Brazil has insufficient cardiac rehabilitation capacity, yet density and regional variation in unmet need is unknown. Moreover, South America has CR guidelines, but whether delivery conforms has not been described.
ObjectiveThis study aimed to establish: (1) cardiac rehabilitation volumes and density, and (2) the nature of programmes, and (3) compare these by: (a) Brazilian region and (b) to other upper middle-income countries (upper-MICs).
MethodsIn this cross-sectional study, a survey was administered to cardiac rehabilitation programmes globally. Cardiac associations were engaged to facilitate programme identification. Density was computed using Global Burden of Disease study ischaemic heart disease incidence estimates. Results were compared to data from the 29 upper-MICs with cardiac rehabilitation (N=249 programmes).
ResultsCardiac rehabilitation was available in all Brazilian regions, with 30/75 programmes initiating a survey (40.0% programme response rate). There was only one cardiac rehabilitation spot for every 99 ischaemic heart disease patient. Most programmes were funded by government/hospital sources (n=16, 53.3%), but in 11 programmes (36.7%) patients depended on private health insurance. Guideline-indicated conditions were accepted in ≥70% of programmes. Programmes had a team of 3.8±1.9 staff (versus 5.9±2.8 in other upper-MICs, p<0.05), offering 4.0±1.6/10 core components (versus 6.0±1.5 in other upper-MICs, p<0.01; more tobacco cessation and return-to-work counselling needed in particular) over 44.5 sessions/patient (Q25–75=29–65) vs. 32 sessions/patient (Q25–75=15–40) in other upper-MICs (p<0.01).
ConclusionBrazilian cardiac rehabilitation capacity must be augmented, but where available, services are consistent across regions, but differ from other upper-MICs in terms of staff size and core components delivered.
Similar to other upper middle-income countries (upper-MICs), cardiovascular diseases (CVD) are among the leading burdens of disease and disability in Brazil.1 The estimated prevalence of CVD in Brazil is 6036/100,000 inhabitants,2 and hence secondary prevention is key. Cardiac rehabilitation (CR) is an established model of care for secondary prevention, which is cost-effective, affordable, and averts costly downstream healthcare utilization.3 Based on substantive evidence that participation is associated also with a 20% reduction in CV mortality and morbidity,4 clinical practice guidelines for CVD,5–7 revascularization,8,9 and heart failure patients,10 among others, recommend referral to CR. There are internationally-agreed core components (e.g., initial assessment, structured exercise training, and risk factor management, including stress)11,12 which are delivered by a multi-disciplinary team of healthcare professionals with expertise in all the secondary prevention recommendations.13 It is recommended programmes offer a minimum of 12 sessions, although greater benefits could be achieved with 36,14 and these sessions can be delivered in an unsupervised setting if patients have barriers to participation.15
Unfortunately, data on the availability and characteristics of CR programmes in Brazil are scarce.16–22 A survey published in 2013 suggested there were a mere 39 programmes in the entire country, despite the great need.20 The nature of services offered was only reported across South American countries in this paper, and hence the situation in Brazil specifically is not known. A more recent survey22 was undertaken of programmes in one of Brazil's 26 states, and 41 were identified (each treating very few patients/year); clearly an updated inventory of programmes nationally is needed. Results of the state-wide survey revealed programmes are often offered in privately-funded settings, and focus primarily on exercise training to the neglect of other core components including tobacco cessation interventions and stress management. Programmes were often staffed by physical therapists, with a notable absence of regulated health professionals in the areas of diet and mental health (including nurses) on teams.22 Overall, the current availability of programmes, density of CR spots per indicated patient, and the nature of services delivered on a national basis (and how this might vary by region and differ from similar settings outside of South America) are unknown.
Accordingly, the objectives of this investigation were to: (1) characterize the volumes, capacity and density of CR by (1a) Brazilian region, and (1b) nationally in relation to other upper-MICs; as well as (2) characterize the following aspects of CR: (2a) who pays for services, (2b) type of patients served, (2c) number and types of healthcare professionals on the CR team, (2d) number of programme sessions/dose, (2e) core components delivered (particularly non-exercise), (2f) delivery of alternative models, and (2g) barriers to delivery, again by Brazilian region, and nationally in comparison to other upper-MICs.
MethodsDesign and procedureThis study was quantitative and cross-sectional in design; detailed methods are reported elsewhere.23 In brief, countries where CR services were available were identified first through previous reviews.17,24 In countries where CR services were not suspected to be available, the internet was searched and major CR and cardiology societies were contacted to identify any programmes or verify lack thereof.
