Diabetes mellitus (DM) and diabetic peripheral neuropathy (DPN) compromises the structures of the musculoskeletal system, especially in the foot-ankle complex. Foot-related exercises can be a promising tool to be incorporated in health care programs to manage and prevent musculoskeletal complications resulting from DM and DPN progression.
ObjectiveTo present the development, validation, and usability evaluation of a booklet that directs training and personalizes the progression of a home-based program of foot-ankle exercises.
MethodsThe booklet containing a foot-ankle exercise program developed in a previous clinical trial was validated using the Delphi technique, with a multi-professional jury of experts who assessed the content of the material, language, individual education, exercise execution, exercise quality, and material implementation. The validated version was evaluated through telephone interview by a convenience sample of 10 individuals with DPN regarding its relevance, health education, comprehension, and usability.
ResultsThe validation process with experts was performed in two rounds achieving 100% agreement in the second round. During the usability evaluation process the main complaint of users was that performing all the exercises was very tiring and took too much time out of their daily routine. Thus, the number of repetitions for each exercise was changed from 30 to 12.
ConclusionThe booklet is a material for prevention and management of the impacts of DM and DPN progression by improving the musculoskeletal function of the foot-ankle. This material provides an exercise regime with a personalized progression based on the perceived effort of the users.
In 2019, it was estimated that 9.3% of the adult world population was living with diabetes mellitus (DM) and the expectation is that the prevalence will increase to 10.2% by 2030.1 Among the main complications of DM is diabetic peripheral neuropathy (DPN) that has a prevalence from 16% to 87% of the DM population.2
