To evaluate the effect of three types of exercise intervention in patients with patellofemoral pain and to verify the contributions of each intervention to pain control, function, and lower extremity kinematics.
MethodsA randomized controlled, single-blinded trial was conducted. Forty women with patellofemoral pain were randomly allocated into four groups: hip exercises, quadriceps exercises, stretching exercises and a control group (no intervention). Pain (using a visual analog scale), function (using the Anterior Knee Pain Scale), hip and quadriceps strength (using a handheld isometric dynamometer) and measuring lower limb kinematics during step up and down activities were evaluated at baseline and 8 weeks post intervention.
ResultsAll treatment groups showed significant improvements on pain and Anterior Knee Pain Scale after intervention with no statistically significant differences between groups except when compared to the control group. Only hip and quadriceps groups demonstrated improvements in muscle strength and knee valgus angle during the step activities.
ConclusionHip strengthening exercises were not more effective for pain relief and function compared to quadriceps or stretching exercises in females with patellofemoral pain. Only hip and quadriceps groups were able to decrease the incidence of dynamic valgus during step-down activity. This study was approved by Brazilian Clinical Trials Registry registration number: RBR-6tc7mj (http://www.ensaiosclinicos.gov.br/rg/RBR-6tc7mj/).
Patellofemoral pain (PFP) is a prevalent clinical condition that is very commonly observed in orthopedic practice.1–4 Dysfunctions in the patellofemoral joint are especially common among physically active young adults, with a 2.2 times higher prevalence in women, although it occurs frequently in men as well.5,6 Symptoms related to PFP include pain associated with movement, particularly with activities such as kneeling, ascending and descending stairs, running and squatting.7
The rehabilitation of these patients is increasingly important, as 45% of those with PFP may suffer from osteoarthritis with advanced age8 and 22% of individuals who have undergone unicompartmental arthroplasty of the knee reported a history of PFP at a younger age.9
In recent years, the role of hip stabilizers has been the object of several studies and rehabilitation protocols.10–13 Patients with PFP often present with pelvic misalignment and increased internal rotation of the femur during the execution of functional activities, such as ascending and descending stairs that are functionally two of the most painful movements of daily living for patients with PFP.14
The theory about the changed position of patella not being caused solely by quadriceps imbalance, but by changing position of the femur in closed kinetic chain activities due to a hip weakness gained strength and it has been hypothesized that the cause of PFP include exercises to the hip and pelvis which would be the key to satisfactory clinical outcomes for PFP patients.15 Thus, strengthening of hip stabilizing muscles, especially the abductors and lateral rotators, as indicated by Powers,15 has changed the opinion and conduct of treatment proposed by clinicians and researchers.
It has not been established which type of conservative treatment is more effective because the majority of studies have used different groups of treatment with a common protocol of exercises to all groups or the association of different types of exercise in the same protocol.16–18 Other studies have proposed the strengthening of the same muscle group, distinguishing only the method of performance.19–21 Besides, no studies were found that assessed the effect of stretching exercises alone, only those that included stretching muscle groups that were common to all groups of treatment.18,21,22 So we do not know what the real effect, in an isolated way, that a treatment based solely on stretching exercises can bring to individuals with PFP. Thus, no study has evaluated each form of treatment in an isolated way, without any combination of then.
There are currently seven prospective randomized controlled trials in the literature that have investigated the inclusion of hip and pelvic muscle strengthening for PFP12,18,20,23–26 patients, but the conclusions of these studies regarding the benefits of proximal muscles strengthening are questionable. Because common exercises for hip and quadriceps, as well as stretching were associated in these protocols, and results were either only compared to no intervention groups26 or included exercises to strengthen adductor muscles, contrary to idea of strengthening abductors and external rotators in order to stabilize the pelvis.23,27 However the design of these studies was based on the knowledge available at the time of those studies.12,20,25
Thus, our purpose was to evaluate the contribution of three types of individual interventions, in patients with PFP and to verify the contributions of each one in terms of decreasing pain, and improving function and lower extremity kinematics.
MethodsA 4arm, randomized controlled assessor-blinded trial was performed.
