Patients with diabetes mellitus are exposed to important complications. Currently little evidence exist on the guidelines that these patients, at some risk of foot ulceration, should follow for physical exercise.
ObjectivesTo reach a consensus among multidisciplinary and international experts on physical activity/exercise recommendations for patients with diabetes, according to foot ulcer risk.
MethodsUsing a three-round Delphi method, a panel composed of 28 multidisciplinary experts in the management of diabetic foot assessed 109 recommendations on physical activity/exercise for patients with diabetes mellitus, according to their risk of foot ulcer. Consensus was assumed when 80% of responses matched the same category (agreement/disagreement).
ResultsTwenty-nine experts participated in the first and second rounds of consultation, and twenty-eight did so in the third, reaching final agreement on 86 of the 109 recommendations considered (78.9%). The study, thus, generated a consensus set of recommendations concerning different aspects of diabetic footcare before, during, and after exercise (e.g. when to examine the foot, how to assess it, what type of sock and insole to use, what types of exercise to perform, and when it is advisable to return to activity after an ulceration).
ConclusionThis Delphi study generated recommendations based on the consensus of international experts on physical activity and exercise by patient with diabetes at risk of ulceration. Recommendations considered the state of the foot and the patient's history and status before physical activity and included information on intensity, duration, frequency, and progressions of physical activity/exercise, and the use of custom-made plantar orthoses, shoe prescription, and the convenience of returning to physical activity after an ulceration.
According to the International Diabetes Federation (IDF), in 2019, 135.6 million people aged 65 years or more had diabetes, equivalent to 19.3% of the total population with diabetes worldwide. Moreover, if present trends continue, the number of people aged 65 years or over with diabetes will rise to 195.2 million by 2030 and 276.2 million by 2045.1
People with diabetes mellitus (DM) are at increased risk of developing serious health problems that could lead to a poorer quality of life and increase healthcare costs.2 One such problem is foot ulcers, which are associated with increased morbidity, mortality, and healthcare costs.3,4 It has been estimated that 15–25% of people with diabetes will be affected by a foot ulcer at some point in their lives.5,6
Diabetes induces characteristic pathological changes in the feet, such as infection, diabetic foot ulcer, and neuroarthropathy, broadly termed diabetic foot syndrome.7 This condition is normally addressed by preventive strategies including patient education, risk stratification, and regular foot evaluations for peripheral vascular disease and neuropathy.8 In addition, physical activity and exercise enhance glycemic control and nerve function for people with DM, hence reducing the risk of diabetic neuropathy, a major risk factor for foot ulcers.
Physical activity is defined as any movement that increases energy use, as distinct from exercise, which is a planned and structured physical activity. Physical activity improves blood glucose control in type 2 DM, reduces cardiovascular risk, contributes to weight loss, and enhances well-being.9,10 If performed regularly, it can prevent or delay the development of type 2 DM.11
Although physical activity and exercise are recommended for people with DM,12–14 information is scarce on the type of activity most suitable for people at risk of developing foot ulcers (e.g., those with neuropathy, peripheral arterial disease [PAD], or foot deformities) and on the specific impact made by physical activity on the foot and on the risk of ulceration.
Patients with diabetes with impaired protective sensitivity and restricted pain response are vulnerable to trauma and extrinsic forces from ill-fitting footwear. Motor neuropathy causes muscle weakness and an intrinsic muscle imbalance that can lead to deformities such as hammer or claw toes, which in turn create elevated plantar pressure due to instability of the metatarsophalangeal joint. For this reason, performing physical activity or exercise without medical supervision can create a risk for persons with DM.15
In clinical practice, uncertainty remains about the best type and intensity of exercise for these patients, especially those at high risk of developing a foot ulceration or re-ulceration. Accordingly, the aim of this study was to reach a consensus among multidisciplinary and international experts on recommendations for physical activity/exercise by people with DM, according to their risk of foot ulcers.