DPN compromises the structures of the musculoskeletal system, especially in the foot-ankle complex, leading to decreased strength of the extrinsic and intrinsic muscles,3–7 decreased ankle range of motion,8 and changes in the mechanical properties of the Achilles tendon.9 These complications are responsible for some of the disabilities shown by this population, especially in mobility, due to changes in gait dynamics10,11 and balance.12 Additionally, loss of foot-ankle mobility is considered an important risk factor for foot ulceration.13–15
There is evidence of improvements in foot-ankle structure and function16,17 and of changes in DPN symptoms18,19 in individuals who performed foot-related exercises. Therefore, exercise can be a promising rehabilitation tool to be incorporated in health care programs to manage and prevent musculoskeletal complications resulting from DM and DPN progression. Recently, foot-ankle therapeutic exercises have become part of the international guideline recommendations to help mitigate risk factors and preventing foot ulceration in people at risk, although the quality of the evidence is still low.20
There are several resources that guide foot care and the importance of practicing regular physical activity.21–24 Although feet are the most affected body segment by DM and DPN long-term complications, there are no specific material focusing on teaching foot-related exercises for deficits management and prevention. With the intention of incorporating the practice of specific foot exercises in daily lives, the development of an educational material to be used at home to motivate learning and provide guidance to people with DM is crucial.
The aim of this study was to develop, validate, and evaluate the usability of a booklet that, in addition to informing about DM and DPN, directs the training and customizes the progression of a home-based program of foot-related exercises targeting the main musculoskeletal impairments related to DM.