For each country identified to offer CR such as Brazil, first available CR or cardiac societies leadership were contacted, such as the Associação Brasileira de Fisioterapia Cardiorrespiratória (ASSOBRAFIR) and Sociedade Brasileira de Cardiologia (SBC). If there was no society available or response, “champions” were identified. Identified leaders were sent an e-mail requesting their collaboration to (a) determine the number of programmes in their country, and (b) administer the survey to each programme in their country.
The most responsible clinician at each programme was emailed with the request to complete the survey. The study was reviewed by York University's Office of Research Ethics (Toronto, Canada) and Mayo Clinic's Institutional Review Board (Rochester, United States). Informed consent was secured through an online form. The survey was administered through REDCap, with data collection occurring from June 2016 to December 2017. Contacts were sent 2 e-mail reminders, at 2 week intervals.
SampleFor the global study, the sample consisted of all CR programmes identified in the world that offer services to patients following an acute cardiac event or hospitalization (i.e., Phase II). The inclusion criteria were CR programmes that offered: (1) initial assessment, (2) structured exercise, and (3) at least one other strategy to control CV risk factors.
For the purposes of this study, CR programmes in Brazil were selected as well as in countries with the same income classification as per the World Bank25 (i.e., other upper-MICs). There are 55 such countries of which, 32 (58.18%) were determined to have CR.
Brazil is geo-politically divided into five regions by the Instituto Brasileiro de Geografia e Estatística (IBGE)26. These are: Central-West (includes Federal District where Brazil's national capital, Brasília, is situated), South, Southeast, North and Northeast (Supplementary material Appendix A).
MeasuresWith regards to the first objective, CR programme volume was defined as the median number of patients served by a programme annually (programme-reported in survey, described below). Region and national CR capacity were computed by multiplying the median number of patients a programme could serve annually (programme-reported in survey) among the responding programmes in a given region or country respectively, multiplied by the total number of programmes in that jurisdiction. To compute density, information on ischaemic heart disease (IHD) incidence in each Brazilian region and upper-MIC was pulled from the Global Burden of Disease2 (2016 estimates); CVD incidence included rheumatic heart disease so to be conservative, IHD was used, however this is an under-estimate because heart failure is not considered. The ratio of capacity per annual incident patient for each country was computed (i.e., density or CR spots per indicated patient).
Development of the survey is described in detail elsewhere.27 In short, items were based on previous national/regional CR programmes surveys.20,28,29 Most items had forced-choice response options, and skip-logic was used to obtain more detail where applicable. The survey was translated to Brazilian-Portuguese (Online Appendix). It was reviewed by 10 CR healthcare professionals (i.e., target respondents), who identified some unclear terminology which was revised.
The following variables were assessed: (i) who funds the programme (i.e., private sources such as healthcare insurance or patients, public sources such as government, or a combination of these sources [i.e., hybrid]), (ii) the type (e.g., myocardial infarction, as well as non-cardiac indications) and number of patients served per session (as well as staff-to-patient ratio), (iii) the number and types of healthcare professionals on the CR team (part-time staff were counted as 0.5), (iv) dose of CR (in hours; i.e., sessions per week×duration in weeks×duration of exercise sessions in minutes); (v) the type and number of core components delivered (of 10; i.e., initial assessment [including risk factors assessed and type of functional capacity test], risk stratification, structured exercise, patient education, risk factor management, nutrition counselling, stress management, tobacco cessation interventions, prescription/titration of medication, and communication with a primary healthcare provider), and (vi) whether the programme offers alternative CR models (i.e., home or community-based programmes, or hybrid models where patients transition from supervised to unsupervised settings).
Data analysisSPSS version 24 was used for analysis.30 All initiated surveys were included. The number of responses for each question varied due to missing data (e.g., respondent did not answer a question due to lack of willingness or potential inapplicability, use of skip logic); for descriptive analyses, percentages were computed with the denominator being the number of responses for a specific item.
Descriptive statistics were used to characterize volume, capacity, density, as well other closed-ended items in the survey (e.g., funding sources, core components delivered, and healthcare professionals on the CR team). All open-ended responses were coded/categorized. Aspects of CR were then compared by region (only descriptively due to limited sample sizes in 2 regions), and nationally versus other upper-MICs using Mann–Whitney U or Chi-square tests as applicable.
ResultsCR is available in 5/5 (100.0%) Brazilian regions. Data were collected in 4 (80.0% regional response rate). Nationally, 30 of 75 programmes responded (40.0% programme response rate). The number of programmes and responses per region were 0 of 1 CR in North, 5 of 9 in Northeast, 2 of 6 in Central-west, 21 of 45 in Southeast and 2 of 14 in South (in detail at Appendix A).
