Understanding patients’ perceptions about rehabilitation can guide healthcare administrators on modifications of program elements, which can ultimately improve cardiac rehabilitation (CR) use, adherence of heart-health behaviors, and improvements in clinical outcomes.
ObjectiveTo examine the perception of patients about their participation in CR.
MethodsQualitative study using semi-structured interviews, performed in a public CR center in Brazil. Twenty-eight patients were interviewed 2-years following participation in two CR models: exercise-based and comprehensive CR.
ResultsThemes identified included: knowledge acquisition, improvement in functionality, and psychosocial well-being. It appeared that the perceived benefits of CR participation were overall positive and similar between the two models; however, those in the comprehensive CR identified additional subthemes: self-care need and knowledge transfer.
ConclusionsThis study suggested that patients from two different CR models perceived in the long term that the CR participation positively impacted their disease-related knowledge, promoted functional gains, and improved psychosocial well-being. Structured educational interventions seemed to be associated with improved participants’ perception about CR, which could contribute to long-term maintenance of heart-health behavior and better outcomes.
Cardiac rehabilitation (CR) is an evidence-based, standard of care for those with coronary artery disease (CAD).1,2 Exercise, risk factor management, patient education, and psychosocial management are internationally-agreed core components of CR.3,4 Current guidelines – including from South America5 – promote this comprehensive structure to achieve cardiovascular risk reduction,6 foster health behaviors,7 reduce disability8 and health-related costs,1 and improve physical activity levels.8 Therefore, CR is a well-established model of secondary prevention care that can mitigate the burden of cardiovascular disease (CVD).1,6
Despite these benefits, CR is only available in 40% of low- and middle-income countries (LMICs),9 which is a group of countries that face a disproportionately heavy burden of CVD with scarce resources and lack of pragmatic guidelines.10 These countries, including Brazil, also report low density and capacity of CR programs to address the high need from this population.11,12,13 Other challenges to achieve CR goals and control cardiac diseases in LMICs include high CR dropout rates (when programs are available),13,14 unavailability of interventions to improve long-term maintenance of heart-health behaviors,14 and no standardization of core components and services,11,12 including the lack of patient education interventions.13
Findings from systematic reviews15,16 and meta-analysis17 have demonstrated the effectiveness of patient education for individuals with CAD in improving disease-related knowledge, self-management behaviors, and health-related quality of life, with potential impact on healthcare costs and recurrence of acute events. A randomized controlled trial (RCT) in Brazil18,19 also showed that comprehensive CR (i.e. exercise plus education) can be delivered in a low- and middle-income setting and is effective. Results of this study could be seen as the first step to establish the standardization of comprehensive CR programs in Brazil. However, other important aspects to improve CR use have yet to be assessed, including the understanding of patients’ perception of CR participation.20
Studies have shown that the knowledge of patients’ perceptions about CR participation can contribute to the understanding of their needs and expectations, which can ultimately refine care, optimize service utilization, and increase short- and long-term treatment adherence.20,21 Moreover, patients’ perception does not often correspond to objective reality or to the perceptions held by providers or administrators regarding care,22,23 which can negatively impact efforts to promote adherence to CR and achieve its goals.
Understanding patients’ perceptions about CR can guide healthcare professionals and administrators on modifications of program elements, which can ultimately improve CR use, adherence of good heart-health behaviors, and promote improvements in clinical outcomes. Thus, the objective of this study was to examine the perception of patients with CAD about their participation in two CR models offered by a public CR service in Brazil.
MethodsDesignThis was a qualitative study. Research protocol approval was received from the Research Ethics Committee of the Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil (CAAE 95424518.3.0000.5149). Participants were approached to participate in this study between September 2018 and January 2019 and were asked to attend one scheduled face-to-face interview designed to gather patients’ perceptions on their CR participation. Clinical data were extracted from medical charts (when available).
