A dual-task tool with a challenging and daily secondary task, which involves executive functions, could facilitate the screening for risk of falls in older people with mild cognitive impairment or mild Alzheimer's disease.
ObjectiveTo verify if a motor-cognitive dual-task test could predict falls in older people with mild cognitive impairment or mild Alzheimer's disease, and to establish cutoff scores for the tool for both groups.
MethodsA prospective study was conducted with community-dwelling older adults, including 40 with mild cognitive impairment and 38 with mild Alzheimer's disease. The dual-task test consisted of the Timed up and Go Test associated with a motor-cognitive task using a phone to call. Falls were recorded during six months by calendar and monthly telephone calls and the participants were categorized as fallers or non-fallers.
ResultsIn the Mild cognitive impairment Group, fallers presented higher values in time (35.2s), number of steps (33.7 steps) and motor task cost (116%) on dual-task compared to non-fallers. Time, number of steps and motor task cost were significantly associated with falls in people with mild cognitive impairment. Multivariate analysis identified higher number of steps spent on the test to be independently associated with falls. A time greater than 23.88s (sensitivity=80%; specificity=61%) and a number of steps over 29.50 (sensitivity=65%; specificity=83%) indicated prediction of risk of falls in the Mild cognitive impairment Group. Among people with Alzheimer's disease, no differences in dual-task between fallers and non-fallers were found and no variable of the tool was able to predict falls.
ConclusionThe dual-task predicts falls only in older people with mild cognitive impairment.
A fall is defined as “an event which results in a person coming to rest inadvertently on the ground or floor or other lower level and other than as a consequence of such things as: sustaining a violent blow; loss of consciousness; sudden onset of paralysis; or an epileptic seizure”.1 Falls in older people are a challenge to international health systems, since falls can lead to fractures, fear of falling, reduced quality of life, institutionalization, hospitalization and death.2
People with cognitive impairment experience falls up to two times greater than older people with preserved cognition often resulting in more serious consequences.2,3 Although reasons for the higher prevalence of falls are still not clear, neurodegenerative changes in mild cognitive impairment (MCI) and dementia result in cognitive, physiological and functional deficits, which contribute to risk of falls.4 Furthermore, cognitive deficits in older adults with MCI and Alzheimer's disease (AD) may increase risk of falls because of changes in executive functions and ability to solve problems, to make decisions and to perform simultaneous tasks.4,5
The screening for risk of falls in older adults with cognitive impairment is needed to better prevent falls. Among several tools, dual-task tests have been used to predict falls in older people with preserved cognition6,7 and cognitive impairment.4 In dual-task situations, individuals who prioritize the secondary cognitive task seem to show increased risk of falls during walking.6
Although dual-task tests are promising for screening falls,6–8 there is a lack of prospective longitudinal studies assessing prediction of falls in people with MCI and separately in people with AD in its mild stage. New dual-task tests which are composed of walking while performing a motor-cognitive task (calling a phone number in this case) were used to assess mobility in older people without cognitive impairment,9 with MCI or mild AD.10 In this sense, the use of a dual-task tool (walking with a challenging and daily secondary task), which involves executive functions, could facilitate the screening for risk of falls in older people with MCI or mild AD. Also, different measures might involve specific neural areas and cognitive functions. Thus, it is important to use measures other than time when assessing dual-task tests.11
The purpose of this prospective cohort study was to verify whether a motor-cognitive dual-task test could predict falls in community-dwelling older people with MCI or mild AD and to establish cutoff scores for the tool applied in each group. We hypothesized that the dual-task test would predict falls in older adults with MCI and mild AD, since it required greater cognitive and motor interaction and it approached to real situations of falls.
MethodsStudy design and settingThis study was a 6-month prospective cohort study at the Universidade Federal de São Carlos (São Carlos-SP, Brazil) from 2015 through 2016.
ParticipantsCommunity-dwelling people aged 60 and over who lived in São Carlos (Brazil) were eligible for the study. Inclusion criteria were the ability to walk at least 10m alone without a walking aid, availability to participate in the proposed assessments, and admission to one of the groups studied (MCI or mild stage AD). Exclusion criteria were motor sequel after stroke, mixed dementia and other types of dementia without being AD, other neurological diseases that interfered in cognition or mobility, severe uncorrected visual or auditory disorders, and people with AD in moderate or advanced stages.