Of the 32 upper-MICs that had CR, data were collected in 29 (90.6% country response rate); 249 surveys were completed (mean programme response rate=52.5% across these countries).23 These countries were: Algeria, Argentina, Belarus, Bosnia and Herzegovina, Bulgaria, China, Colombia, Costa Rica, Cuba, Dominican Republic, Ecuador, Georgia, Iran, Jamaica, Kazakhstan, Lebanon, Macedonia, Malaysia, Mauritius, Mexico, Panama, Paraguay, Peru, Romania, Russia, Serbia, South Africa, Turkey, Venezuela.
Availability, volumes, capacity and densityOverall, 16 (53.3%) were in a hospital; all of which were academic, tertiary centres (with 1 being military).
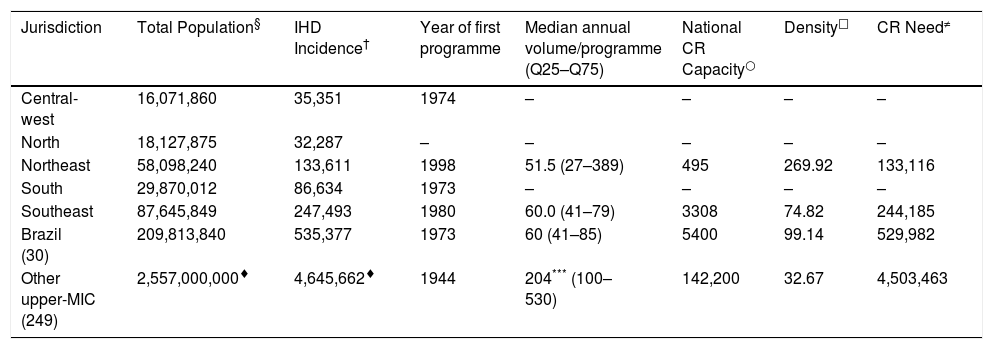
As shown in Table 1, programme volumes were significantly lower than other upper-MICs. Programmes served a median of 4.5 [Quartile 1 and 3 (25–75)=2.7–8.5] patients per exercise session (compared to 7.0 [Q25–75=2.7–8.5] in other upper-MICs; p=0.03). The median number of patients per 1 staff during supervised exercise was 5.0 (Q25–75=3.0–10.0; similar to other UPPER-MICs=6.0, Q25–75=3.0–10.0).
Volume, capacity and density by Brazilian region, and other upper middle-income countries.
| Jurisdiction | Total Population§ | IHD Incidence† | Year of first programme | Median annual volume/programme (Q25–Q75) | National CR Capacity○ | Density□ | CR Need≠ |
|---|---|---|---|---|---|---|---|
| Central-west | 16,071,860 | 35,351 | 1974 | – | – | – | – |
| North | 18,127,875 | 32,287 | – | – | – | – | – |
| Northeast | 58,098,240 | 133,611 | 1998 | 51.5 (27–389) | 495 | 269.92 | 133,116 |
| South | 29,870,012 | 86,634 | 1973 | – | – | – | – |
| Southeast | 87,645,849 | 247,493 | 1980 | 60.0 (41–79) | 3308 | 74.82 | 244,185 |
| Brazil (30) | 209,813,840 | 535,377 | 1973 | 60 (41–85) | 5400 | 99.14 | 529,982 |
| Other upper-MIC (249) | 2,557,000,000♦ | 4,645,662♦ | 1944 | 204*** (100–530) | 142,200 | 32.67 | 4,503,463 |
– Not provided, available or applicable.
Calculated using median number of patient programme could serve per year (from survey) multiplied by the number of programmes in the jurisdiction or country. Value represents the number of patients who could receive CR in a year (i.e., CR spots).
Based on ratio of need (i.e., IHD incidence) to supply (i.e., national CR capacity). Represents number of CR spots per patient in need.
Capacity, density and unmet need are also shown in Table 1. Density is almost three time worse than in other upper-MICs. When compared to the 86 other countries of the world with CR and sufficient information to compute it, Brazil's density is 73rd worst (data shown elsewhere).31
Nature of CR servicesProgramme responders were asked to report who pays for their services, and could check all applicable sources (n=30; only 7.0% reported >1 source). Appendix A displays the funders of CR by region. Nationally, 16 (53.3%) reported government funding (with only 2400 spots nationally funded by government), 11 (36.7%) reported private health insurance, 2 (7.0%) reported both. In upper-MICs No CR programme reported that patients pay all programme out-of-pocket, however the average percent of the total programme patient pay is 75.50±36.15% more than in other upper-MICs (38.93±33.90%, p<0.05).