PatientsForty recreational female athletes between the ages of 18 and 28 years with PFP were selected from the university campus and randomly assigned to groups for treatments. A recreational athlete was defined as anyone participating in aerobic or athletic activity at least 3 times per week for at least 30min.23
Subjects were included in the study if they were female and had anterior knee pain with a minimum intensity of 3 or greater on the 10-cm visual analog scale (VAS)1,23 for at least three months before the study assessment. Additional inclusion and exclusion criteria were followed according to Nakagawa et al.28 Inclusion criteria: (1) insidious onset of symptoms; (2) retropatellar or peripatellar pain with at least 2 of the following activities (ascending/descending stairs, running, kneeling, squatting, prolonged sitting or jumping). Exclusion criteria: (1) previous history of knee surgery; (2) history of back, hip, or ankle joint injury or pain; (3) patellar instability; (4) lesion or pain during palpation or test of any structure of knee and (6) any neurological involvement that would affect gait.
Of the 40 volunteer subjects included in the project, all subjects first underwent a physical, kinematic, and strength assessment. This study and the informed consent form related to this same study were approved by the Ethics Committee of the Ribeirão Preto Medical School, Universidade de São Paulo (USP), Ribeirão Preto, SP, Brazil (reference number: 10371/2010). All volunteers read and signed the informed consent document.
This study was prospectively registered in the Brazilian Clinical Trials Registry (REBEC), registration number: RBR-6tc7mj.
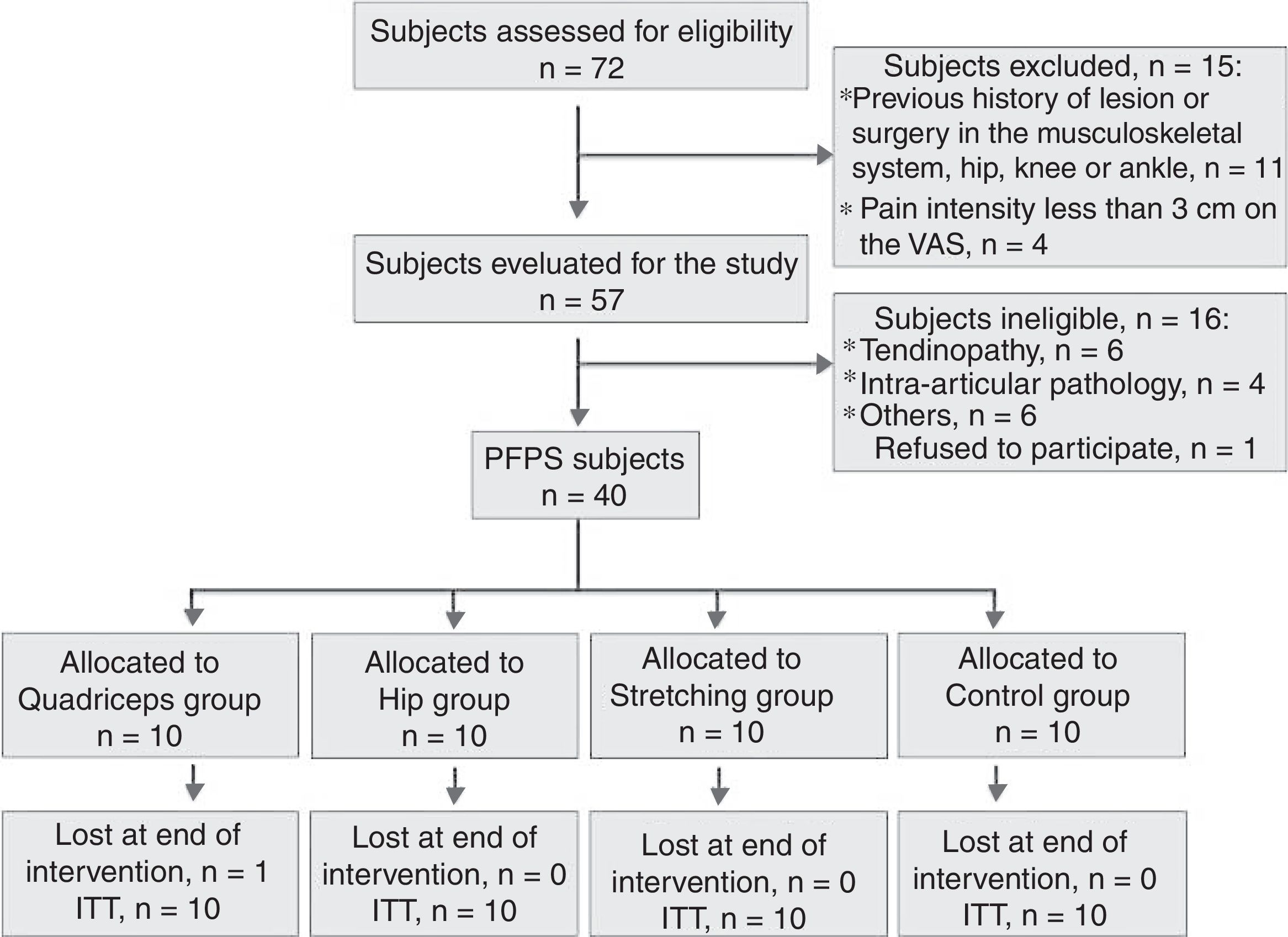
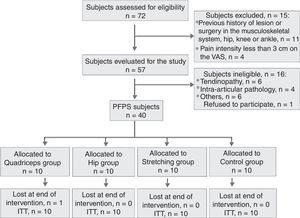
RandomizationThe PFP subjects were randomly allocated to one of four groups: quadriceps strengthening group (QG), hip strengthening group (HG), stretching group (SG) or a control group (CG) (no treatment). The randomization schedule was generated using R 2.7.2 statistical software. The allocation was concealed by the use of consecutively numbered, sealed and opaque envelopes (Fig. 1).
Outcome measuresAll kinematic assessments were performed by RFL (author), who had at least 4 years experience doing these procedures. Only LVOM, MSBM and RFL (authors) were blinded to the group allocation, because MCS (author) provided all treatments to the groups. LVOM and MSBM were also responsible for the administration of the questionnaires, intensity of pain assessment and muscle strength assessment tests.