The diagnosis of MCI or mild AD was confirmed by an experienced neurology professor. Criteria for diagnosis of MCI were: (1) cognitive complaint reported by the volunteer or a care giver (i.e., a person who stayed with the volunteer subject at least half a day, four days per week); (2) objective cognitive impairment not related to delirium (i.e., Clinical Dementia Rating Scale-CDR=0.5 point)12; (3) normal global cognitive function for educational level13 achieved; (4) preserved functionality14; and, (5) absence of clinical dementia.15 The diagnosis of AD followed the Diagnosis and Statistical Manual of Mental Disorders (DSM-V TR),15 and only individuals with CDR=1 (mild stage) were included in the AD Group.12
The study was carried out in accordance with the Declaration of Helsinki. Ethical approval was obtained from the Universidade Federal de São Carlos (São Carlos-SP, Brazil) (819.668/2014). All participants were informed about the research objectives, risks and benefits and they provided a written informed consent.
MeasurementAll participants were instructed to wear comfortable clothing and their usual closed shoes, to eat at least one hour prior to testing, not to practice vigorous exercises the day before the testing and to bring any necessary eyeglasses or hearing aid to the test. The tests were applied in a closed environment and all instructions were explained in a simple, clear and objective way.
Clinical and sociodemographic data were collected, including age, gender, years of schooling, use of drugs, and presence of diseases, The Minnesota Leisure Time Activities Questionnaire was used for weekly caloric expenditure16 and the Geriatric Depression Scale was used for risk of depressive symptoms.17
Dual-taskThe dual-task was evaluated using the Timed Up and Go test (TUG)18 associated with a motor-cognitive task (TUG-DT).10 Before the dual-task test, the subjects performed both tasks separately. Each test was demonstrated once by the assessor and one practice trial was performed by each subject. If the subject did not perform the practice trial correctly, one more trial was done.
For the isolated motor-cognitive task, a drawn raffled card containing a sequence of eight numbers was fixed in a wireless phone (15.1-cm high×4.7-cm width×2.2-cm depth; Motorola® FOX 1000 model) and placed on a table (68.5cm high). While seated in front of this table, the subject was instructed to pick up the phone after the command “go”, dial the numbers on the card then place the phone on the table. The time and number of errors (incorrectly dialed number or an absence of any number being dialed) were registered after the command “go” and stopped when the subject placed the phone back on the table. The TUG was applied at the usual speed using a chair 45-cm high with trunk support and 68-cm-high armrests18 and time spent doing the test was recorded. According to Alexandre et al.,18 a predictive value of 12.47s on the TUG (sensitivity=73.7%; specificity=65.8%) could be used as an indicator of risk of falls in older people.
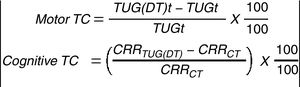
After completing both isolated tasks, the TUG-DT test was performed with a new drawn card (that contained a sequence of eight numbers) fixed on the phone. The subject was instructed to get up after the command “go”, pick up the phone on the table (placed at 50cm away from the chair, on the right side and parallel to the path), dial the numbers of the card while walking the TUG path, place the phone back on the table, and sit down on the chair. Total time, number of steps, errors and stops, cadence (steps/minute) and number of correct response per time ratio spent on the TUG-DT were analyzed. Also, the motor task cost and cognitive task cost were calculated, as shown in Fig. 1.19
All tests described above were paused and standardized instructions were given, and they were performed by a single trained assessor to maximize the consistency of the mobility assessment and to minimize possible biases in older people with varying comprehension difficulties, which were better described in the study of Ansai et al.10
FallsAfter baseline assessment, each subject/care giver received a 6 month calendar of falls20 to fill out. Also, all subjects/care givers received monthly telephone calls to ensure accurate falls data and to reinforce the definition of a fall and to encourage filling out the calendar. Each subject was classified as a faller, (i.e., a person who fell at least once during the follow-up), or non-faller based on the information provided by the subject or care giver.
Study sizeThe sample size was calculated by the G*Power 3.1 software. Admitting the main study design (using univariate logistic regression analysis), a type I error of 5%, a statistical power of 80%, an effect size of 0.3, and the number of predictors (1), it was determined that a minimum of 29 people should be in each group.
