | 3.02 ± 3.50 | 2.14 (0.93, 3.33) | |
| Self-efficacy for PA domains | ||||
| Light activity (walking) | ||||
| Baseline | 1.32 ± 1.98 | 1.60 ± 2.06 | Educational Program: SSBaseline Score: SSDiff: 1.15 (0.43, 1.88) | |
| Follow-up | 1.84 ± 2.09 | 3.08 ± 1.98 | 1.24 (0.48, 1.98) | |
| Change in Score * | 0.52 ± 2.63 | 1.47 ± 2.16 | 0.95 (0.12, 1.84) | |
| Self-efficacy for MVPA | ||||
| Baseline | 0.32 ± 1.18 | 0.36 ± 1.27 | Educational Program: SSBaseline Score: SSDiff: 1.20 (0.52, 1.88) | |
| Follow-up | 0.68 ± 1.68 | 1.91 ± 2.32 | 1.23 (0.49, 1.96) | |
| Change in Score * | 0.36 ± 0.52 | 1.55 ± 2.18 | 1.19 (0.48, 1.92) | |
| HADS | ||||
| Anxiety symptoms | ||||
| Baseline | 6.57 ± 4.28 | 5.51 ± 4.20 | Educational Program: NSBaseline Score: SSDiff: −0.71 (−1.89, 0.47) | |
| Follow-up | 4.46 ± 4.33 | 3.23 ± 3.12 | −1.24 (−2.62, 0.34) | |
| Change in Score * | −2.11 ± 3.73 | −2.28 ± 3.86 | −1.76 (−1.64, 1.16) | |
| Depression symptoms | ||||
| Baseline | 4.89 ± 4.31 | 3.55 ± 3.70 | Educational Program: NSBaseline Score: SSDiff: −0.78 (−2.14, 0.60) | |
| Follow-up | 4.30 ± 4.67 | 2.91 ± 3.35 | −1.40 (−2.93, 0.23) | |
| Change in Score * | −0.59 ± 4.15 | −0.64 ± 4.31 | −0.05 (−1.69, 1.62) |
Data are mean±standard deviation, mean difference (95% confidence interval)
Abbreviations: BHPAQ: Baecke-Habitual Physical Activity Questionnaire; HADS, Hospital Anxiety and Depression Scale; LLA: Leisure and locomotion activities; MVPA: Moderate to vigorous physical activity; NS = not statistically significant at 0.05 level; OPA: Occupational physical activity; PEL: Physical exercise in leisure; SS: statistically significant at 0.05 level.
Follow-up: Five to seven-months after discharge.
Difference in means = mean of educational program group minus mean of usual care group, and 95% confidence intervals calculated using bootstrap.
Analysis of covariance for change in score as outcome, intervention group as the factor, and outcome value at baseline as the covariate (adjusting value). Factor and covariate were tested at 0.05 significance level. Reference intervention: usual care. Confidence interval using Wald method. Diff: Difference in changes between educational program and usual care.
At the end of the follow-up, the educational program group had a higher mean total BHPAQ score (7.94 ± 1.84) indicating performing more physical activity than the usual care group (6.90 ± 1.09), with a mean difference of 1.04 (95% CI: 0.34, 1.69). When looking at the subdomains of the BHPAQ, the largest difference in means was for the leisure activity. For self-efficacy there was a higher mean for the total, walking, and moderate activity scores, in the educational program group. On average, the means of the anxiety and depression scores were smaller (fewer symptoms) at the follow-up for both groups, but their 95% confidence intervals included zero, showing that the differences were not statistically significant.
In the ANCOVAs, intervention group was not statistically significant for the BHPAQ subdomains of OPA and LLA, and for HADS anxiety and depression. The baseline score was statistically significant for all outcomes.