There were two evaluations. The initial and final evaluation post 8 weeks consisted of an assessment of pain,29 a functional questionnaire,2 assessment of muscle strength through a handheld isometric dynamometer,30,31 and dynamic valgus were assessed during functional activities (ascending and descending stairs).
PainIntensity of pain, the primary endpoint of our study, was assessed using a visual analog scale (VAS) on a 10cm scale, where 0 indicated “no pain” and 10 indicated “worst possible pain”. This scale is considered a reliable, valid, and responsive method to examine individuals with PFP.29
FunctionPhysical function was assessed by an Anterior Knee Pain Scale (AKPS),2 which is a specific questionnaire for individuals with PFP. This tool is valid for individuals with PFP and has proved to be highly reliable in test-retest,29 in addition, it was translated, adapted, and validated in Brazil.2
KinematicsFor kinematic data analysis, the Qualisys®Pro-Reflex video camera system32 with six infrared video cameras was used, which allowed for the reconstruction in 3D of passive reflective markers located at specific bony prominences (i.e. hip, knee, and ankle).16 The frequency of data capture was 120Hz, and standard deviation errors below 10mm were allowed during the initial calibration.
Participants were asked to ascend and descend a three-step stair at normal speed, simulating a usual everyday situation. The mean values obtained from three ascending and descending attempts were used for statistical analyses.
Dynamic valgus was measured in the frontal-plane at 45 degrees of tibiofemoral flexion because this was the best moment to assess the valgus, and altered patterns of movement could be exacerbated in this position.33,34
Strength evaluationUsing a load cell (KRATOS®) adapted (handheld dynamometer) to a digital reader, the isometric muscle strength of the hip abductors (gluteus medius), adductors, lateral rotators, medial rotators, and hip extensors (gluteus maximus) and flexors (iliopsoas and rectus femoris) was measured. For knee extensors (quadriceps) and flexors (hamstrings), the load cell was adapted and fixed with chains to a flexor-extensor machine and the MVC isometric muscle strength was measured in a favorable position30,35–37,60 and properly stabilized with a belt so as to avoid any possible influence by the examiner. The values were normalized to each individual's body mass.