SettingThe two CR models were offered by a public CR service in the city of Belo Horizonte in Brazil: an exercise-based CR and a comprehensive CR (exercise and education). The program provides a continuum of care for patients with CAD from emergency care to secondary prevention six months after the event. The attributes of the site and the programs are described elsewhere.24 In brief, both models offered 36 exercise sessions for 6 months, each 60 min in duration. The frequency of intervention was as follows: 3 times a week in the first 4 weeks, twice a week for the following 4 weeks, and once a week for the remaining 16 weeks of the program. Additionally, in the comprehensive CR program, 24 weekly education sessions were offered, each 30 min in duration, along with an education workbook. These sessions were delivered by a group of healthcare educators in a group setting.
ParticipantsThis convenience sample consisted of all consenting participants that completed one of the two CR protocols offered by a public CR service as part of a RCT.24 Participants were referred to the CR programs with the following cardiac diagnoses or procedures: CAD, post-myocardial infarction (MI), percutaneous coronary intervention, or coronary artery bypass grafting. The inclusion criteria consisted of having completed the CR program more than two years ago and not having a cognitive impairment (i.e. a score of less than three25 on the Six-Item Screener (SIS)26).
Sample size was based on the principle of theoretical saturation, a process by which data are collected and analyzed until data saturation is reached. This is defined as the point at which no new themes emerge.27
ProceduresEligible individuals were contacted by telephone, informed about the study objectives, and assured of their confidentiality regarding the provided information. Informed consent was obtained from all participants. The SIS26 was applied by telephone and participants without identifiable cognitive impairment were scheduled for a face-to-face interview.
A single researcher performed data collection through an individual face-to-face in-depth semi-structured interview at the hospital site. A pilot study with 2 individuals was conducted to assess whether the questions were understandable and/or adjustments were needed. The interviews were recorded using a digital device, and later transcribed in full. Interviews lasted on average 20 min. Transcripts were sent to the participants to ensure validity and to avoid significant errors that may impact the research quality.27,28 Transcripts did not include participants’ names, whose identification was done according to sex, age, and CR protocol.
Interview guideA semi-structured interview guide (Table 1) was developed, consisting of questions about patients’ experience of CR participation. The interview guide had 5 questions divided into two parts: (1) questions related to the overall CR experience; and, (2) questions related to heart-health behaviors: physical exercise, diet, smoking cessation, alcohol consumption, and medication use, which are usual goals of CR programs. Suggestions for the improvement of the program were also requested. Patients’ sociodemographic characteristics (educational level, family income, and occupation) were also collected during these interviews.
Semi-structured interview guide.
| Research topics | QuestionsProbes |
|---|---|
| Overall Cardiac Rehabilitation Program experience | 1. How was your experience participating in the Cardiac Rehabilitation Program? |
| ● What are the positive aspects of the Cardiac Rehabilitation Program? | |
| ● What are the negative aspects of the Cardiac Rehabilitation Program? | |
| 2. What is your opinion about the education classes? (for the group that participated) | |
| ● Do you have any suggestions for the structure of the program? (exercise or education components) | |
| ● Any questions or other comments related to your experience | |
| Heart-health behaviours | 3. Was there any day-to-day activity that you were not able to do before the Cardiac Rehabilitation Program? |
| ● At the end of the Cardiac Rehabilitation Program, were you able to do the activities you need in your day-to-day? (give examples) | |