MethodsThis study had two-phases: (i) booklet development; and (ii) validation of the booklet's content by experts and evaluation of its usability by users. All participants, both users and experts, were Brazilian and signed an informed consent form after agreeing to participate. The study was approved by the Research Ethics Committee of Universidade de São Paulo, SP, Brazil (CAAE: 90331718.4.0000.0065).
Booklet developmentThe booklet development included foot care recommendations and information about DM and DPN, and a customized program of foot–ankle exercises.
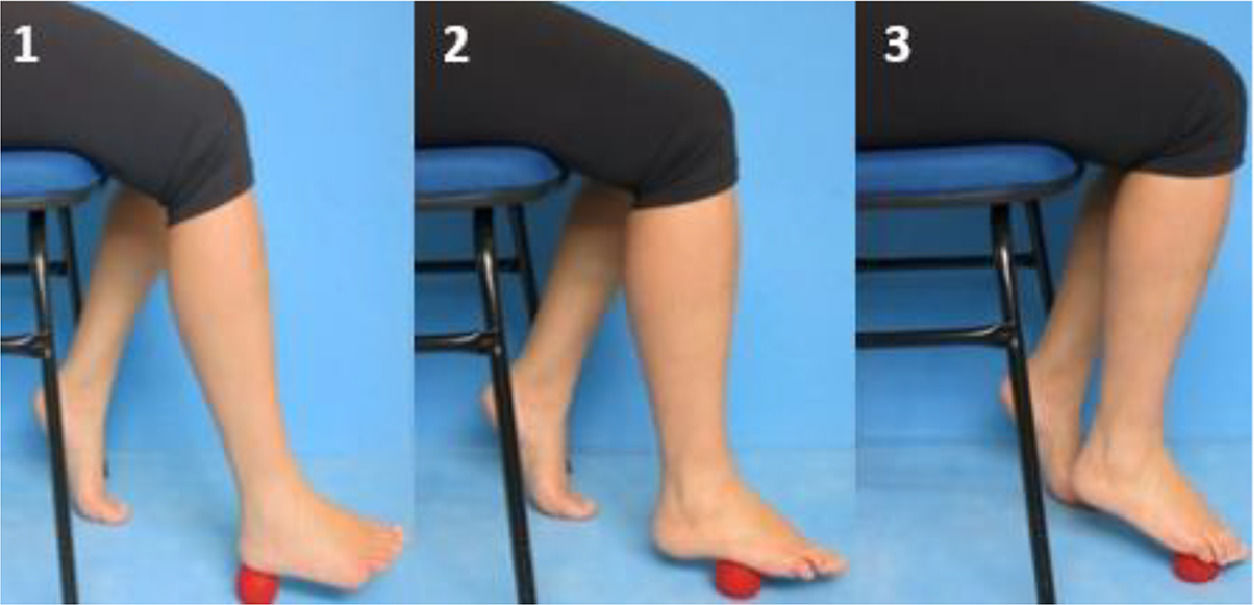
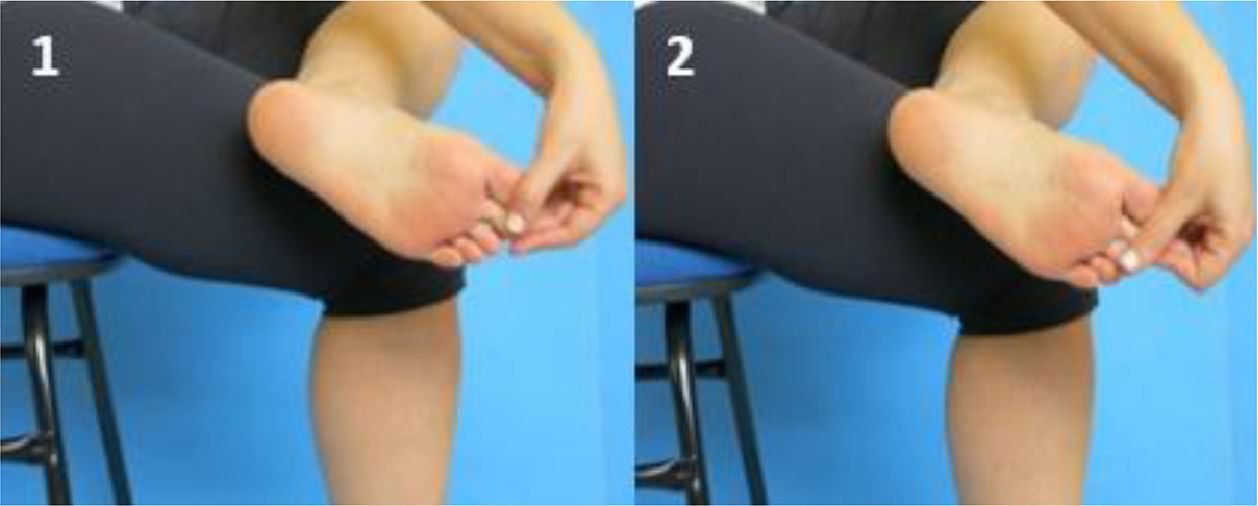
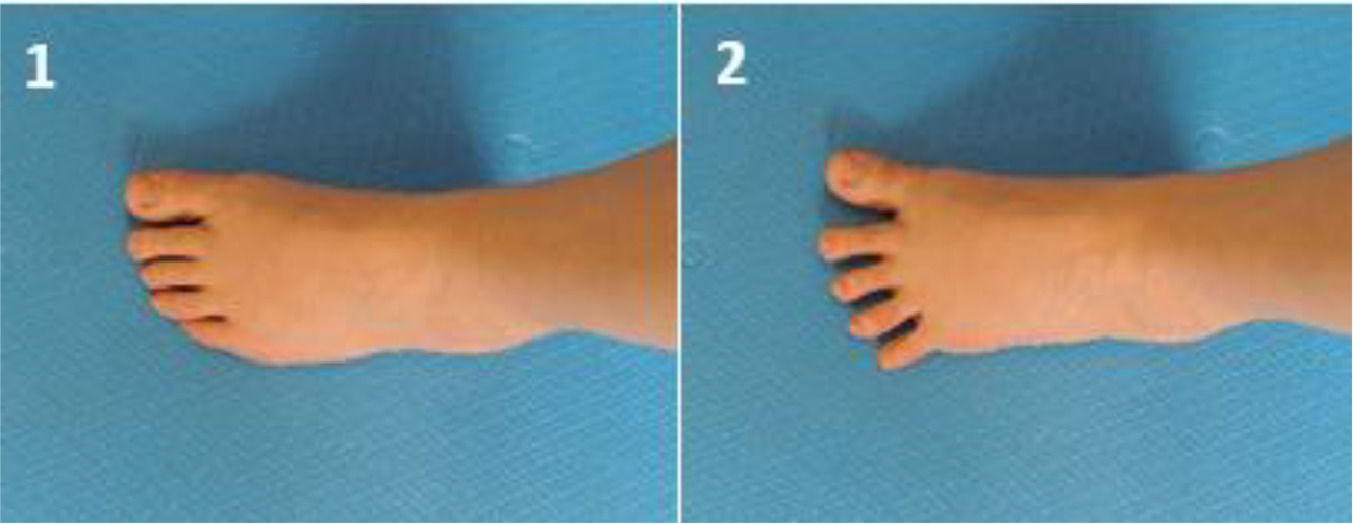
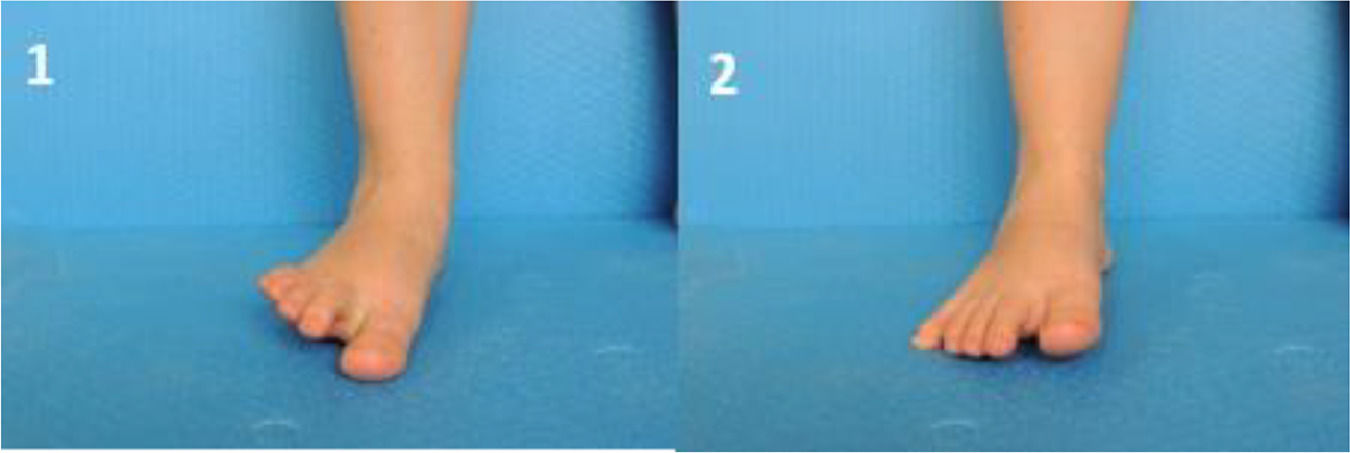
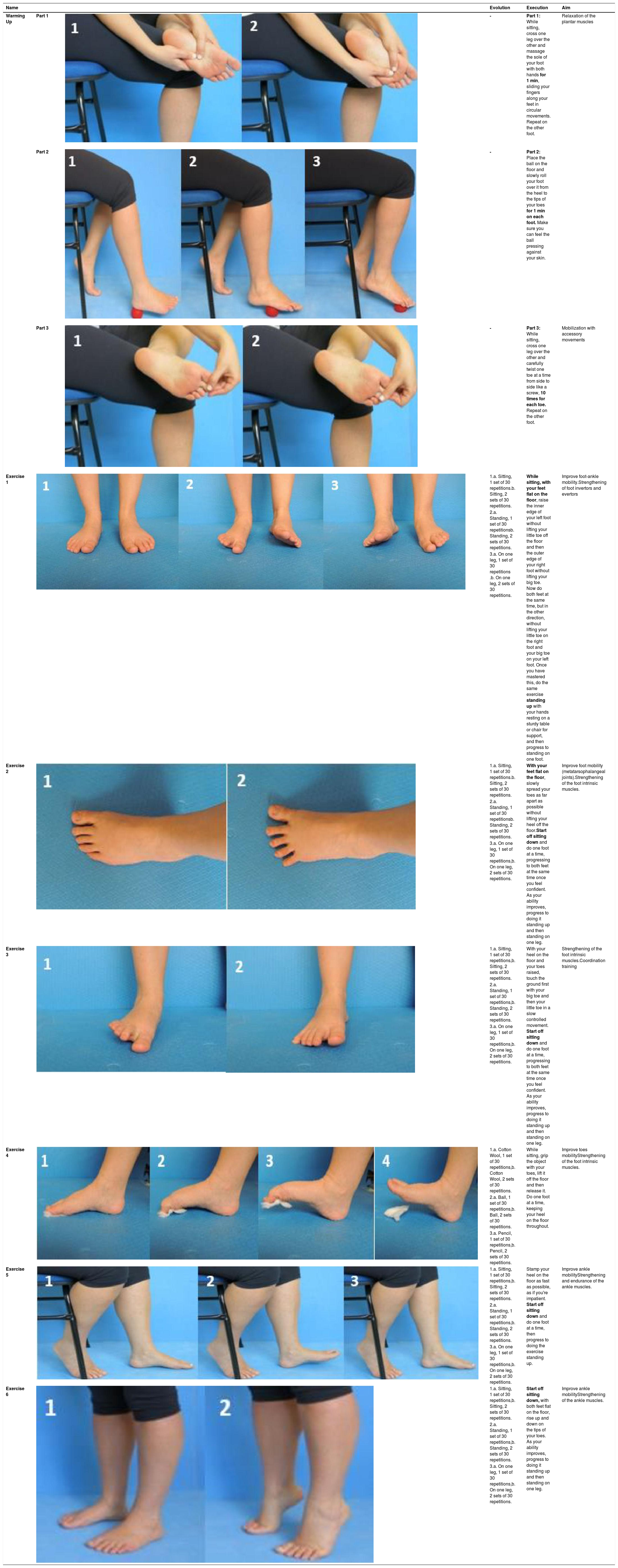
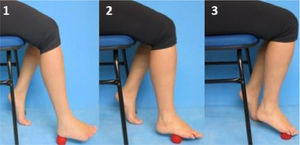
For the booklet layout, texts, photos, and color illustrations were included. Images and illustrations are strategies for representing and complementing textual language and are pedagogical resources that facilitate individuals' understanding.25,26 Each exercise page has a description explaining how the exercise should be performed and contains photos to illustrate the exercise. The selection of the six foot exercises and the included progression parameters were based on a previous successful clinical trial.18 Because the time spent to perform exercises interferes directly with the adherence to daily practice,27 the number of exercises per session was set to be performed within 30 minutes. The exercises were selected to guarantee safety to the user while performing them at home and aimed at improving foot-ankle range of motion and strengthening the intrinsic and extrinsic foot muscles.
The progression of the exercises in the booklet was guided by the overload principle, which assumes the application of a progressive effort in the training sessions that overloads the musculoskeletal system, to cause a stress that exceeds the muscle's metabolic capacity.28 The progression was established by increments in the training volume with increases in the number of repetitions within a set, in the number of sets, and in the load to be sustained during the exercise, i.e., exercises should first be performed sitting, then standing, and, in the last stage, standing on one foot.