Statistical methodsA significance level of α=0.05 and the SPSS software (20.0) were used to analyze the data. Data normality was tested using the Kolmogorov–Smirnov test. An independent t-test and the Chi-square test were used to verify differences in sociodemographic and clinical characteristics between fallers and non-fallers in older adults with MCI or mild AD. Univariate logistic regression (adjusted for prevalence of rheumatism in the MCI Group) was applied to identify the association between variables of the dual-task test and falls follow-up for each group. Only the variables with significant association were entered into a multivariate backward stepwise logistic regression equation (adjusted for prevalence of rheumatism in the MCI Group) to predict falls. The groups were analyzed separately in the logistic regression models. The selection of variables in the multivariate model was based on the likelihood ratio test p values (0.05 for entry, 0.1 for removal). The receiver operating characteristics (ROC) curve was used to determine the cutoff score that maximized both sensitivity (i.e., how well it correctly identifies subjects with a condition of interest) and specificity (i.e., the frequency that the test is negative in the absence of a condition of interest) for the time spent on the TUG-DT and the variable that better predicted falls by the multivariate regression model.
ResultsParticipantsAt baseline, 40 individuals with MCI and 38 with mild AD were assessed. During the follow-up period, two subjects from the MCI Group and one subject from the AD Group died, so their data were excluded. Thus, the final sample was composed by 38 older people with MCI and 37 with mild AD.
Descriptive dataFalls were reported by 20 subjects with MCI and 19 subjects with mild AD. In the MCI Group, fallers presented with a higher prevalence of osteoarthritis (50%) compared to non-fallers. Other sociodemographic and clinical variables were not significantly different between fallers and non-fallers in each group (Table 1).
Sociodemographic and clinical characteristics between fallers and non-fallers in MCI and AD Groups.
| Variable | MCI group non-faller (n=18) | MCI group faller (n=20) | AD group non-faller (n=18) | AD group faller (n=19) |
|---|---|---|---|---|
| Age (years), M±SD | 74.1±6.5 | 77.3±6.2 | 77±6.2 | 78.1±6.1 |
| Female gender, n (%) | 16 (88.9) | 16 (80.0) | 11 (61.1) | 10 (52.6) |
| Years of schooling, M±SD | 5.7±3.6 | 4.5±4.3 | 5.2±4.8 | 5.8±4.5 |
| Drugs | ||||
| Total number | 5.2±3.9 | 5.1±2.8 | 4.5±1.9 | 5.9±4.1 |
| Use of psychotropic, n (%) | 6 (33.3) | 8 (40.0) | 12 (66.7) | 17 (89.5) |
| Diseases | ||||
| Total number | 2.5±1.2 | 3.3±1.5 | 3.1±1.3 | 3.6±1.0 |
| Diabetes, n (%) | 5 (27.8) | 6 (30.0) | 5 (27.8) | 9 (47.4) |
| Rheumatism, n (%) | 1 (5.6) | 10 (50.0)* | 3 (16.7) | 4 (21.1) |
| Labyrinthitis, n (%) | 2 (11.1) | 3 (15.0) | 1 (5.6) | 2 (10.5) |
| GDS (0–15), M±SD | 2.9±2.2 | 5.0±2.9 | 3.9±3.3 | 3.5±1.9 |
| Minnesota, M±SD | 1863.4±2415.5 | 1200.1±1694.3 | 788.4±1052.4 | 638.3±834.4 |
M±SD, mean±standard deviation; n (%), number of individuals (percentage); MCI, mild cognitive impairment; AD, Alzheimer's disease; GDS, Geriatric Depression Scale; Minnesota, Minnesota Leisure Time Activities Questionnaire.
In the MCI Group, fallers spent a higher time (35.2s), number of steps (33.7 steps) and motor task cost (116%) to perform the TUG-DT compared to non-fallers. In the AD Group, no significant difference was found in dual-task variables between fallers and non-fallers (Table 2).