| 4. Do you currently follow the guidelines provided during the Cardiac Rehabilitation Program? (Physical exercise, food, smoking, alcohol consumption, medication adherence)? Report how. | |
| ● Describe details about physical exercise: if the participant is currently exercising, type of exercise, how many times per week, how many minutes per day, how he/she fells (tired?), reasons to exercise | |
| ● Describe details about dietary habits: describe their food habits and salt consumption. | |
| ● Describe details about smoking habits: smoking status, how many cigarettes per day, if former smoker, how long did stop smoking. | |
| ● Describe details about alcohol consumption: drinking habits and quantities. | |
| ● Describe details about medication adherence: if participant follows medication prescription, if there are any strategies to take her/his medication at the right time, reasons for not following prescription | |
| 5. What are the facilitators identified to follow the behavior guidelines provided during the Cardiac Rehabilitation Program? | |
| ● Do you use any strategy to follow the guidelines provided? Please detail if any. | |
| ● What are the difficulties/barriers encountered in following the guidelines provided during the Cardiac Rehabilitation Program? |
Data were analyzed using principles of Grounded Theory29 to identify key factors related to CR participation and patients’ experience with this intervention. Analyses were then performed through thematic content analysis.30 This technique consists of three phases as follows: (1) collected data were initially organized for pre-analysis with a cursory reading of the transcribed materials; (2) an exploratory analysis was performed, which consisted of a careful reading of each transcript to identify and establish codifications to build the meaning cores, which construct the communication; and, (3) the data analysis was performed, with categorization of the emerged themes and interpretation of the materials that were related to the theoretical foundation.30 At least two members of the research team coded each transcript. Additional codes were added iteratively to capture new information until saturation was reached. The research team discussed differences in coding until consensus was reached. Coders also captured quotes supporting each factor. Findings were organized using Microsoft Excel.
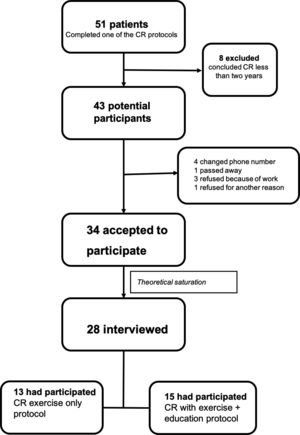
ResultsParticipants’ characteristicsFig. 1 displays the flow of participants through the study. In total, 43 patients were eligible, of which 34 (79%) signed the consent form and 28 (82%) were interviewed.
Sociodemographic and clinical characteristics of participants are reported in Table 2. No significant differences were found between participants who completed the two CR models. Participants were significantly more likely to be male, married, retired, with incomplete elementary education level, and monthly family income of less than 560.79 USD.
Participants’ characteristics.
| Total (n = 28) | Exercise-based CR (n = 13) | Comprehensive CR (n = 15) | ||
|---|---|---|---|---|
| Sociodemographic | ||||
| Age (years) | 65.7 (63.0, 68.5) | 66.0 (61.7, 70.3) | 65.5 (61.4, 69.5) | |
| Sex | Men | 20 (71.4) | 10 (76.9) | 10 (66.7) |
| Women | 8 (28.6) | 3 (23.1) | 5 (33.3) | |
| Civil status | Single | 4 (14.3) | 2 (15.4) | 2 (13.3) |
| Married | 19 (67.9) | 9 (69.2) | 10 (66.7) | |
| Widow | 2 (7.1) | 1 (7.7) | 1 (6.7) | |
| Divorced | 3 (10.7) | 1 (7.7) | 2 (13.3) | |
| Occupation | Domestic homemaker | 1 (3.6) | 1 (7.7) | – |
| Employed | 9 (32.1) | 4 (30.8) | 5 (33.3) | |
| Retired | 18 (64.3) | 8 (61.5) | 10 (66.7) | |
| Unemployed | – | – | – | |
| Education levela | Illiterate | 2 (7.1) | 1 (7.7) | 1 (6.7) |
| Incomplete elementary | 18 (64.3) | 9 (69.2) | 9 (60.0) | |
| Complete elementary | 1 (3.6) | 1 (7.7) | – | |
| Complete high school | 5 (17.9) | 1 (7.7) | 4 (26.7) | |
| Complete post-secondary | 2 (7.1) | 1 (7.7) | 1 (6.7) | |
| Post-graduate | – | – | – | |
| Monthly family incomeb | Up to 1 minimum salary | 4 (14.3) | 1 (7.7) | 3 (20.0) |
| 1 to 2 minimum salaries | 6 (21.4) | 4 (30.8) | 2 (13.3) | |
| 2 to 3 minimum salaries | 10 (35.7) | 4 (30.8) | 6 (40.0) | |