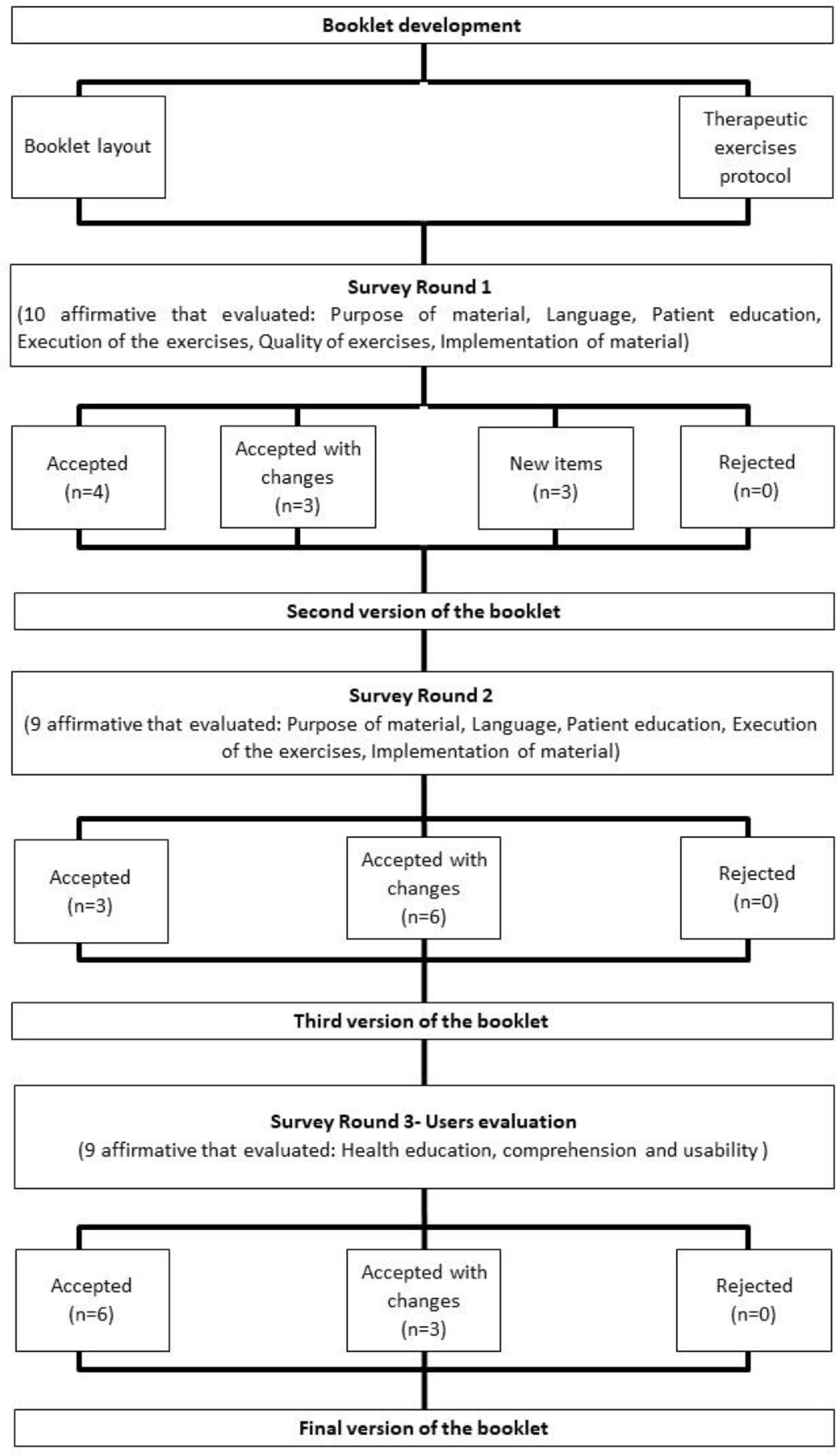
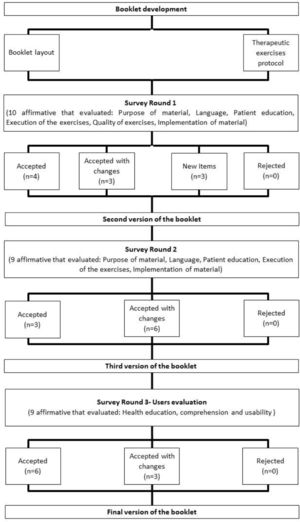
Booklet validation and usability evaluationThe content validation of the Portuguese version of the booklet was performed through the Delphi technique by a jury of experts. The Portuguese validated version of the booklet was then evaluated by users with DPN to gather their opinions on its usability (Fig. 1).
The Delphi technique, with a jury of experts, was used to obtain consensus regarding the booklet. This technique has the advantage of keeping responses anonymous, allowing experts' opinions to be heard and analyzed in several rounds, to improve the refinement process.29 A broad analysis of the material required a multidisciplinary team of experts with clinical experience in the care of individuals with DM and/or practice in health education.