Dual-task and isolated motor-cognitive task performances between fallers and non-fallers in MCI and mild AD groups.
| Variables (M±DP) | MCI group non-faller (n=18) | MCI group faller (n=20) | AD group non-faller (n=18) | AD group faller (n=19) |
|---|---|---|---|---|
| Isolated motor-cognitive task | ||||
| Time (s) | 19.8±6.9 | 24.2±15.7 | 32.2±11.4 | 29.4±13.9 |
| Errors | 0.1±0.2 | 0.5±1.4 | 3.8±5.2 | 1.6±6.6 |
| TUG-DT | ||||
| Time (s) | 23.4±6.12 | 35.2±17.9* | 39.6±15.6 | 31.7±11.2 |
| Steps | 23.9±6.8 | 33.7±12.6* | 32.1±9.0 | 28.1±7.5 |
| Stops, n (%) | 17 (94.4) | 17 (85.0) | 18 (100.0) | 19 (100.0) |
| Cadence (steps/minute) | 61.9±10.8 | 60.2±12.3 | 52.4±15.6 | 55.1±9.8 |
| Errors | 0.9±1.9 | 0.8±1.6 | 3.9±4.8 | 1.6±2.87 |
| Correct response/time | 0.3±0.1 | 0.2±0.1 | 0.1±0.1 | 0.2±0.1 |
| Motor task cost (%) | 85.6±28.6 | 116.0±49.3* | 117.7±66.0 | 111.5±48.6 |
| Cognitive task cost (%) | 32.5±21.7 | 35.3±19.2 | 24.6±34.1 | 31.8±28.2 |
MM±SD, mean±standard deviation; n (%), number of individuals (percentage); MCI, mild cognitive impairment; AD, Alzheimer's disease; TUG-DT, timed up and go dual-task test.
Regarding univariate predictors (adjusted for a positive diagnosis of rheumatism), falls in the MCI Group were significantly associated with higher time, increased number of steps and higher motor task cost when performing the TUG-DT (Table 3). After the inclusion of these variables in the multivariate logistic regression model, only the number of steps was identified as an independent predictor of falls (OR [95% CI]=1.13 [1.01–1.26]) and the model used was able to explain falls in 51.4% (positive likelihood ratio=70%, negative likelihood ratio=78%). A cutoff score of 23.88seconds in TUG-DT performance had a 61% specificity and a 80% sensitivity to predict falls in the MCI Group (area under the curve=77.2%) (Table 4). Moreover, a number of steps higher than 29.50 had a 83% specificity and a 65% sensitivity to predict falls (area under the curve=76.5%).
Univariate predictors of falls in older people with MCI and mild AD using dual-task and isolated motor-cognitive task measures.
| Variables | MCI Group (n=20) | AD Group (n=19) | ||
|---|---|---|---|---|
| P Value | OR (95% CI) | P Value | OR (95% CI) | |
| Isolated motor-cognitive task | ||||
| Time (s) | 0.27 | 1.04 (0.97–1.13) | 0.49 | 0.98 (0.93–1.03) |
| Errors | 0.53 | 1.72 (0.31–9.62) | 0.29 | 0.93 (0.81–1.06) |
| TUG-DT | ||||
| Time (s) | 0.02* | 1.15 (1.01–1.30) | 0.09 | 0.95 (0.90–1.00) |
| Steps | 0.02* | 1.13 (1.01–1.26) | 0.15 | 0.94 (0.86–1.02) |
| Stops, n (%) | 0.22 | 1.55 (0.76–3.14) | ||
| Cadence (steps/minute) | 0.71 | 0.98 (0.92–1.05) | 0.52 | 1.01 (0.96–1.07) |
| Errors | 0.13 | 0.44 (0.15–1.26) | 0.09 | 0.85 (0.71–1.02) |
| Correct response/time | 0.23 | 0.01(0.00–15.50) | 0.06 | 123.07 (0.78–19233.43) |
| Motor task cost (%) | 0.04* | 1.02 (1.00–1.04) | 0.74 | 0.99 (0.98–1.01) |
| Cognitive task cost (%) | 0.29 | 0.97 (0.93–1.02) | 0.48 | 1.00 (0.98–1.03) |
n (%), number of individuals (percentage); MCI, mild cognitive impairment; AD, Alzheimer's disease; TUG-DT, dual-task test; OR (95% CI), odds ratio (95% confidence interval).
In the AD Group, no dual-task variable was able to predict falls (Table 3). Therefore, it was not possible to establish a cutoff score for the tool applied.
DiscussionThis study aimed to verify whether the TUG-DT could predict falls in community-dwelling older people with MCI or AD in the mild stage. The TUG-DT predicted falls only in MCI, with higher number of steps significantly and independently associated with falls. In accordance with the Alzheimer's Association,21 the sample was composed of subjects aged 70–80 years old, a higher prevalence of women, and subjects using psychotropic drugs. Regarding the high prevalence of rheumatic conditions in fallers with MCI, Arnold and Faulkner22 found that older people with rheumatic diseases, such as knee osteoarthritis, were at risk of falls due to gait disturbances. Also, radiographic incidence of knee osteoarthritis has been shown to be five times more common in older adults with MCI compared to healthy people.23 Thus, the association between these comorbidities and MCI can increase the occurrence of falls.