InterventionsPatients included in the treatment groups participated in two sessions per week for eight weeks with a minimum break of 24h between sessions. Individuals were asked and requested not to perform exercises outside the program and all treatment sessions were performed in the university's posture and human movement analysis laboratory (LAPOMH). Each treatment session was approximately 50min in duration, and all sessions were performed individually and supervised by the same physical therapist. For all groups of treatment the weights were increasing as the patient's reported changes in their following the Rating of Perceived Exertion (RPE) scale38 based on Borg's Scale of effort.39 This is common method used to assess the intensity of exercise and this scale has been used and researched for its use in both clinical and exercise settings.39,40 The exercises chosen for each group should strengthen the muscles of the hip & knee & lead to increased stabilization of the hip & knee joints:
- -
Quadriceps strengthening group (QG). The exercises in this group focused specifically on quadriceps strengthening (see Appendix A).
- -
HIP strengthening group (HG). This group performed exercises to strengthen hip stabilizing muscles (see Appendix B).
- -
Stretching group (SG). In this group, the physical therapist monitored and stabilized the patients during the stretching exercises for all muscles involved in knee and hip stabilization (see Appendix C).
- -
Control group (CG). Patients included in this group did not have any kind of intervention for eight weeks, but they were tested at the start of the program & at the end like the other 3 groups. At the end of the experiment, a rehabilitation program was made available to all patients.
Sample size calculation: forty PFP patients (10 in each group) were needed to provide 80% power, based on a 1-sided test, type I error of 0.05, standard deviation of 1.8 (from prior data), and the ability to detect a 3-cm between-group difference in pain intensity based on a 10-cm VAS.23
A linear regression model with mixed effects (i.e. random and fixed) was used. Mixed-effect linear models are used in the analysis of data in which the answers are grouped (i.e. repeated values for the same individual) and the assumption of independence of observations within a group is not adequate.41 A significance level of 5% was defined.
For analysis of dynamic valgus, a qualitative analysis of data was chosen, which was performed using the McNemar's test,42 and which aimed to assess the real effect of a therapeutic intervention within treatment groups; results are expressed in absolute values and a percentage.
All participants attended all treatment sessions except the quadriceps group that computed a loss. For the quadriceps group, the statistical analysis took into account the loss of one individual from the group. An intention-to-treat (ITT) analysis approach was carried out. The missing data was dealt with by using a multiple imputation.43 In addition, a “per protocol” analysis was also performed using patients with complete data only. For statistical analysis, only the symptomatic leg was considered.
Clinical relevanceIn order to assess clinical relevance, the MCID (minimal clinically important difference) was performed and an average improvement exceeding the minimum of 2cm on the VAS is considered clinically relevant.29
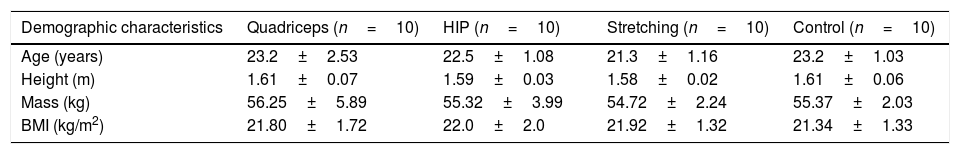
ResultsTable 1 summarizes the demographic characteristics of the groups at the baseline.
Female patient demographics for muscle strengthening & stretching in PFP patients at baseline.
| Demographic characteristics | Quadriceps (n=10) | HIP (n=10) | Stretching (n=10) | Control (n=10) |
|---|---|---|---|---|
| Age (years) | 23.2±2.53 | 22.5±1.08 | 21.3±1.16 | 23.2±1.03 |
| Height (m) | 1.61±0.07 | 1.59±0.03 | 1.58±0.02 | 1.61±0.06 |
| Mass (kg) | 56.25±5.89 | 55.32±3.99 | 54.72±2.24 | 55.37±2.03 |
| BMI (kg/m2) | 21.80±1.72 | 22.0±2.0 | 21.92±1.32 | 21.34±1.33 |
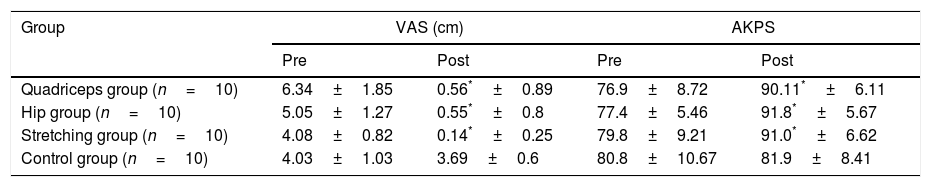
VAS revealed that, except for the CG, all groups had improvements in post-treatment period. Between-group comparison showed no differences between treatment groups after the 8 week exercise period and all groups showed better performance than the CG (Table 2).