| 3 to 4 minimum salaries | 4 (14.3) | 2 (15.4) | 2 (13.3) | |
| 4 to 5 minimum salaries | 2 (7.1) | 1 (7.7) | 1 (6.7) | |
| 5 to 6 minimum salaries | 1 (3.6) | – | 1 (6.7) | |
| Did not want to reveal | 1 (3.6) | 1 (7.7) | – | |
| Clinic | ||||
| Diagnostic | Myocardial Infarction | 24 (85.7) | 11 (84.6) | 13 (86.7) |
| Angioplasty | 2 (7.1) | 2 (15.4) | – | |
| CRVM | 2 (7.1) | – | 2 (13.3) | |
| Comorbid | Hypertension | 28 (100) | 13 (100) | 15 (100) |
| Diabetes | 24 (85.7) | 12 (92.3) | 11 (73.3) | |
| Obesity | 6 (21.4) | 2 (15.4) | 4 (26.7) | |
| Dyslipidemia | 28 (100) | 13 (100) | 15 (100) |
Data are frequency and percentage: n (%) except age, which is mean and 95% confidence interval. No difference between the exercise-based and the comprehensive program groups for any of the variable P>.05.
Illiterate = less than 1 year of study; Incomplete elementary = between 1 and 7 years; Complete elementary = 8 years; Incomplete high school = between 9 and 10 years; Complete high school = 12 years; Incomplete post-secondary = between 13 and 15; Complete post-secondary = 16 years; Post-graduate > 16 years.
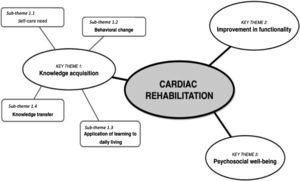
Three thematic categories emerged after careful analysis of the data. These key themes fall under the categories of knowledge acquisition, improvement in functionality, and psychosocial well-being. These categories are shown in Fig. 2 with associated sub-themes.
Examples of patient’s perceptions for each theme are presented in Table 3.
Selected patient’s expressions in each key theme.
| Key theme | Sub-themes | Patient’s perception |
|---|---|---|
| Key theme 1: Knowledge acquisition | Self-care need | “I learned a lot in the rehabilitation. I learned the effect of medication, how to take care of myself, know my limitations, and how to eat better” (I24, male, 66 years old, comprehensive protocol).“[… ]I learned that walking itself lowers pressure, you feel better after walking, your body feels great. […] the teachings which keep me alive because […] if it wasn’t for this diet that I have, I might be dead (I03, male, 49 years, comprehensive protocol). |
| Behavioral changes | “[…] I learned a lot of good things for me, to always do gymnastics, […] the priority is diet and gymnastics, […] I started doing gymnastics while in the CR program and continued there (health clinic), I went back to cycling and […] I’m making brown rice, I only steam my food […]” (I17, female, 61 years old, comprehensive protocol). | |
| Application of learning to daily living | “[…] Today I don’t do my walking without first warming up, and when I finish, I do the cool-down. And I try to do everything that is shown in the book too, I try to do every type of exercise” (I21, male, 71 years old, comprehensive protocol).“It was excellent to me that I learned a lot that I didn’t know, for example, I didn’t imagine that I would have to have control of my heartbeat during my walk” (I22, male, 71 years old, comprehensive protocol).“I have that little watch, I bought it […] I keep looking at the frequency, and when I see that I’m in that exhausted phase, I slow down, then when I see that it gets better, I start to accelerate again” (I11, woman, 66 years old, exercise protocol). | |
| Knowledge transfer | “[… ]and it works to pass it on to other people, to your family, just as I passed the info there to the group (primary care group)” (I17, female, 61 years old, comprehensive protocol). “And that book helped me so much, a lot. I already lent that book to about 10 people or more. There were people who copied it” (I21, male, 71 years old, comprehensive protocol) | |
| Key theme 2: Improvement in functionality | “I was starting to mop the floor and I was tired, my chest was starting to hurt, I couldn’t wring the floor cloth […] After the rehab I can do it, I cook, I wash my clothes all by hand, I can rub it. Now I am excited to do these activities” (I23, woman, 68 years old, exercise protocol).“[…] I couldn’t swim, today I swim. I couldn’t walk straight for some time, now I walk an hour and a half easily” (I21, male, 71 years old, comprehensive protocol).“I couldn’t do work that was hard. It felt bad, then it got better […] I got tired of climbing the stairs. I’m not tired anymore, now I feel great. I've been working out, climbing the stairs. I don’t get tired, my heart is good” (I18, male, 69 years, exercise protocol). | |