In the present study, 53% MCI and 51% mild AD fell during the 6-month follow up. Taylor et al.2 also found a high prevalence of falls (54%) in cognitively impaired older people during a 1-year follow up. Some deficits could explain the occurrence of falls in cognitively impaired older people, including MCI and AD, such as decreased muscle strength, increased reaction time, balance disorders, and neuropsychological factors (e.g. use of psychotropic drugs, presence of depressive symptoms).2,24
In the MCI Group, fallers and non-fallers presented significant differences in time, number of steps and motor task cost spent on the TUG-DT, and these variables were identified as univariate predictors of falls. Montero-Odasso et al.7,25 verified that older people with MCI demonstrated normal mobility in simple tasks, but they exhibited more instability and slower gait speed compared to healthy older people in dual-task situations. The worse mobility performance in dual-task activities could be related to a decline in executive functions and possible control by common specific cortical areas (i.e., prefrontal, parietal and premotor areas). Also, the authors suggested that people with MCI had an increased risk of falls when they were exposed to a cognitive challenge while walking.7,25 Similarly, Taylor et al.4 assessed gait associated with a motor task of carrying a cup of water and gait associated with a cognitive task of counting backward in cognitively impaired older people. Fallers showed worse performance in the dual-task involving the cognitive secondary task compared to non-fallers, with slower gait speed, shorter stride length, and a higher support base.
A time greater than 23.88s to complete the TUG-DT predicted risk of falls in the MCI Group (sensitivity=80%), while a number of steps (i.e., less than 29.50 steps) was able to identify people without risk of falls (specificity=83%). Thus, it is important to use the two measures of TUG-DT to predict falls in older people with MCI. To our knowledge, other studies that assessed dual-task and falls in older adults with MCI did not establish cutoff scores for predicting falls,7,10 which is a strong point of the present study.
Amboni et al.26 verified that risk of falls during dual-task activities was proportional to the degree of cognitive impairment. However, in the present study, AD fallers and non-fallers did not present differences in the TUG-DT performance and the test was not able to predict falls in the mild AD Group. In dual-task situations, the simultaneously performed tasks interfered and competed for attention and brain cortical resources, which could result to changes in one or both tasks.25 Older people with mild AD demonstrated worse performance in a dual-task test when compared to MCI subjects, and people with preserved cognition.10 In the present study, both AD fallers and non-fallers presented impairment in the TUG-DT performance. Falls in AD Group are linked to an interaction of multiple systems and risk of falls was associated with intrinsic and extrinsic factors linked to primary cognitive impairment, such as gait unsteadiness, variability of stride timing, executive dysfunction, and use of drugs.5 Therefore, the mobility analysis is not able to predict falls in AD subjects, as several risk factors could have acted together to cause these events.
The findings of the present study show the importance to prevent falls even in older people with slight cognitive impairments. The TUG-DT can be used to facilitate the screening of risk of falls in older people with MCI and maybe to target interventions involving dual-task activities. Furthermore, multifactorial strategies to screen and to prevent falls is needed in older people with mild AD.
This study has some limitations, including the non-random sampling, the non-differentiation of MCI types due to difficult of diagnosis and recruitment, and the lack of control over the familiarization with the phone model. On the other hand, a prospective study about falls, testing and follow-up procedures was conducted and we used a common and daily secondary task. Other studies including people with MCI or AD used non-functional secondary cognitive tasks to assess risk of falls.2,4,7,27
In conclusion, community-dwelling older people with MCI (CDR=0.5) and mild AD (CDR=1) presented with a similar prevalence of falls. The TUG-DT test was able to differentiate MCI fallers from non-fallers, and could be useful as a screening tool for risk of falls in older people with MCI, using cutoff scores of 23.88s and 29.50 steps. Future research with dual-task tests involving functional secondary tasks associated with other potential risk factors are needed to predict falls in older people with mild AD.
Conflicts of interestThe authors have no conflicts of interest to declare.
This study was supported by the Coordination for the Improvement of Higher Education Personnel (CAPES). The sponsor had no involvement in the study design, in the collection, analysis and interpretation of data.