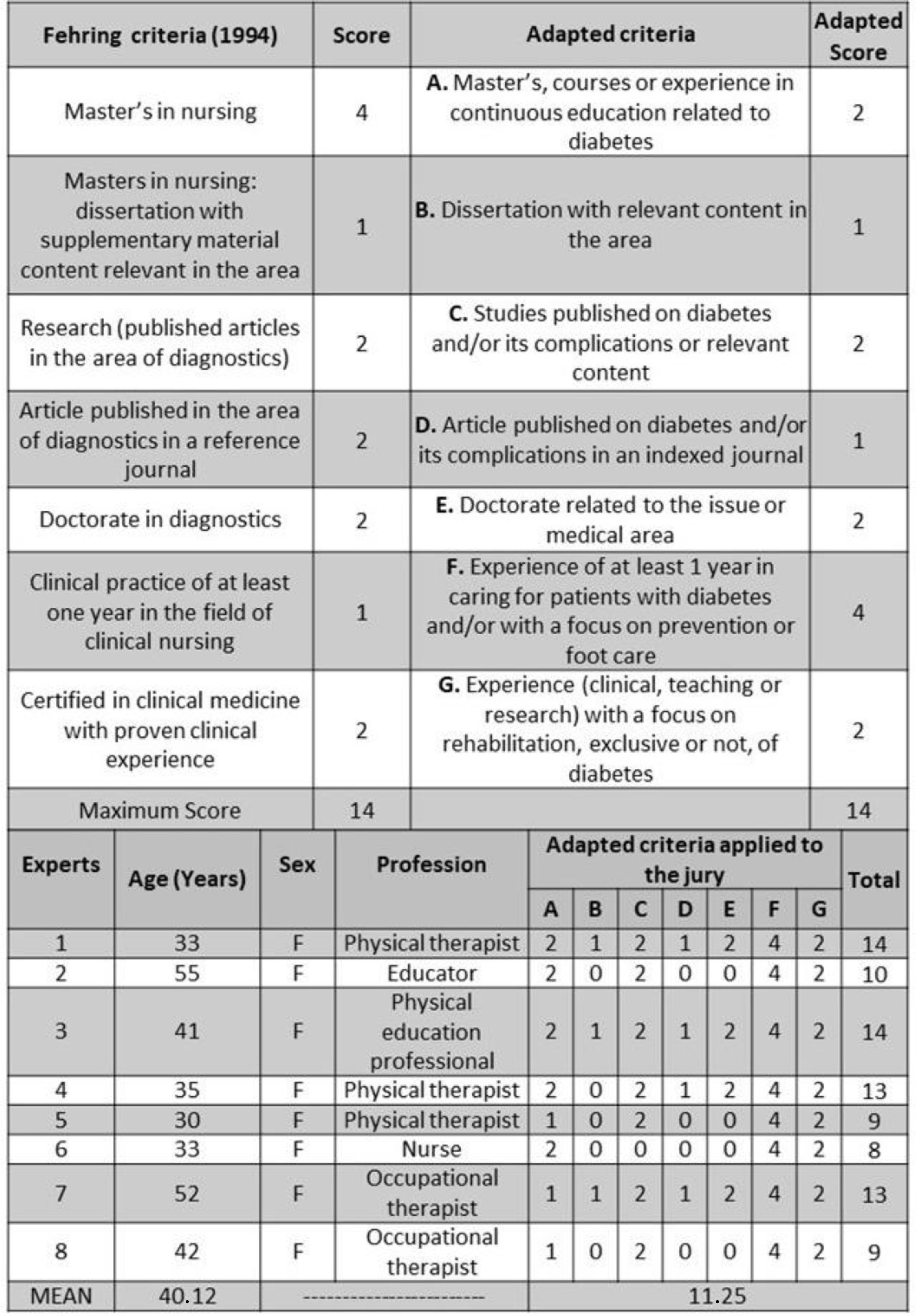
There is no established number of experts on the jury,30 but studies indicate between 15 and 60 experts.31 Fifteen experts, all Brazilian, were invited, but seven were not available to participate in all necessary stages of the study. Thus, eight experts (30–55 years) accepted the invitation and were included: an educator, a nurse, three physical therapists, a physical education professional, and two occupational therapists. For the experts selection, curricula were evaluated using an adaptation of the Fehring criteria (Fig. 2).32,33 The experts were recruited with a minimum score of five out of 14 in the experts adapted scoring system.
The Delphi process was performed in two rounds. In the first round, the jury presented suggestions on the booklet layout and the exercise protocol. The suggestions were then analyzed and incorporated into the second version of the booklet. In the second round, the second version of the booklet was submitted to the same jury, and they were asked to inform if the material was approved or not.
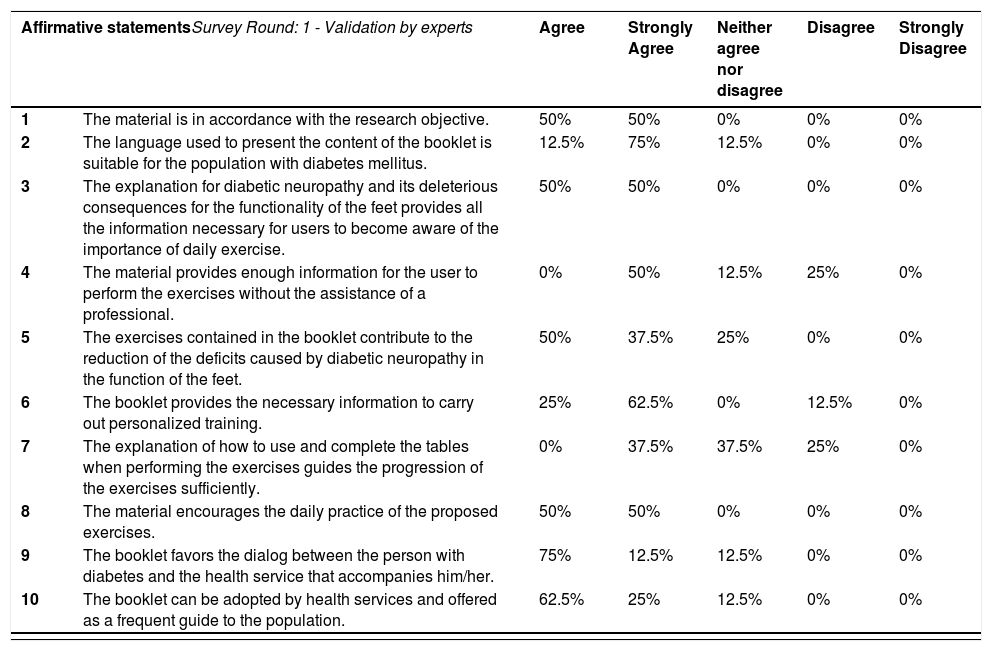
Survey round 1 and 2 - validation by expertsIn the first submission of the booklet, we prepared a structured questionnaire according to the Delphi technique.34–36 The first round was performed between March to May 2015, when the specialists answered individually about statements related to: purpose of the booklet, language suitability to the target population, quantity and quality of the information, contribution of the foot-exercises to improve DM and DPN deficits, and motivation for daily exercise practice (Table 2). The experts gave each statement a score on a five-point Likert scale: strongly agree; agree; neither agree nor disagree; disagree; strongly disagree.