| Key theme 3: Psychosocial well-being | “[…] In terms of health, the time that I felt the best was exactly during the rehab program […] you end up doing an exercise that is vital for yourself, you can see that these exercises give good performance to our health […] a tiredness which is compensated by the time it ends, you leave looking like you are floating, it is like you are someone else” (I01, male, 66 years old, comprehensive protocol).“[… ]In the emotional sense, it was also very good. Wow! My self-esteem … went up, up a lot, it was very good” (I04, female, 71 years old, exercise protocol).“[…] Even when I was living with people, I didn’t have much tolerance. Sometimes I got nervous, then it got better and my boys felt it, so I changed my way […]” (I17, female, 61 years old, comprehensive protocol).“[…] one of the first things I felt was that I lost some of the fear. After the angioplasty, you get scared of doing things! As the girls put me up to running, so I realized that I can do a lighter workout in the gym, I can continue my brisk walks like I used to do, do a few jogs. […] That was good for me, it gave me more confidence” (I15, male, 63 years old, exercise protocol). |
Note: in parentheses (patient research number, sex, age, and study group).
The respondents of both the exercise and comprehensive protocols perceived CR as an opportunity to learn about the need to take care of themselves after the cardiac event and the relevance of behavioral change in secondary prevention, and to guide their daily lives after a cardiac event. Knowledge acquisition was also seen as an enabler on information sharing about their health condition to people they are related to. This first theme had four associated sub-themes as follows: self-care need, behavioral changes, application of learning to daily living, and knowledge transfer.
Self-care need: Participants of the comprehensive protocol revealed that they became aware of the need to take care of their current health condition due to the systematic information provided during CR, which included taking their medications correctly, respecting their physical and mental limitations, and having an adequate diet. They emphasized the benefits of physical exercise achieved during the CR program. They also defined self-care as an essential task to stay alive. This perception was not identified in participants from the exercise protocol.
Behavioral changes: Participants perceived that behavioral changes acquired during CR participation were made possible by the knowledge gained during the program. These behaviors included the regular practice of physical activity (reported by participants in both protocols) and healthy eating habits (reported only by participants of the comprehensive protocol). Additionally, participants associated body weight reduction and blood pressure control with these new behaviors.
Application of learning to daily living: Participants from both CR programs mentioned that the knowledge acquired was applied to their daily activities, including the practice of physical exercises. This perception was related to properly performing physical exercises, to include warm-up/cool-down components in their activity practices, and to identify the ideal intensity for training. In addition, participants identified the need for a heart rate monitor and support materials to continue the practice of physical activity – and include this in their new daily routine - after CR.
Knowledge transfer: Participants of the comprehensive protocol perceived the need to share the knowledge gained and the materials received in CR with family, friends, and primary care physical activity groups.
Key theme 2: Improvement in functionalityParticipants of both CR protocols perceived improvements in functionality such as better performance of their daily, leisure, and professional activities and increased physical-related mobility, such as the ability to walk longer distances and/or at higher speeds and climb stairs.