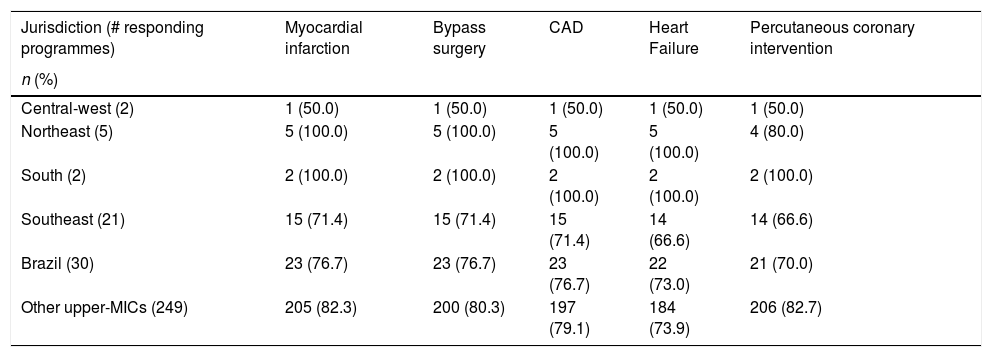
The most common types of patients accepted in CR programmes are shown in Table 2. There were no significant differences between Brazil and other upper-MICs (p>0.05). Many programmes also accepted patients with non-cardiac indications, namely: high-risk primary prevention (n=21, 70.0%), diabetes (n=17, 56.6%), intermittent claudication/peripheral vascular disease (n=16, 53.3%), lung disease (n=15, 50.0%), stroke (n=9, 30.0%) and cancer (n=8, 26.7%) patients. This did not differ from other upper-MICs (all p>0.05).
Most-commonly accepted cardiac rehabilitation indications, by Brazilian region, vs. other upper middle-income countries.
| Jurisdiction (# responding programmes) | Myocardial infarction | Bypass surgery | CAD | Heart Failure | Percutaneous coronary intervention |
|---|---|---|---|---|---|
| n (%) | |||||
| Central-west (2) | 1 (50.0) | 1 (50.0) | 1 (50.0) | 1 (50.0) | 1 (50.0) |
| Northeast (5) | 5 (100.0) | 5 (100.0) | 5 (100.0) | 5 (100.0) | 4 (80.0) |
| South (2) | 2 (100.0) | 2 (100.0) | 2 (100.0) | 2 (100.0) | 2 (100.0) |
| Southeast (21) | 15 (71.4) | 15 (71.4) | 15 (71.4) | 14 (66.6) | 14 (66.6) |
| Brazil (30) | 23 (76.7) | 23 (76.7) | 23 (76.7) | 22 (73.0) | 21 (70.0) |
| Other upper-MICs (249) | 205 (82.3) | 200 (80.3) | 197 (79.1) | 184 (73.9) | 206 (82.7) |
No statistical analyses were performed to compare regions because of the small sample sizes. Mann–Whitney U tests were used to test for significant differences between Brazil and other upper-MICs. There were no significant differences. CAD, coronary artery disease (i.e., with no recent event or procedure).
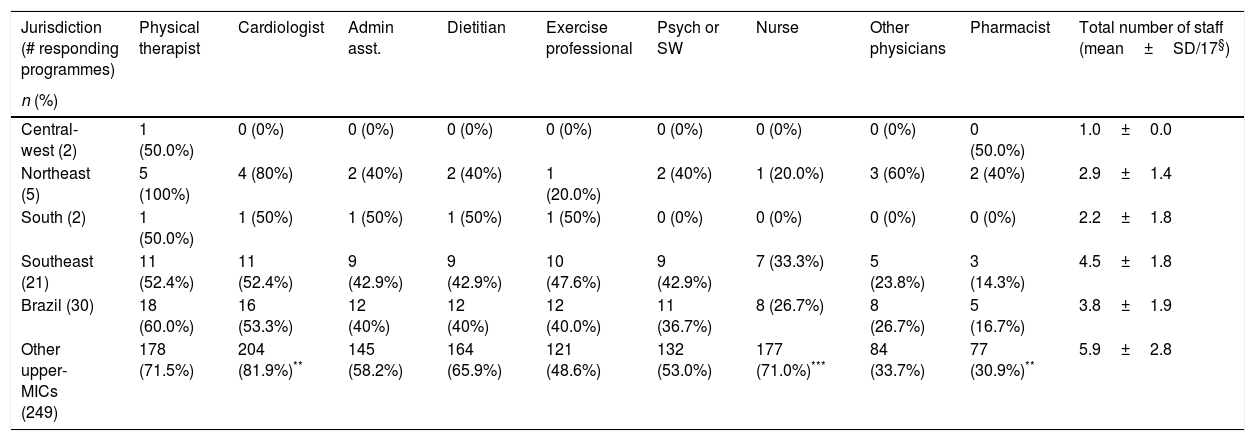
The number and nature of healthcare professionals on CR teams is shown in Table 3. Brazil programmes had significantly fewer staff versus other upper-MICs; specifically, teams were less-often comprised of nurses, cardiologists and pharmacists than other upper-MICs.