Experts opinions and comments regarding each item were grouped, and the ratings of each item were analyzed. The items were classified as accepted, accepted with changes, or rejected, using the consensus criteria based on previous studies.37 Items that at least 70% of experts indicated "strongly agree" and "agree" were accepted; items that this same percentage of experts indicated “neither agree nor disagree” were accepted with changes, and items that at least 70% indicated “disagree” or “strongly disagree" were rejected.32,36,38 We also strongly recommended the experts to give suggestions and/or justifications for their answers. In this exploratory stage, all suggestions that were considered pertinent to the purposes of the booklet were incorporated, generating a second version of the booklet.
In the second round, performed between May to July 2015, we submitted a new structured questionnaire to the same experts explaining all changes and inclusions made, and we asked them to reassess the booklet, indicating whether they agreed (YES) or disagreed (NO) with the statement, in addition of asking for more comments and suggestions. For the second round, items that rated at least 70% in the jury's general opinion as “agreed (YES)” were accepted.
Survey round 3 - users’ usability evaluationThe booklet was evaluated by a convenience sample of 10 Brazilian users from a larger randomized controlled trial,39 all diagnosed with DM (average (range) time of diagnosis 17.7 years (2–37 years)) with a mean ± standard deviation DPN degree of 3.9 ± 2.9 (range 2.2–9.3). The DPN degree was determined based on the Decision Support System for the Classification of Diabetic Polyneuropathy (http://www.usp.br/labimph/fuzzy/), a software that uses a fuzzy linguistic model that considers three input domains: symptoms and tactile and vibratory sensitivities.40,41 The software gives a score from zero to 10, with higher scores indicating more severe DPN. All the users presented low risk of ulceration according to IWGDF Guidelines on the prevention and management of diabetic foot disease.42 The participants used the booklet for eight weeks, three times a week, and were interviewed by telephone between February to April 2020. The users scored, using a five-point Likert scale, nine affirmative sentences about: health education, comprehension, and usability (Table 2). Because round 3 is an evaluation step, and not a validation one as the previous rounds, the items that rated less than 70% approval (sum of "agree" and "strongly agree") were revised but not submitted to a new evaluation round.
Data analysisData were analyzed using descriptive statistics and the content validation index (CVI) for the first round.43–45 A criterion of 70% consensus approval was used for all the changes implemented in the booklet.
ResultsFirst version of the bookletIn the first version of the booklet, we included two characters to facilitate the communication with the reader through dialog balloons, to guide them about foot self-care and to clarify how the booklet works. In addition to the selected exercises, we included an introduction of the booklet content, explanations about how to use the booklet, important information about the disease, and recommendations for foot care.
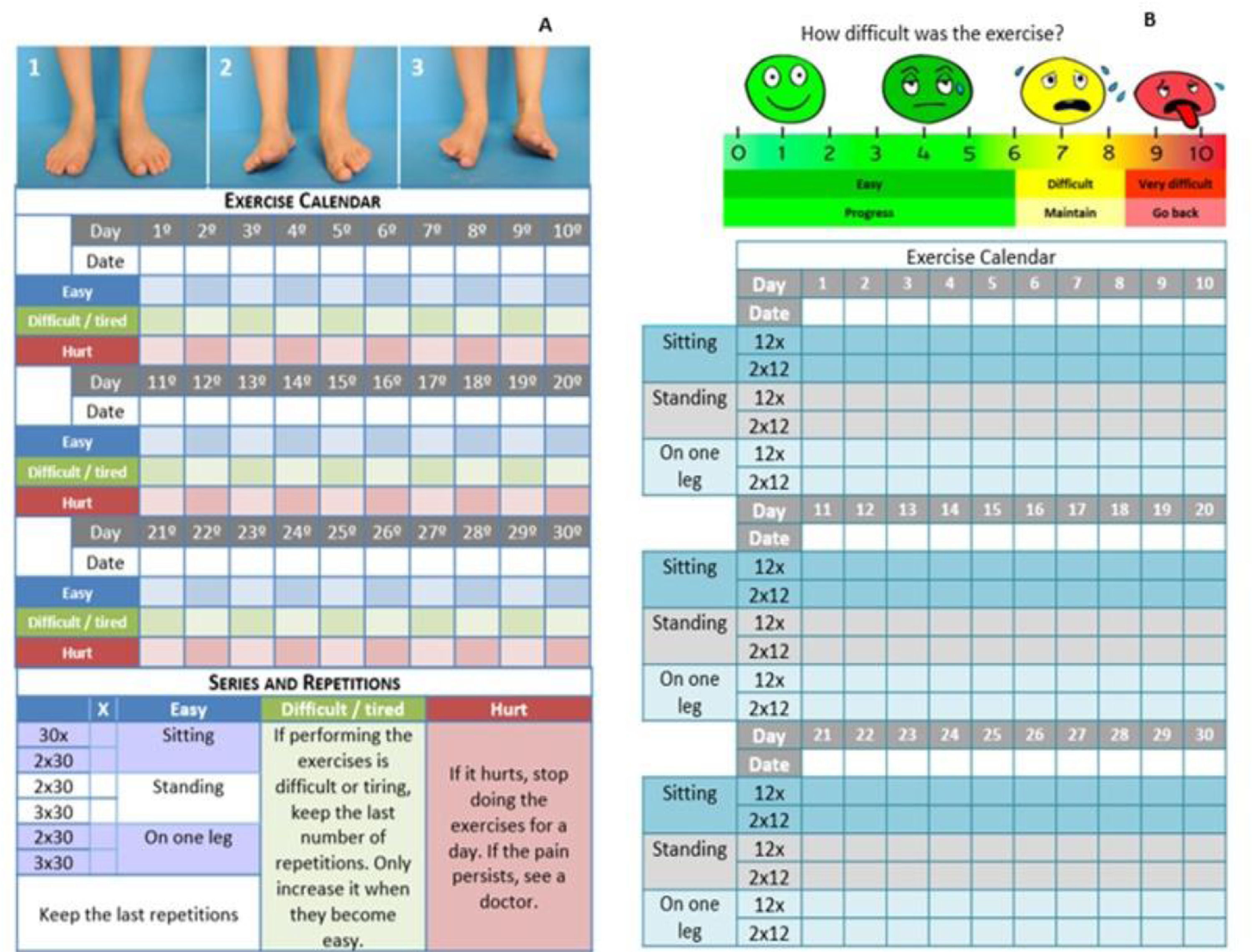
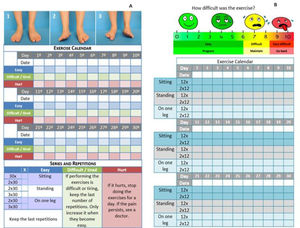
A warm-up exercise through a self-massage was also included to prepare the user to perform the exercises (Table 1). Each exercise had six sublevels of progression (Fig. 3). This progression corresponded to an increase in the difficulty due to a change in the adopted posture (sitting, standing, standing on one foot), and within each posture, the volume of the exercise could be increased (one to two sets of 30 repetitions). The control and progression of the exercises was performed through the completion of a table, where the user, after performing an exercise, would qualify the exercise as “easy”, “difficult / tired”, or “hurt”. Each category had a specific definition to guide the user in their choice and the table used a color feature to facilitate the identification of each criterion (Fig. 2). For each exercise and according to the user's performance, the most appropriate progression was indicated, which includes increasing, maintaining, or decreasing the training volume. For example, if the answer was “easy” to perform a certain exercise, then there was a recommendation to increase the training volume. If the exercise was classified as “difficult”, the last sets of repetitions should be maintained, but if “hurt” was chosen, the advice was to stop doing this exercise for a day, but if pain persists, the user should seek a health service.