Pain (VAS) pre and post treatment. Anterior Knee Pain Score (AKPS) pre and post treatment for female PFP patients. Final criteria for clinical relevance on pain results based on MCID to the treatment groups and final results comparison between treatment group.
| Group | VAS (cm) | AKPS | ||
|---|---|---|---|---|
| Pre | Post | Pre | Post | |
| Quadriceps group (n=10) | 6.34±1.85 | 0.56*±0.89 | 76.9±8.72 | 90.11*±6.11 |
| Hip group (n=10) | 5.05±1.27 | 0.55*±0.8 | 77.4±5.46 | 91.8*±5.67 |
| Stretching group (n=10) | 4.08±0.82 | 0.14*±0.25 | 79.8±9.21 | 91.0*±6.62 |
| Control group (n=10) | 4.03±1.03 | 3.69±0.6 | 80.8±10.67 | 81.9±8.41 |
| VAS | Between-group postMean difference | 95% confidence interval | p | Final criteria | |
|---|---|---|---|---|---|
| HG×QG | −0.12 | −1.03 | 0.79 | 0.79 | NCR |
| HG×SG | −0.41 | −1.30 | 0.48 | 0.36 | NCR |
| HG×CG | 3.14 | 2.25 | 4.03 | <0.01 | CR |
| QG×SG | −0.53 | −1.44 | 0.38 | 0.24 | NCR |
| QG×CG | 3.02 | 2.11 | 3.93 | <0.01 | CR |
| SG×CG | −3.55 | −4.44 | −2.66 | <0.01 | CR |
HG, hip group; QG, quadriceps group; SG, stretching group; CG, control group; CR, clinically relevant; NCR, not clinically relevant.
All treatments groups had a significant MCID for pain outcomes at the end of 8 week exercise program, except the CG. Between-group comparisons were performed in order to compare which treatment protocol was more effective and none of the three groups had a greater treatment effect than the other two except when compared to the CG (Table 2).
FunctionFor between-group comparison questionnaire scores pre and post-treatment, all groups except the CG improved their scores (p<0.01). No difference was found between the 3 treatment groups. All 3 groups showed better performance than the CG (Table 2).
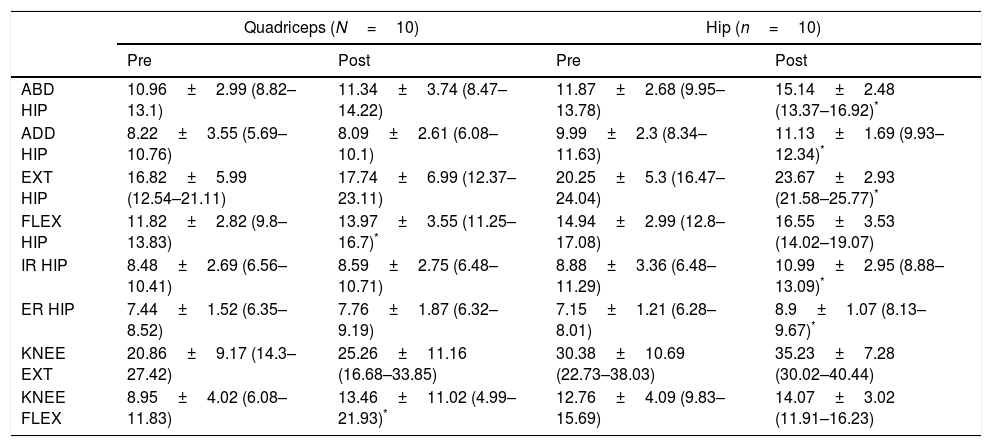
StrengthThe post-treatment period revealed strength improvement for HG (i.e. hip abductors, adductors, internal/external rotators and extensors); QG (hip and knee flexors); CG (decrease hip extensors); SG (no significant changes) (Table 3).