DiscussionParticipants in the educational program group presented a higher mean score of BHPAQ five to seven months after hospital discharge when compared to those who received the usual care. The 1-point difference may not represent an MDC or MCID, because these values have not yet been established for the BHPAQ total scores. Other controlled and randomized clinical trials have shown positive results of educational programs with individualized approaches when they included, in addition to written material, telephone follow-up or other strategies for remote encouragement of physical activity and/or self-efficacy for physical activity.4,5 However, the outcomes were assessed using other instruments and cannot be directly compared to our study. To date, there are no alternative instruments to the BHPAQ that have been adapted to Brazilian Portuguese, with clearly established values for MDC or MCID, and whose psychometric properties have been extensively tested in the Brazilian populations.31 Even though the magnitude of the difference between groups might not be large, according to the World Health Organization, any change aimed at increasing the practice of physical activity is important and practicing some physical activity is better than none.32
For all outcomes, the ANCOVA showed that where a person starts at baseline may affect their final score at follow-up. However, even after adjusting for baseline values, BHPAQ total and total self-efficacy had a larger change in score for the educational program group. Other controlled randomized clinical trials have shown positive effects of educational programs with individualized approaches when they included, in addition to written material, telephone follow-up or other strategies for remote encouragement of physical activity and/or self-efficacy for physical activity.4,7
Our educational program used a comprehensive approach, focused on the individual needs for physical activity, starting before the PCI, and reinforced through telephone follow-up for three months after hospital discharge. These strategies may have contributed to the increase in habitual physical activity, as has occurred in other studies that tested individualized behavioral interventions.7,19 A clinical trial in Brazilian patients with coronary heart disease demonstrated that both, the comprehensive cardiac rehabilitation, and the physical activity-based rehabilitation, had positive effects on functional capacity, but the comprehensive approach group had better outcomes.20
Systematic reviews have shown that home rehabilitation, combined with telephone follow-up, increased the level of physical activity in older adults with cardiovascular diseases.33 This is consistent with our study, considering that the participants in our study were mostly older adults. The higher scores of leisure-related physical activities at follow-up in the educational program group reinforces the importance of considering individual preferences when proposing cardiac rehabilitation programs to improve physical activity. Leisure activities might be easier to implement in a person's life than moderate ones and can be more easily adapted to the individual's preferences.
Self-efficacy scores for the practice of physical activity at follow-up were also higher in the educational program group compared to the usual care group. These results are similar to studies that used self-efficacy as a way to improve physical activity.34 Self-efficacy is important for the maintenance and encouragement of physical activity in individuals with CAD, and the individual's expectation of their ability to perform the activity must be considered. In a systematic review, authors found evidence that self-efficacy is related to the patients' participation in and adherence to physical rehabilitation performed at home, including exercise.35
In this study, we did not find statistically significant differences between the two groups in symptoms of anxiety and depression at follow-up. However, a study in China,36 demonstrated decreases in anxiety symptoms at nine and 12 months and in depression symptoms at 12 months, when compared to the participants of the usual care group.
As any other study, our results have some uncertainty, and we identified several limitations. Self-reported assessments of habitual physical activity and self-efficacy for physical activity depend on the participant's memory and can be over/underestimated. In addition, although we strived to achieve the calculated sample size, the time allotted by the funding agency and the relatively large number of cancelled PCIs (∼10%), which was not under our control, precluded us to do so. The lack of blinding of the researcher who implemented the intervention and assessed the outcomes is a limitation of this study that could not be overcome logistically. However, we sought to minimize its effect by strictly following the protocol for data collection.
ConclusionWe concluded that the educational program tested in this study is potentially effective to increase habitual physical activity and self-efficacy for the practice of physical activity in Brazilian individuals with CAD undergoing the first PCI. However, further similar randomized controlled trials in larger samples using reliable and valid outcome instruments are still needed.
This educational program uses affordable technologies, have lower cost when compared with the face-to-face cardiac rehabilitation programs37 that might require special equipment and/or specialized instructors, and has lower time and economic burden of transportation compared to going to a rehabilitation clinic, for example. The implementation of educational programs could lead to an increase of rehabilitation cardiac services especially for people who encounter barriers to participate in face-to-face cardiac rehabilitation programs in Brazil.
We would like to thank the study participants and all personnel who facilitated the research in the study hospital. This study received financial support from the Coordination for the Improvement of Higher Education Personnel (CAPES) - Finance Code 001, and from The National Council for Scientific and Technological Development (CNPq), process n. 303146/2017-6.