Booklet validation - Therapeutic exercise protocol.
The general results for the first round showed that the experts agreed with 82.5% of the statements, they neither agreed nor disagreed with 11.25%, and disagreed with 6.25% (Table 2).
Overall results (in percentage) of the Likert scale applied to the two Survey Round: 1 - Validation by experts and 3 - Users’ usability evaluation.
The average CVI of the first round was 0.82, which indicates that the first version of the booklet achieved satisfactory validation content.46 However, for the 4th affirmative statement (“The material prepares the user with enough information to perform the exercises without the assistance of a professional”) and for the 7th statement (“The explanation of how to use and complete the tables when performing the exercises guides the progression of the exercises sufficiently”) the CVI was 0.50 and 0.37, respectively. The remaining eight statements obtained CVI values above 0.80.
In general, there was a high approval rate for the first round, but as the jury made several suggestions, a second version of the booklet was developed. The exercise illustrations and guidance for recording practice and personalized progression were reviewed.
Experts considered that completing the progression tables was complex, so they suggested to transform the two tables into a single table. Also, the experts considered that the terms suggested for the user to define the feeling of performing the exercises (easy, difficult / tired, or hurt) should be changed because the expression “hurt” refers to a condition that suggests other complications that require medical attention and does not belong to the category of perceived exertion. They also suggested the inclusion of a Visual Analogue Scale (VAS). So, the VAS was included, with the words “easy”, “difficult”, or “very difficult”, the numbers from 0 to 10, and the facial expressions that symbolize the degree of effort felt when performing the exercise (Fig. 3).
For the statements “The language used to present the content that makes up the booklet is appropriate for the diabetes mellitus population” and “The way the exercises are described allows the users to properly understand how it should be performed” the jury pointed out spelling and agreement errors, suggesting corrections and the inversion of the order of some information. The experts considered the language adequate, but because some words or phrases, such as "overload", "glycemia", "injury to the peripheral nerves", could lead to difficulties in the content's understanding by the user, changes were made.
Survey round 2- validation by expertsIn the second round, 100% of the experts agreed with all the statements, meaning that they agreed with all the items and content of the booklet. As some suggestions were again made by the experts, even with a full consensus, these suggestions were incorporated. The jury suggested reversing the order of some information and replacing some words to improve the language and exercises descriptions.
Survey round 3 - users’ usability evaluationTen users evaluated the booklet usability in the third round (90% women, 58.7 ± 3.9 years old), and they had different educational levels: 30% incomplete elementary school, 50% high school, and 20% higher education.
The target population used the booklet for eight weeks and concluded that the material explains in a simple way the complications of DM and DPN and the importance of self-care. However, all of them reported that they already had previous knowledge about the theme and that the booklet reinforced important information received from the health professional. They did not report any complaints of pain and stated that it was easy to understand how the exercises should be performed, and that the illustrations facilitated the adherence to the training. But the users also reported that performing all the exercises was very tiring and took a lot of time from their daily routine.
Among the 9 items evaluated, three had a rating approval below 70%. These were related to performance and exercise progression. Sixty percent of the users reported having difficulty performing 30 repetitions of the six exercises, being unable to finish the repetitions, and feeling very tired during the execution. To solve this issue, either they performed less repetitions, or fractionated the set in different days, and completed the total number in more days. To further improve the material, the number of repetitions was changed from 30 to 12.