Healthcare professionals on the cardiac rehabilitation team, by Brazilian regions vs other upper middle-income countries.
| Jurisdiction (# responding programmes) | Physical therapist | Cardiologist | Admin asst. | Dietitian | Exercise professional | Psych or SW | Nurse | Other physicians | Pharmacist | Total number of staff (mean±SD/17§) |
|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | ||||||||||
| Central-west (2) | 1 (50.0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (50.0%) | 1.0±0.0 |
| Northeast (5) | 5 (100%) | 4 (80%) | 2 (40%) | 2 (40%) | 1 (20.0%) | 2 (40%) | 1 (20.0%) | 3 (60%) | 2 (40%) | 2.9±1.4 |
| South (2) | 1 (50.0%) | 1 (50%) | 1 (50%) | 1 (50%) | 1 (50%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2.2±1.8 |
| Southeast (21) | 11 (52.4%) | 11 (52.4%) | 9 (42.9%) | 9 (42.9%) | 10 (47.6%) | 9 (42.9%) | 7 (33.3%) | 5 (23.8%) | 3 (14.3%) | 4.5±1.8 |
| Brazil (30) | 18 (60.0%) | 16 (53.3%) | 12 (40%) | 12 (40%) | 12 (40.0%) | 11 (36.7%) | 8 (26.7%) | 8 (26.7%) | 5 (16.7%) | 3.8±1.9 |
| Other upper-MICs (249) | 178 (71.5%) | 204 (81.9%)** | 145 (58.2%) | 164 (65.9%) | 121 (48.6%) | 132 (53.0%) | 177 (71.0%)*** | 84 (33.7%) | 77 (30.9%)** | 5.9±2.8 |
Includes Cardiologist, Physiatrist, Sports Medicine Physician, other Physician, Physical therapist, Nurse, Nurse–practitioner, Psychiatrist, Psychologist, Social worker, Dietitian, Kinesiologist, Pharmacist, Exercise specialist, Community Health worker, Administrative assistant/Secretary, Other.
No statistical analyses were performed to compare regions because of the small sample sizes. Chi-square tests were used to test for significant differences between Brazil and other upper-MICs (denoted in other upper-MIC row):
CR programme dose was just over 44.5h (Q25–75=30–70); this was significantly greater than other upper-MICs (30.0h; Q25–75=10–45; p=0.001). Nationally, programmes offered 44.5 sessions/patient (Q25–75=29–65); median frequency was 3 sessions per week, and median programme duration was 15 weeks (Q25–75=12–16); this was significantly greater than other upper-MICs (32 sessions/patient, Q25–75=15–40 and 10 weeks, Q25–75=6–12).
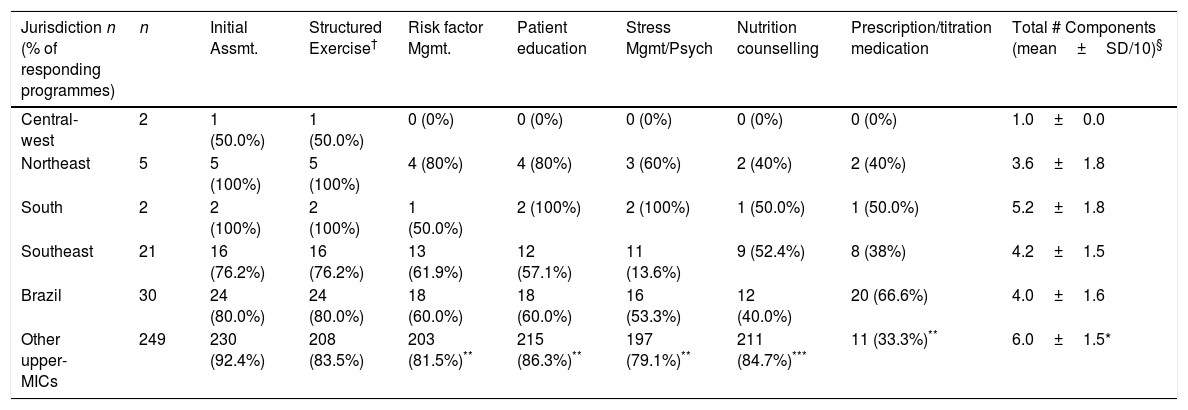
Programmes offered 4/10 core components on average and the most-frequently delivered components are shown in Table 4. Initial assessment and structured exercise are offered much more frequently than other components (i.e., not comprehensive programmes), with communication with primary care (n=10, 33.3%), tobacco cessation (n=6, 20.0%) and return to work counselling (n=4, 13.3%) least commonly offered. Programmes in Brazil offered significantly fewer components than other upper-MICs, with less percentage of programmes (p<0.01) offering the majority of core components except initial assessment and structured exercise.