MethodsStudy designThis observational, cross-sectional, descriptive study was conducted using a three-round Delphi technique,16 that is commonly used to identify areas of agreement among experts in diverse areas of knowledge17–19 in the absence of full agreement or when knowledge is incomplete, uncertain or unproven.20 The Delphi method offers several advantages over other consensus techniques such as focus groups or nominal groups. First, it does not require the physical presence of the experts, enabling them to participate at a distance in space and time. In addition, the anonymity provided fosters free expression and minimizes the influence of opinion leaders. Specifically, the present study was conducted following the CREDES guide (Conducting and REporting of DElphi Studies),21 details of which have been published previously.22 This study was approved by the Office for Responsible Research at our institution. No authorization from the ethics committee was required, as no personal patient data were used.
ParticipantsFour experts working in Spain in the field of diabetic foot (two endocrinologists, a podiatrist, and a physical therapist) were recruited to the scientific committee. These experts, selected out of convenience from the research group's professional network, conducted the critical review of the first version of the Delphi survey created by the research team, reviewed the selection criteria for the expert panel, and identified other experts to participate in the study.
An expert panel was formed to elicit the opinions of international, multidisciplinary experts working in various fields related to the management of diabetic foot (endocrinology, family medicine, vascular surgery, podiatry, physical therapy, and physical activity and sports), through an online Delphi survey to be completed individually and anonymously.
There are no firm recommendations regarding the optimal size of a Delphi panel in heterogeneous samples. In recent Delphi studies, some panels have included as many as 60 members,17,23 while others have had 40,24 or as few as 19.18 In our study, invitations were emailed to 60 professionals with clinical and scientific experience in diabetes and who met the study selection criteria (these are specified in detail in the study protocol). Twenty experts were initially selected from each group.22 The panelists were not required to be physically present, but only to respond online to the Delphi survey questions, within the stipulated period.
Delphi methodThe research group developed an adapted version of the Delphi survey based on a literature review of guidelines related to physical activity and diabetes14,25–39 The scientific committee then reviewed and modified this draft survey to create a final version. Foot risk was stratified in accordance with the guidelines published by the International Working Group on the Diabetic Foot (IWGD), as follows: risk 0 (very low risk): no loss of protective sensation (LOPS) and no PAD; IWGDF risk 1 (low risk): LOPS or PAD; IWGDF risk 2 (moderate risk): LOPS + PAD, or LOPS + foot deformity, or PAD + foot deformity; IWGDF risk 3 (high risk): LOPS or PAD, and one or more of the following; history of foot ulcer, a lower-extremity amputation (minor or major), end-stage renal disease.12 The final Delphi survey consisted of 50 statements, with a total of 109 items, grouped into recommendations for before, during, and after physical activity/exercise (Supplementary Material 1). A pilot study was conducted with 10 of the panelists to ensure that the survey items were readily comprehensible and that its method of application was appropriate.
A letter of invitation, following the script proposed by Jon Landeta,40 was sent by email to the professionals selected for the expert panel. This letter included a link to access the online survey created using Google Forms. The professionals who accepted this invitation were asked to rate their level of agreement or disagreement with each survey item on a 5-point Likert scale, ranging from 1 = total disagreement, to 3 = neither agreement nor disagreement, and 5 = total agreement. A free text space was also provided for each survey item, where the panelist could make any comment considered appropriate.
The Delphi process consisted of three rounds. After performing the pilot study, which proceeded without suggestions being offered, the first round commenced on 12 June 2021. The panelists were given eight weeks to complete the survey, during which time three reminders were sent, if necessary, to maximize the response rate. After the first round, the researcher responsible for maintaining the participants’ confidentiality downloaded the data into an Excel sheet, which was then analyzed by the entire team. The second and third rounds began on 19 September and 23 October 2021, respectively, inviting responses from the experts who had participated in the previous rounds. In this case the panelists were given two weeks to respond to each round, which included only the items that had not previously produced a consensus, and to provide, if they wished, explanatory comments in the free-form text fields. The final list of recommendations was based on the items for which a consensus was reached.