Pre and post treatment effects on muscle strength (Kgf) for female PFP patients.
| Quadriceps (N=10) | Hip (n=10) | |||
|---|---|---|---|---|
| Pre | Post | Pre | Post | |
| ABD HIP | 10.96±2.99 (8.82–13.1) | 11.34±3.74 (8.47–14.22) | 11.87±2.68 (9.95–13.78) | 15.14±2.48 (13.37–16.92)* |
| ADD HIP | 8.22±3.55 (5.69–10.76) | 8.09±2.61 (6.08–10.1) | 9.99±2.3 (8.34–11.63) | 11.13±1.69 (9.93–12.34)* |
| EXT HIP | 16.82±5.99 (12.54–21.11) | 17.74±6.99 (12.37–23.11) | 20.25±5.3 (16.47–24.04) | 23.67±2.93 (21.58–25.77)* |
| FLEX HIP | 11.82±2.82 (9.8–13.83) | 13.97±3.55 (11.25–16.7)* | 14.94±2.99 (12.8–17.08) | 16.55±3.53 (14.02–19.07) |
| IR HIP | 8.48±2.69 (6.56–10.41) | 8.59±2.75 (6.48–10.71) | 8.88±3.36 (6.48–11.29) | 10.99±2.95 (8.88–13.09)* |
| ER HIP | 7.44±1.52 (6.35–8.52) | 7.76±1.87 (6.32–9.19) | 7.15±1.21 (6.28–8.01) | 8.9±1.07 (8.13–9.67)* |
| KNEE EXT | 20.86±9.17 (14.3–27.42) | 25.26±11.16 (16.68–33.85) | 30.38±10.69 (22.73–38.03) | 35.23±7.28 (30.02–40.44) |
| KNEE FLEX | 8.95±4.02 (6.08–11.83) | 13.46±11.02 (4.99–21.93)* | 12.76±4.09 (9.83–15.69) | 14.07±3.02 (11.91–16.23) |
| Stretching (N=10) | Control | |||
|---|---|---|---|---|
| Pre | Post | Pre | Post | |
| ABD HIP | 13.02±6.02 (8.71–17.33) | 13.29±5.45 (9.4–17.19) | 12.06±3.58 (9.5–14.62) | 11.4±3.22 (9.1–13.7) |
| ADD HIP | 9.61±4.43 (6.44–12.78) | 9.62±4.57 (6.36–12.89) | 9.32±1.43 (8.3–10.34) | 8.77±1.68 (7.57–9.97) |
| EXT HIP | 19.3±7.57 (13.88–24.71) | 21.25±8.33 (15.29–27.21) | 22.74±6.03 (18.43–27.05) | 19.76±6.18 (15.34–24.19)* |
| FLEX HIP | 14.6±4.95 (11.06–18.14) | 15.02±4.49 (11.81–18.23) | 13.42±3.29 (11.07–15.77) | 13.42±4.03 (10.54–16.3) |
| IR HIP | 9.61±4.18 (6.63–12.6) | 10.4±4.18 (7.41–13.39) | 10.0±2.14 (8.47–11.53) | 9.14±1.86 (7.81–10.48) |
| ER HIP | 8.03±3.49 (5.53–10.52) | 8.15±2.86 (6.1–10.2) | 7.72±1.27 (6.81–8.62) | 7.09±1.61 (5.94–8.25) |
| KNEE EXT | 32.07±13.56 (22.37–41.77) | 31.85±15.26 (20.93–42.77) | 39.71±9.54 (32.89–46.53) | 36.76±10.44 (29.29–44.22) |
| KNEE FLEX | 14.15±7.08 (9.08–19.21) | 13.71±5.07 (10.09–17.34) | 12.53±3.46 (10.06–15.01) | 11.39±2.98 (9.26–13.53) |
ABD HIP, abductors of hip; ADD HIP, adductors of hip; EXT HIP, extensors of hip; FLEX HIP, flexors of hip; IR HIP, internal rotators of hip; ER HIP, external rotators of hip; KNEE EXT, knee extensors; KNEE FLEX, knee flexors.
Values are mean±SD; Values in parentheses are 95% confidence interval.