Key Core Components Delivered by Region, Nationally and in Other Upper Middle-Income Countries.
| Jurisdiction n (% of responding programmes) | n | Initial Assmt. | Structured Exercise† | Risk factor Mgmt. | Patient education | Stress Mgmt/Psych | Nutrition counselling | Prescription/titration medication | Total # Components (mean±SD/10)§ |
|---|---|---|---|---|---|---|---|---|---|
| Central-west | 2 | 1 (50.0%) | 1 (50.0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1.0±0.0 |
| Northeast | 5 | 5 (100%) | 5 (100%) | 4 (80%) | 4 (80%) | 3 (60%) | 2 (40%) | 2 (40%) | 3.6±1.8 |
| South | 2 | 2 (100%) | 2 (100%) | 1 (50.0%) | 2 (100%) | 2 (100%) | 1 (50.0%) | 1 (50.0%) | 5.2±1.8 |
| Southeast | 21 | 16 (76.2%) | 16 (76.2%) | 13 (61.9%) | 12 (57.1%) | 11 (13.6%) | 9 (52.4%) | 8 (38%) | 4.2±1.5 |
| Brazil | 30 | 24 (80.0%) | 24 (80.0%) | 18 (60.0%) | 18 (60.0%) | 16 (53.3%) | 12 (40.0%) | 20 (66.6%) | 4.0±1.6 |
| Other upper-MICs | 249 | 230 (92.4%) | 208 (83.5%) | 203 (81.5%)** | 215 (86.3%)** | 197 (79.1%)** | 211 (84.7%)*** | 11 (33.3%)** | 6.0±1.5* |
Initial assessment, risk stratification, structured exercise, patient education, risk factor management, nutrition counselling, stress management, tobacco cessation interventions, prescription/titration of medication, and communication with a primary healthcare provider.
Includes physical activity counselling, exercise prescription and/or exercise training.
No statistical analyses were performed to compare regions because of the small sample sizes. Chi-square tests were used for significant differences between Brazil and other upper-MICs (denoted in other upper-MICs row).
During the core component of initial assessment, 20 (66.7%) programmes had patients undergo an exercise stress test. Risk factors assessed pre-programme included blood pressure (n=30, 100.0%), physical inactivity (n=30, 100.0%), tobacco use (n=23, 76.7%), anthropometrics (n=21, 70.0%), lipid profiles (n=20, 66.6%), harmful use of alcohol (n=20, 66.6%), blood glucose (n=15, 50.0%), depression (n=13, 43.3%), and diet (n=12, 40.0%). Most programmes also delivered resistance training (n=19, 63.3%). In 22 (73.3%) programmes, patients were re-assessed at programme end, and the results were communicated to the patients’ primary care physician in 10 (33.3%) programmes. Finally, 18 (60.0%) programmes had some form of patient contact post-programme.
Seven (23.3%) programmes reported delivery of any alternative model of CR (6 in Southeast and 1 in Northeast). This proportion did not differ from other upper-MICs (n=49, 19.7%). Five (3.0%) programmes reported using smartphones, an “app”, or text messaging with patients (i.e., some form of eCR; versus n=32, 12.8% in other upper-MICs, p<0.05). Four (13.3%) programmes reported offering a “hybrid” model (versus n=16, 6.4% in other upper-MICs) and only one programme reported offering community-based CR (versus n=18, 7.2% in other upper-MICs). Nationally, 2 (6.6%) programmes offered alternative forms of exercise (e.g., pilates, dancing).