Statistical analysisThe panelists’ specialties and countries were characterized by absolute and relative frequencies. Their responses to each survey item were analyzed in terms of the percentage of response categories obtained, as is the case in most of the studies cited in the CREDES guide.21 Ratings of 4 or 5 were considered to indicate “agreement” and of 1 or 2 “disagreement.” When a response category was agreed upon by 80% or more of the panelists, the statement was considered to have obtained consensus,41 and it was omitted from the following round of consultation. All analyses were performed using the Microsoft Excel program (Microsoft, Redmond, WA, USA).
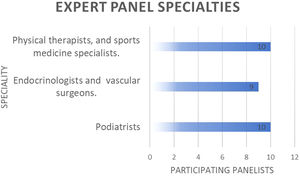
ResultsIn the first round, 29 experts (48.3% response rate) responded to the Delphi survey. By specialties, 10 of these participants were experts in physical activity, sports sciences, or physical therapy, 10 were podiatrists and 9 were endocrinologists, family physicians, or vascular surgeons (Fig. 1). Most were of Spanish nationality, but a significant number of panelists from other countries also took part (Table 1).
In no case did disagreement among the panelists reach 80%, and so none of the items were directly eliminated. The results of the first round are provided in Supplementary Material 2 – S.1. This round took 73 days due to provided extension time. Consensus was reached on 42 items (38.5%), and the remaining 67 items were included in the second round of the survey. After reviewing the panelists’ comments, some items were reformulated or qualified, but there were no fundamental changes to the original meaning (the modifications are detailed in Supplementary Material 2 – S.2). The research team drafted a report on the round 1 results, which was sent to the panelists together with the round 2 survey.
The second round, which took 24 days, during which the panelists received two reminders, achieved a response rate of 100% (n = 29) (Supplementary Material 2 – S.3). A consensus was reached on another 34 of the survey items (31.2%), leaving 33 items to be repeated or reformulated in the third round.
For round 3, which lasted 41 days the response rate was 96.6% (n = 28). The initial deadline was extended, and four reminders were sent to maximize the number of participants. Once the responses were recorded, the final analysis for round 3 was performed (Supplementary Material 2 – S.4). In this round, consensus was reached on 10 additional items (9.2%).
By the end of the third round, the panelists had reached a consensus on 86 items (78.9%) (Table 2). The 23 items (21.1%) for which no consensus was obtained were removed from the final recommendations (Supplementary Material 2 – S.5). These results formed the basis for a final table of recommendations for patients with diabetes for before, during, and after exercise, according to the foot risk presented (Table 3). Pre-exercise recommendations included questions such as when and how to inspect the foot, the initial medical examination of the patient's general condition, the type of sock recommended for patients with PAD, the impact of neuropathy and/or foot deformities on the risk of foot ulcers (IWGDF 0–3), and the most appropriate type of exercise, taking into account its intensity, duration, frequency and progression. Recommendations on aspects to consider during and after exercise/physical activity included the use of custom-made plantar orthoses, the prescription of footwear, the types of exercise to perform, and the timetable for a return to activity after an ulceration.
Delphi survey items that reached consensus, by consultation round.
Bold type: main statement; grey table cell: round consensus item; black table cell: title thematic blocks.
List of recommendations by IWGDF risk.
Bold type: main statement; Black table cell: title thematic blocks.
The experts’ consensus recommendations for patients with diabetic foot are summarized as follows. Before starting any physical activity, all patients should undergo a prior check-up of both feet, and those classified as risk 2 or 3 should repeat this check-up during and after the activity. In addition, every patient should receive a prior assessment of their general condition and of any keratotic lesions or excessive dryness in different areas of the foot.
When neuropathy and/or PAD are observed, the socks worn should have no seams, rubber, or elastic, and the choice of footwear should be guided by a professional. Aerobic exercise is recommended, with strength and flexibility training adapted to each type of foot at risk, such as the inclusion of rehabilitation exercises for patients with motor neuropathy or the practice of aquatic exercise rather than walking, thus avoiding pressure on the foot, for those at high risk of ulceration. Orthopedic treatment is recommended for patients at risk 3, while those at risk 2 or 3 should receive a check-up 15 days after starting physical exercise and monthly at the location where the exercise takes place.