The final version of the booklet was entitled “Foot and Ankle Exercises for People with Diabetes Mellitus” and presents 36 pages, including sessions that introduce the characters that present all the content to the users, sessions with information about self-care and about DM and DPN, frequently asked questions, and the exercise session. The validated version of the booklet is available in Portuguese in the online supplementary material A. A translated version in English is also available as online supplementary material B but was not used in this study.
DiscussionThe aim of this study was to develop, validate, and evaluate the usability of an educational booklet containing home-based foot-ankle exercises designed for people with DM and DPN that allows the customization of the training progression according to individual effort perception. To achieve this, the developed booklet had its material content validated with a Delphi technique consensus by experts, and had its usability evaluated by users with DPN.
The booklet was developed and validated with a high degree of agreement between the experts, that also suggested changes that further improved the booklet. Among the main contributions were changes in the vocabulary to make the text simpler and understandable by the target population, and improvements in the table to control the exercise progression. The suggestions resulted in the reduction of the amount of text and in the use of images that made the material more attractive, strategies that have been used with success for people with low health education.25,47 Studies point out that language could be a barrier to self-management of people with DM, because the lack of understanding about the disease and its complications brings adverse results in the control of the disease and its comorbidities.48,49 The jury also suggested incorporating an informative session for health professionals, expanding the use of the booklet, that can be used as a guide for groups of people with diabetes in primary care, home-based treatment, or even individual sessions.
In the evaluation round, users did not complain about the language, however, they suggested changes in the number of repetitions of the exercises. In addition to comments by the users that the exercises were tiring, it was also pointed out that the time to complete all exercises was excessive, which became an obstacle for its inclusion in their daily routine. Because exercise protocols with eight to 12 repetitions are reported as sufficient to produce increases in both muscle strength and endurance,50 the number of repetitions was decreased from 30 to 12.
Considering all the implemented improvements, we can conclude that the booklet is a didactic and intuitive tool that favors the daily practice of foot-ankle exercises. The use of the educational material by health professionals is also a way to remember the verbalized guidelines. It is not intended to replace professional activity, but rather serve as a resource that helps and complements their action.51,52
There is evidence that home exercises are effective.53–55 On the other hand, to maintain the effects of home exercise programs, users must maintain exercise practice for a long time, and the adherence of older adults to home exercise interventions decreases over time.56 Literature shows that patients who used educational materials changed their lifestyle,57 improved their knowledge about DM, improved self-management, and improved their quality of life.58 In addition, receiving written guidance on DM care made people improve their adherence to treatment, even six months after receiving the material.59 Thus, it is possible to affirm that the use of the booklet is a continuous care strategy.
Self-management of diabetes aspects is a complex activity that requires the person with diabetes continuous attention and updates about psychological, social, economic, and behavioral factors interfering in their control of diabetes.60,61 Thus, education for self-management is a key element as it provides guidance for people when making their health care decisions and carrying out their activities.62,63 Contemporary educational resources, such as websites, apps, and digital platforms, have transformed the self-management process by using technology to facilitate care coordination and promote patient health literacy.63,64 However, the use of such technological resources presents some barriers for those who are not comfortable with digital technology65–67 or have social and economic limitations. Internet access also interferes in the technological tools’ consumption, affecting those who are already vulnerable such as older adults, racial/ethnic minorities, and people with low income and education. Therefore, printed materials, such as the developed booklet, can be a safe option for self-management processes and education as they are more accessible to people of all ages and any income level, and do not require additional technological resources.68,69 Health professionals can decide which is the best tool for the patient's treatment based on their level of adherence and preferences for a booklet or a software/app for self-care and personalized foot-ankle exercises.32
The booklet is a tool to complement the care provided by the health team and is not intended to replace the care provided by health professionals. It can be used in clinics, home care, and primary care, acting as a resource to raise awareness of the need for continuous foot-ankle care in people with diabetes. It is recommended that at the distribution sites the user should be trained and guided by a health care provider to fully understand the content of the booklet and perform the exercises properly.
Limitations of the studyThe inclusion of the visual analogue scale, the language adaptation, and the inclusion of the session with foot care recommendations increased the number of pages of the booklet (18 front and back pages), making it an extensive material. It should be printed in colors, but color printing further increases the costs, which can make it more difficult to be distributed. Furthermore, new studies could expand the consultation to a greater number of users. The booklet was produced, validated, and evaluated in Portuguese only by Brazilians, so while an English version is provided, it was not assessed by the experts and users for the features related to language. Therefore, future studies are necessary for validation of the booklet for other countries and languages, including English.
ConclusionThe booklet was validated with a high rate of agreement among experts, and the usability assessment step performed by the users was essential for the improvement of the material. The developed booklet is an educational material for continuous health care, for improving foot-ankle musculoskeletal function, and intends to be a useful tool to prevent and manage the impacts of DM progression. The unique contribution of this material comparing to others available for this population is a regime of exercises with a customized progression based on the users’ effort targeting the reduction of the primary musculoskeletal deficits in the foot-ankle region.
We thank health professionals and people with DM for their contribution and suggestions for improving the booklet and Dr. Ricky Watari for providing language assistance for the manuscript.
JL Veríssimo is received grant funding from the Coordination Agency for the Improvement of Higher Education Personnel (CAPES) [financial code 001]. EY Suda received grant funding from the São Paulo Research Agency (FAPESP) [2017 / 15449-4]. Isabel C.N. Sacco is a fellow of the National Council for Scientific and Technological Development (CNPq) (Process: 304124/2018-4). Funders have no role in the study and have no authority over any study activity or the decision to send the report for publication.