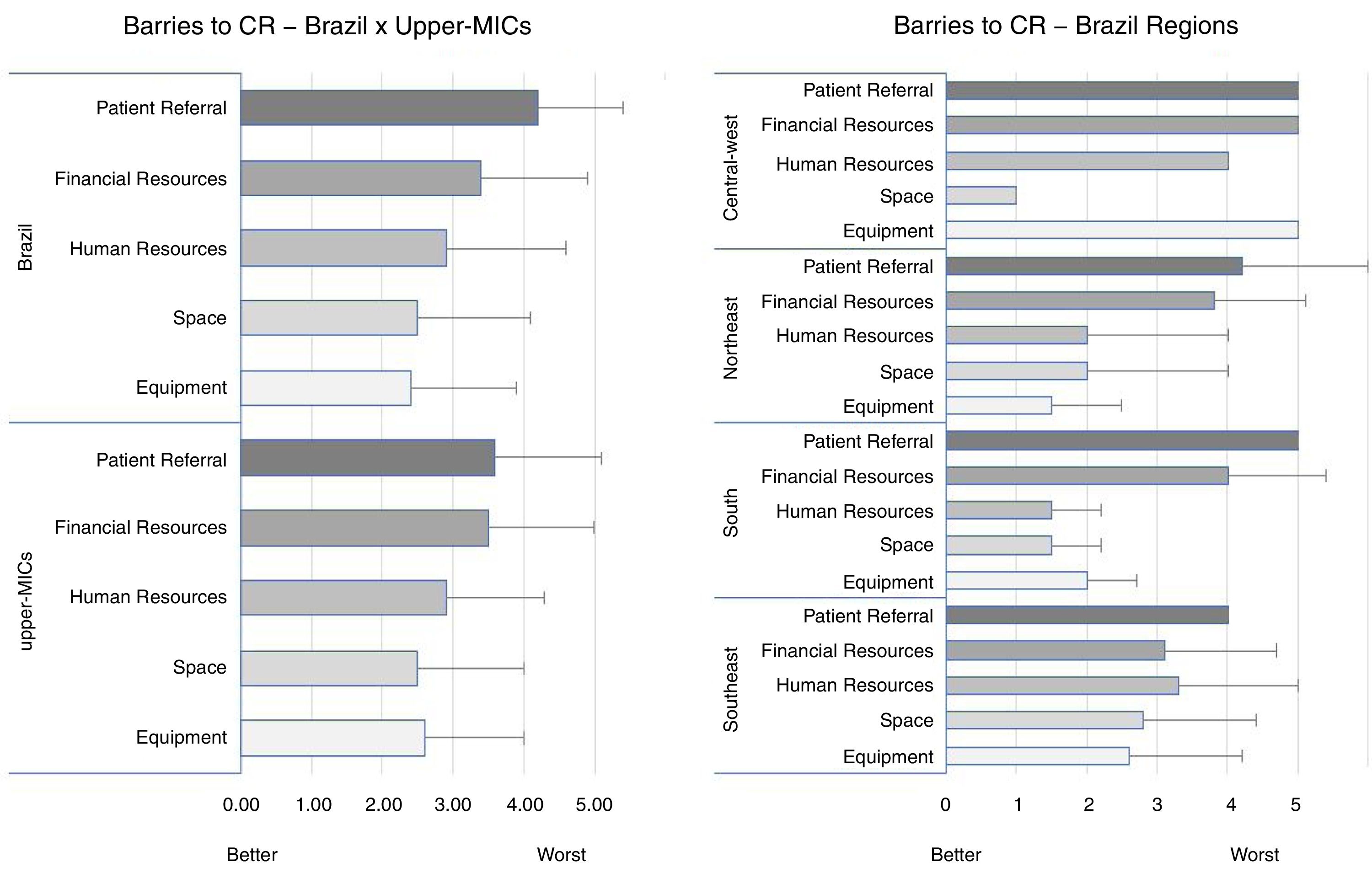
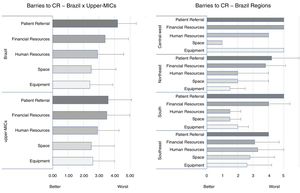
Delivery barriersFig. 1 displays barriers to CR delivery by Brazilian region and in other upper-MICs. The greatest barrier in all jurisdictions was patient referral (although tied for Central-West). No barrier differences were found compared to other upper-MICs. Other barriers reported by Brazilian respondents included transportation (n=22, 73.3%), lack of knowledge about CR among healthcare professionals (n=5, 16.7%) and patient motivation (n=3, 10.0%).
Barriers to Cardiac Rehabilitation Delivery by region, and versus other upper-MICs.
Respondents did not provide information on barriers for CR in 6/30 Brazil surveys and in 16/249 other UPPER-MICs.
No statistical analyses were performed to compare regions because of the small sample sizes.
Mann–Whitney U were used to test for significant differences in Brazil versus other UPPER-MICs. No significant differences were found.
Upper-MIC, upper middle-income country.
For the first time, the unmet need for CR in Brazil has been established, with density estimates computed based on indicated patient burden specifically rather than population as in previous studies.19 Over 500,000 more spots are needed per year to treat IHD patients in Brazil, to ensure they achieve the mortality and morbidity reductions associated with participation.4
Guideline-indicated patients are appropriately accepted (including over 70% of programmes accepting heart failure patients, which is the most recent indication10) as in other upper-MICs, with these patients participating generally in 45 sessions (3 times/week over 15 weeks; total 45h), which is considered a sufficient dose to achieve mortality and morbidity reductions.14 Most patients received only 4 of 10 core components (e.g., initial assessment, structured exercise, risk factor management, and patient education), delivered by a multidisciplinary team comprised of only ∼4 members (e.g., physical therapists, cardiologists, administrative assistants and dietitian). There is great need for capacity around return-to-work and tobacco cessation which could be achieved with inclusion of occupational therapists and psychologist on a part-time basis on CR teams. The low degree of communication with primary care physician could be related to the low number of nurses on CR teams in Brazil and reflects the struggle to achieve integrality of health care. Scant programmes delivered CR unsupervised.