These recommendations are consistent with those of the American Diabetes Association,38 stating that patients with type 2 diabetes should perform three or more sessions of moderate-to-vigorous-intensity physical activity per week, for a total of at least 150 min and avoid two or more consecutive days without physical activity/exercise. The latter recommendations, however, do not provide enough data on appropriate exercises for people at high risk of foot ulceration.
Shortly after the completion of this study, the American College of Sports Medicine published new recommendations, with clarifications regarding the types of exercise appropriate for patients with peripheral neuropathy, among other aspects also addressed in our study. These guidelines are consistent with the conclusions drawn from our study.42 However, these recommendations are not specifically adapted to different risk categories for diabetic foot.
The IWGDF39 recommends various forms of foot-related exercises, such as strengthening and stretching, to alleviate risk factors for the incidence of foot ulceration,43–46 but their recommendations do not provide recommendation on frequency, and do not differentiate between foot risk categories. In the present study, more closely-targeted recommendations have been obtained, for example that patients with neuropathy (IWGDF risk 1, 2, or 3) should perform exercises to improve static and dynamic balance, beginning with low or moderate-intensity aerobic exercise appropriate to the patient's age and physical characteristics. If the patient presents with motor neuropathy, regardless of the degree of risk, rehabilitation exercises should be performed to limit the progression of the deformities. In those with mild to moderate PAD (IWGDF risk 1, 2, or 3), the healthcare provider should consider adding specific exercises to improve vascular function.
Several publications detail the key footwear aspects to consider.47–49 Others support the use of tilting soles and custom-made insoles.48,50 However, there is limited evidence about what type of shoes and socks should be recommended, that takes into account the condition of the patient's foot and their medical history. Our Delphi study addresses this information gap, compiling expert advice on appropriate socks and footwear during physical activity, according to the foot risk, taking into account possible complications like neuropathy, foot deformities, and PAD. For example, the type of sock should be tailored to the physical activity performed, but all cases should be light-colored (to visualize any bleeding more easily), clean, seamless, and with no tight-fitting elastics. If the patient has PAD and or neuropathy, the socks should have no seams, rubber, or elastic that could restrict circulation. However, consensus was not possible on certain aspects, such as the type of sock most appropriate for patients. We obtained no specific recommendations regarding shoes, but it was agreed that "a professional should always be consulted about the type of footwear before the patient begins an exercise regimen”.
A question that remains to be clarified is that of the appropriateness of exercise by patients with an open ulcer. To date, no guidelines have specifically addressed when and how patients should return to physical activity after an ulceration, although some studies have made observations in this regard. For example, Lyu et al.,51 argue that the early adoption of walking exercise can improve outcomes in patients with PAD. However, the current evidence is scarce and heterogeneous, as reflected in two systematic reviews which conclude that the available data do not allow any recommendations to be made on exercise in patients with diabetic foot ulcers.14,52
Pending new studies that address this topic, in the presence of PAD, our study offers expert recommendations on mobilizing the foot when there is ulceration. Another current issue is when and how to start or resume exercise after a recent ulceration. Our panelists agreed that patients should gradually ease into their exercise program, a view that is consistent with the results of other studies, suggesting that a well-controlled activity regimen that includes walking, maintaining balance, and strengthening the legs can positively influence the patient's health and function.27
The recommendations for which we failed to reach consensus reflected a similar lack of agreement in the scientific literature, relating to aspects such as the correct way to cut nails, the best type of socks for patients with neuropathy and PAD, and the use of smart watches or mobile apps to monitor blood oxygen (due to the absence of available devices with sufficiently reliable measurements). Given the dearth of quality studies or evidence on clinical efficacy, the panelists also failed to reach a consensus on recommendations for exercise in patients with IWGDF risk 2 or 3, the use of static pedals, the best type of surface on which to practice physical activity, or the use of a definitive offloading orthosis within 15 days of ulceration.