Key theme 3: Psychosocial well-beingPatients perceived CR benefits related to emotional health, including recovery of self-esteem, improvement in social relations, and regaining confidence to resume daily activities.
DiscussionEarly reports indicated that an understanding of the patients’ perceptions of CR is associated with CR use, adherence of recommended heart-health behaviors, and improvements in patients’ clinical outcomes. Cardiac rehabilitation programs are underutilized worldwide11 and, to our knowledge, there are no standardization of comprehensive CR programs in Brazil. The qualitative analysis showed how patients with CAD, who had attended CR, had positive perceptions about this participation two years after discharge from these structured programs. Perceptions were related to the categories of knowledge acquisition, improvement in functionality, and psychosocial well-being. It appeared that the perceived benefits of CR participation were similar between CR models; however, participants in the comprehensive CR program identified extra sub-themes: self-care need and knowledge transfer.
Knowledge acquisition was perceived by participants from both CR models. However, our results suggest that the structured education from the comprehensive CR model made it possible for patients with CAD to reflect on the importance of broader lifestyle goals, including dietary control and appropriate medication use, as these perceptions were only mentioned by participants of the comprehensive protocol. Recent studies have shown that educational interventions designed for patients in CR are associated with adherence to lifestyle recommendations, including a heart-health diet,18,31,32 and medication use.31,33 The identification of these components two years after CR completion suggests that comprehensive CR would have more sustained effects on behavior change post-CR and may be associated with maintenance of long-term health habits, which is a major challenge for CR.34
Another important finding related to the participation in a comprehensive CR program was patients’ ability to recognize their physical, behavioral, and emotional limitations and the importance of behavioral change in secondary prevention, which is essential for self-management. When patients acknowledge the role that lifestyle behaviors play in the course of their disease, it is feasible to say that they can understand their personal control over these behaviors and their active and responsible role in disease control, including drug management, symptom recognition, and risk factor modification.35,36 In this scenario, it is also necessary to highlight the importance of healthcare providers and educators to support and guide patients to translate that knowledge and awareness into action, which was also identified by a previous study.37 Therefore, providing sufficient information is one of the steps for autonomy and accountability in adherence to care, with the role of health professionals as facilitators in the process of effective self-care engagement being crucial so that patients feel confident to self-manage their conditions.36–39
Even without participating in the education classes, the individuals in the exercise CR protocol used non-systematic instructions/information received from physical therapists and information exchange between patients during exercise sessions to change behaviors. The participants in the CR programs value the opportunities for socialization with the multidisciplinary team as well as with other participants as a way of understanding their condition and its possible causes, thereby promoting lifestyle changes.
The information received was perceived as beneficial in different ways by patients with CAD, such as a tool for maintenance of physical activity and healthy eating habits, which resulted in perception of weight loss. Exercise is a core component of CR and while exercise adherence rates among CR participants are usually met during the program, studies have shown that exercise after CR completion is not maintained, with only one-third of patients engaging in regular exercise when assessed 6 months following CR completion.40 The constructs related to exercise maintenance after CR perceived by participants in this study included the following: the importance of social support; factors related to self-regulation, i.e. establishing a routine/habit; creating action plans and goals; and self-monitoring, as well as recognizing and associating health benefits. These results are similar to the ones provided by previous studies.41,42
Patient education is a core component of CR programs and refers to activities that raise an individual's awareness, giving the individual the health knowledge required to decide what is best for their health.16 This study provides contemporary data on the education experience of patients with CAD following a comprehensive CR program. This is particularly important given the challenge to include this core component in programs: education interventions require training of healthcare providers to become health educators, resources (for both providers and patients), and perform content and cultural adaptation to individual needs.4 In the present study, participants in the comprehensive CR program recognized the application of learning in their daily routine and the usefulness of the book to reinforce learning. Another study similarly found that educational sessions were informative, empowering, and necessary for women to maintain healthy lifestyle changes, including performing a safe home or community center exercise program.43 The fact that patients remain aware of the need to continue taking care of themselves two years after the end of CR and continuing with the behavioral changes implemented in their daily lives reinforces that the education offered was effective.24