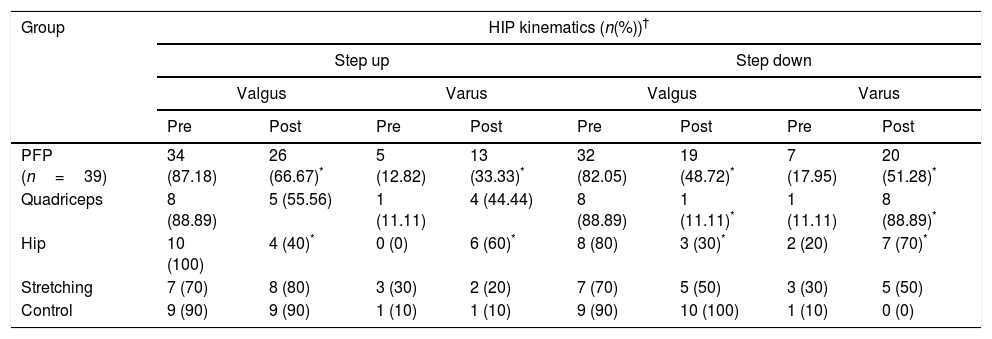
Step-down: The QG and HG had improvement in movement patterns in the post-treatment testing. The HG had 80% of individuals with a valgus knee alignment and 20% varus pattern pre-treatment. Post-treatment, 30% of individuals still had a valgus alignment whereas 70% presented with a varus pattern. For the QG, 88.89% of individuals had a knee valgus alignment and 11.11% had a varus pattern pre-treatment. Post-treatment: only 11.11% of subjects still had a valgus alignment whereas 88.89% showed a varus pattern. For the step-up, only the HG had improvement. Pre-treatment, 100% had a knee valgus pattern. Post-treatment, 40% still had this pattern and 60% showed a knee varus pattern (Table 4).
Pre and post treatment effects on lower limb kinematics for female PFP patients.
| Group | HIP kinematics (n(%))† | |||||||
|---|---|---|---|---|---|---|---|---|
| Step up | Step down | |||||||
| Valgus | Varus | Valgus | Varus | |||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | |
| PFP (n=39) | 34 (87.18) | 26 (66.67)* | 5 (12.82) | 13 (33.33)* | 32 (82.05) | 19 (48.72)* | 7 (17.95) | 20 (51.28)* |
| Quadriceps | 8 (88.89) | 5 (55.56) | 1 (11.11) | 4 (44.44) | 8 (88.89) | 1 (11.11)* | 1 (11.11) | 8 (88.89)* |
| Hip | 10 (100) | 4 (40)* | 0 (0) | 6 (60)* | 8 (80) | 3 (30)* | 2 (20) | 7 (70)* |
| Stretching | 7 (70) | 8 (80) | 3 (30) | 2 (20) | 7 (70) | 5 (50) | 3 (30) | 5 (50) |
| Control | 9 (90) | 9 (90) | 1 (10) | 1 (10) | 9 (90) | 10 (100) | 1 (10) | 0 (0) |
Regarding pain and function, our results showed that the three most common forms of treatment for PFP patients, with focus on quadriceps strengthening, strengthening and stabilization of the hip, and stretching were equally effective and no significant differences were observed among them. These results confirmed previous clinical trials that showed that treatment, regardless of the physical intervention applied, could be beneficial to PFP individuals.18,19,44–49
Our results confirmed that prescription of stretching exercises relieved pain and increased function similarly to effects of strengthening programs and stabilizing hips and knees for PFP patients. Reduced hamstring length can result in increased stress on the patellofemoral joint,50 thus, increased flexibility might prevent the development of such pathologies as PFP.16,51 Our study is the first to analyze, in an isolated way, the role of muscle stretching in PFP individuals, and the results suggested that stretching exercises were equally effective for pain relief and functional improvements in PFP patients.
Recently, Khayambashi et al.,12 in a comparative study, concluded that hip strengthening was better than quadriceps strengthening but the quadriceps group were exercised using different isometric angles that were not protective and increased the stress to patellofemoral joint52 and used strengthening exercises combined with the strengthening hip adductors that is completely contrary to idea of strengthening hip abductors and external rotators to help stabilize the pelvis.15 The study design led to a bias toward positive results for the group undergoing hip strengthening. However, Rathleff et al.,53 in a systematic review, found no association between weakness of the hip muscles and the development of PFP, therefore reduced hip strength could be a result and not the cause of PFP. Rabelo and Lucareli54 agreed with this hypothesis. In two other systematic reviews performed by Lack et al.55 and Santos et al.,56 it was observed that the strengthening of proximal structures (hip) combined with quadriceps strengthening, showed strong evidence of improvement in pain(decreased) and function(improved) in the short term, but with no evidence of improvement or superiority in the long term when compared to isolated quadriceps strengthening. These reviews showed that hip muscle strengthening was effective in reducing the intensity of pain and improving functional capabilities in patients with PFP, despite the lack of evidence for its ability to increase muscle strength.