Some of these recommendations for which no consensus was reached, such as the type of sock or the correct cut for nails, are specific to the field of podiatry, while others (for example, the frequency and intensity of mobility exercises, the use of static pedals by patients at high risk of ulceration) correspond more to the field of sports medicine. Nevertheless, in our Delphi study, the relevant specialties were well distributed among the panelists. The lack of consensus regarding the more specific items might be due to the neutral position adopted by the experts who lacked specialist knowledge in these areas, a factor that may have introduced some bias into the study. To counter this possibility, we believe that recommendations on specific aspects of the foot or on types and repetitions of exercises should be agreed upon by a panel composed of experts within a single discipline.
The limitations to our research are those inherent to this type of qualitative study, such as the constraints of a close-ended survey, although free text space was provided for each item for panelists to freely comment. Another limitation, is the convenience nature of the sampling procedure used and the voluntary participation of the experts. Either or both of these factors may have introduced a selection bias. The low response rate in the initial selection of experts may be due to the difficulty getting in touch with the experts, because contact information was retrieved from their scientific publications, which in some cases may have been outdated. Consequently if the invitation was never received, this too would have constituted a selection bias. Another limitation is the fact that patients were not included in the panel or consulted as part of the study. However, we intend to conduct a follow-up study in which the recommendations obtained will be shared and managed by a group of people with diabetes, to better adapt the recommendations and the vocabulary to their needs.
Among the study's main strengths, to our knowledge this is the first set of expert recommendations to be proposed that address, in a clear and structured way, how patients should exercise, in accordance with their individual foot risk. Another strong point of this study is the high response rate obtained in each of the three rounds of the survey process (only one of the participating experts did not complete all three rounds). The Delphi methodology in itself represents another important strength, as its participatory nature favors the acceptability of the recommendations among multidisciplinary practitioners and their implementation in a range of clinical settings. On the other hand, these exercise recommendations have been formulated solely with the consensus of clinical experts; our research design method is not intended to be a replacement for robust, high-quality clinical trials, but rather a clinical guide to determining the patient's status and a starting point to consider important aspects for the individual patient. Further studies are needed to evaluate the ease of implementation of the recommendations, the degree of patient adherence, the long-term benefits, and the safety and efficacy of different types of physical exercise for this population.
ConclusionThis Delphi study generated recommendations based on the consensus of international experts for physical activity and exercise by patient with diabetes at risk of ulceration. These recommendations take into account the state of the foot and the patient's history and status before physical activity. They include guidance such as when and how the foot should be examined, an initial consideration of the patient's general condition, the type of sock to be worn by those with PAD, neuropathy, and foot deformities, considering also the risk of foot ulcers (IWGDF risk 0–3), the type of exercise to be performed (in terms of intensity, duration, frequency, and progression), and recommendations for during and after physical activity/exercise, such as the use of custom-made plantar orthoses and shoe prescription, and the considerations for returning to physical activity after an ulceration.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors thank the following expert panelists for their contributions: Doctors Rauf Nouni García, Jose Ignacio Blanes Mompó, Diego Pastor Campos, Ruth Sánchez Ortiga, Dídac Mauricio, Yolanda García Álvarez, Sonia Hidalgo Ruiz, Javier Aragón Sánchez, Nalini Campillo Vilorio, Manuel González Sánchez, Juan Pedro Sánchez Ríos, María Reina Bueno, Matilde Monteiro Soares, Ana Esther Levy Benasuly, Gabriel Rivera San Martín, Laura Carrasco Cortijo, Almudena Cecilia Matilla, Alex Garrido Méndez, José Antonio Rubio García, Piergiorgio Francia, Richard Collings, Sheri Colberg, Luca Dalla Paola, Romeu Mendes, Michael J Mueller, Jaap van Netten, Stephanie Woelfel, and Nina Petrova.