An interesting fact indicated by those in the comprehensive CR program was the knowledge transfer to family and friends. Respondents perceived the need to share resources and knowledge to motivate others to feel better, adopt prevention strategies, and adopt lifestyle changes, thus acting as multiplier agents. This involvement in disease control by patients is essential, especially in LMICs where health resources are scarce.4,44
One of the objectives of CR is the maintenance/recovery of functional capacity45 and reintegration and optimization of participation in society,46 which contributes to return to previous activities.42 A range of personal, environmental, and social factors may limit this ability to perform activities; therefore, one of the goals of CR programs should be to maximize functional capacity and provide ways to facilitate reintegration.46 In this context, respondents from both protocols perceived they made improvements in functionality, which improved social participation, self-esteem, and well-being. These observed factors are consistent with the literature, that identifies CR as a source of empowerment for patients to return to active living.43
Fear, anxiety, and depression are common symptoms among cardiac patients – especially the ones with a recent cardiac event47 and recovering from cardiac surgery.48 Participants in our study perceived a decrease in their fear to return to regular daily activities. This was an important finding because studies have shown that cardiac patients usually experience both fear of having a new event and a desire to perform normal daily activities.49 In this context, CR was perceived as a safe environment in which participants became physically active and encouraged to resume their usual tasks. These results were also identified in previous studies.21,50 In addition, participants perceived the exercise component of their program as the responsible factor for tangible improvements in health and well-being, which was also identified in previous studies and considered as a reassuring factor for practicing more exercise and returning to the previous level of physical activity.44
Participants also perceived CR participation and the continuous practice of physical exercise during and after this intervention as positive factors affecting their psychosocial well-being. Examples of psychological benefits associated with the practice of exercise included the pleasure associated with the CR sessions, the well-being feeling after exercise, and the confidence to resume daily activities. These factors are associated with recovery of patients’ self-esteem and improvements of their social relations, which are also considered facilitators in maintaining active behavior.47,51 As recognized by the patients in the present study, CR decreased negative emotions associated with their cardiac history and increased their sense of control.52
This study has several limitations. Therefore, we recommend caution when interpreting the results. The chief limitation is related to selection bias, because results are from a sample of patients who attended CR programs at one site, which is not the reality of most cardiac patients in LMICs.13,14 Moreover, those who accepted to participate may be those who had a better experience. Thus, these findings may be limited in their generalizability. However, the results appear consistent with those from other studies, supporting the validity of the results. Another limitation is the fact that patients’ perceptions are not necessarily isolated from their beliefs; therefore, it is suggested that future studies also focus on patients’ beliefs about CR and their condition. Finally, although the interpretation and discussion of the themes generated would appear to support long-term perceptions of these patients, these results remain speculative until replication in a larger sample of patients with CAD. New qualitative studies with different groups of patients attending CR programs (e.g. stroke, diabetes, and hypertensive patients) should be conducted, to assess the unique experiences of these participants.
ConclusionThis study suggested that patients from two different CR modes (exercise and comprehensive) perceived in the long term that the CR participation positively impacted their disease-related knowledge, promoted functional gains, and improved psychosocial well-being. Structured educational interventions seemed to be associated with an increase in participants’ perception about CR in addition to an increase in physical exercise performance, which could contribute to long-term maintenance of heart-health behaviour and better outcomes.
Conflict of interestNone to declare
Authors would like to acknowledge Gabriela Suellen Chaves and Thiago Henrique da Silva Martins for organizing the database. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance Code 001; by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq#307301/2018-4) and; by Fundação de Pesquisa do Estado de Minas Gerais (FAPEMIG).