When compared to previous studies on CR in Brazil,20,21 it does appear the number of programmes is increasing (75 identified), although differences could be explained by different methods of programme identification. In one of the Southeast region alone 41 programmes were identified, however many of them are offering exercise only.22
For the first time, CR delivery in Brazil was compared inferentially with other comparable countries. There was consistency in CR delivery with other upper-MICs in terms of accepted indications but also major differences in volumes, density and funding source. Brazilian programmes were less comprehensive, mainly exercise-based programmes, delivered by a limited staff, over a significantly longer period, when compared to other upper-MICs. When considering overall “quality” (i.e., of 20 structure and process indicators such as wait times, risk factors assessed and components) of programmes in Brazil, it was adequate (12 indicators “met” [i.e., ≥75% programmes], or 60%), but considered low when compared to other countries globally (ranked 14th or poorest; see).23
The implications of this work are many. First, capacity needs to be increased dramatically, both by increasing the number of patients treated per programme (particularly through greater referral) and by initiating new programmes. Brazilian programmes are not exploiting alternative delivery settings such as home-based service and eCR, as is also observed in other upper-MICs. Considering the continental nature of the country and the high number of small cities, increasing delivery of alternative models could improve CR capacity, especially in regions where there are few programmes (North and Central-west). Home-based CR has been established as a viable approach to delivery in low-risk patients in the Brazilian context.32
Second, available programmes should be resourced for staffing by a larger team, particularly including nurses and community healthcare workers (who can be trained to deliver several of the core components),11 and for delivery of comprehensive services, to optimize patient outcomes.33,34 A CR education curriculum has been validated in Brazilian-Portuguese and demonstrated effective, which covers the majority of core components (https://www.healtheuniversity.ca/pt/CardiacCollege/About/Pages/download-guide.aspx).35,36 Moreover, the International Council of Cardiovascular Prevention and Rehabilitation has developed a training and certification programme on how to feasibly deliver all core CR components in low-resource settings, which could be used to augment availability of CR professionals to deliver all components (http://globalcardiacrehab.com/training-opportunities/certification/).37
This study has several limitations, particularly related to generalizability and measurement. Firstly, response rates to online surveys are notoriously low. The rate was 40% in the current study for Brazilian programmes and 50.3% for other upper-MICs, which is fair, but suggests there may be bias.
Second, survey items were piloted, but not validated against real-world CR delivery. Respondents may have been inclined to respond in a socially-desirable manner, such that results were skewed to reflect better provision of CR. However, participants were informed that their responses were confidential. Third, the survey was translated, and although reviewed by CR professionals, all best practices in scale translation and validation were not undertaken. Finally, multiple comparisons were performed, and there were very few respondents in some regions, and hence caution is necessary when interpreting the findings.
ConclusionCR has been available in Brazil for almost 55 years. There are 75 programmes, each treating on average 60 guideline-indicated but also primary prevention and non-communicable disease patients per year, over almost 15 weeks, through 4 core components delivered by a team of 4 staff. Programmes were fairly consistent with other upper-MICs, except Brazilian programmes offer longer programmes, with fewer components and few staff. However, there is only 1 CR spot for every 99 patients in need annually (more than other upper-MICs), with 500,000 more spots needed nationally to meet IHD demand alone. Most programmes were funded by government sources but in over one-third of programmes patients need private healthcare insurance, further limiting access. CR capacity must be augmented in Brazil, potentially through increased provision of eCR.
FundingThis project was supported by a research grant from York University's Faculty of Health, Canada; Conselho Nacional de Pesquisa(CNPq# 305786/2014-8), Brazil; Coordenação de Aperfeiçoamento de Pessoal de Nível Superior(CAPES - Código de Financiamento 001), Brazil and Fundação de Pesquisa de Minas Gerais(FAPEMIG # PPM00869-15 and 00554-17), Brazil.
Conflicts of interestThe authors declare no conflicts of interest.
The International Council of Cardiovascular Prevention and Rehabilitation through which this study was undertaken, and other national champions who collaborated to identify and reach programmes in Brazil, namely: Aparecida Maria Catai, Gerson Cipriano, Iracema Umeda, Jocimar Martins, Lilian Pinto da Silva, Mauro Augusto dos Santos, Marlus Karsten, Renata Cruzeiro, Thaianne Sérvio, and in their upper middle-income country, namely: Drs. Claudia Anchique-Santos, Eduardo Rivas-Estany, Lela Maskulia, Masoumeh Sadeghi, Hermes Lomeli, Graciela Gonzalez, Rosalia Fernandez, Dan Gaita, Wayne Derman. We also thank the World Heart Federation who formally endorsed the study protocol.