Our study had the objective of completely differentiating the treatment groups, so none of the protocols had any exercises in common, to assess the real effect of specific exercises. In previous studies, some protocols often used exercises that were common to different protocols.16–18,23 Others focused on one muscle group and distinguished only the way the strengthening was carried out,19–21 or included stretching exercises for muscle groups that were common to all treatment groups.18,21,22 Therefore, the question is whether the improvement observed could have occurred as a result of a specific exercise for strengthened muscle, regardless of the way it was strengthened, or whether this improvement occurred due to the common stretching exercises proposed. As a consequence, this possibly resulted in no significant differences being observed between treatments.
The qualitative analysis of movement showed at baseline that PFP individuals had a valgus movement pattern of around 87.18% and 82.05% during step-up and step-down, respectively. At the end of the intervention period, these values decreased to 66.67% and 48.72% respectively. Stratifying into subgroups, only the HG and QG had significant improvements at the end of the 8 weeks intervention period. Step-up had a greater incidence of dynamic valgus, agreeing with a previous study57 that showed step-up was more unstable for PFP individuals and could intensify altered movement patterns.
Recent studies reported that strengthening proximal structures could alter incorrect patterns of movements that resulted in excessive dynamic valgus and consequently increased pain in PFP patients. However, these were conceptual statements and kinematics were not assessed.11,15,24,26,33 Herman et al.58 and Earl and Hoch27 also reported that individual hip strengthening exercises did not alter movement patterns. Recently, an exercise program proposed by Baldon et al.23 was able to change movement patterns in PFP individuals, agreeing with our results. Our study also found that only the strengthening groups (i.e. HG and QG) had significant improvement in their movement patterns. Nevertheless, despite this improvement in the HG and QG, results in pain and function did not show greater improvement than those in the SG.
In the assessment of muscle strength, only the HG had significant improvement in almost all muscle groups of the hip (i.e. abductors, adductors, extensors, and internal and external rotators). This difference was probably due to the joint position at the moment of evaluation because muscles such as the gluteus maximus and medius which are lateral rotators in the orthostatic position, and anterior fibers of these muscles become medial rotators in the sitting position (i.e. the position chosen during the strength test).59 The QG showed strength improvement only for hip flexors and knee flexors. This can be explained by the strengthening of the quadriceps themselves, which act as a biarticular muscle that also facilitates hip flexion.59
All groups that received any kind of treatment showed statistical and clinically relevant results in pain relief at the end of the 8 week intervention period, with average improvement greater than the minimum clinically important difference (MCID) for pain of 2cm VAS.29 At the conclusion of the 8 week intervention period, in order to compare which protocol of treatment was more effective, final results for pain were compared and no group was superior to the others except when compared to the control group that received no treatment.
Above all, the present study highlighted the benefits of physiotherapy treatment that, regardless of the form of intervention, contribute to relieve pain, either by stabilizing and strengthening the hip and quadriceps muscles, or by improving the flexibility of the structures involved. No studies were found in the literature that compared individual treatment protocols to completely different ones, as was done in this study. Some more recent studies have stated that an association of programs would be even more beneficial to patients with PFP than an isolated program that focuses on only one type of treatment. Thus, the most indicated and effective rehabilitation for each individual should be based on the deficits observed in the initial evaluation of each individual.
LimitationsOur study had some limitations. First, despite the large number of total patients with PFP, the stratified treatment groups were eventually small; nevertheless, sample calculation allowed us to use this number of individuals. Second, participants’ baseline characteristics seemed to be different, especially for pain, probably as a consequence of low number of participants. Third, the current findings should not be extrapolated to males with PFP, as only women participated in this study. And third, 8 weeks was a short time for a follow-up but we know that this is a period that we can already observe pain relief in these patients.12,23
ConclusionHip strengthening exercises was no more effective on pain and function compared to quadriceps exercises or stretching exercises in females with PFP. Both hip and quadriceps strengthening exercises improved lower extremity kinematics after 8 weeks of intervention.
Conflicts of interestThe authors declare no conflicts of interest.
This study received financial support of The State of São Paulo Research Foundation – FAPESP (process number: 2010-/12561-9).