Posterior capsule tightness (PCT) is associated with shoulder pain and altered shoulder kinematics, range of motion (ROM), external rotation (ER) strength, and pain sensitization.
ObjectiveTo assess the effects of two interventions on shoulder kinematics, Shoulder Pain and Disability Index (SPADI) scores, ROM, strength, and pressure pain threshold (PPT) in individuals with PCT and shoulder impingement symptoms.
MethodsIn this prospectively registered randomized controlled trial 59 individuals were randomized to either an Experimental Intervention Group (EIG, n=31) or a Control Intervention Group (CIG, n=28). The low flexion (LF) test was used to determine the presence of PCT. Shoulder kinematics, SPADI scores, internal rotation (IR) and ER ROM, ER strength, and PPT were measured pre- and post-treatment. Those in the EIG received an intervention specific to pain and PCT and those in the CIG received a non-specific intervention, both 4 weeks in duration.
ResultsIndividuals in the EIG demonstrated more scapular upward rotation (P=.03; mean difference (MD)=3.3°; 95% Confidence Interval (CI)=1.3°, 4.9°) and improved value on the LF test (P=.02; MD=4.6°; 95%CI=0.7°, 8.6°) than those in the CIG after treatment. Both groups presented less anterior (P<.01; MD=-0.7mm; 95%CI=-1.3mm, -0.2mm) and superior (P<.01; MD=-0.5mm; 95%CI=-0.9mm, -0.2mm) humeral translations, decreased SPADI score (P<.01; MD=-23.6; 95%CI=-28.7, -18.4), increased IR ROM (P<.01; MD=4.6°; 95%CI=1.8°, 7.8°) and PPTs for upper trapezius (P<.01; MD=60.1kPa; 95%CI=29.3kPa, 90.9kPa), infraspinatus (P=.04; MD=47.3kPa; 95%CI=2.1kPa, 92.5kPa), supraspinatus (P<.01; MD=63.7kPa; 95%CI=29.6kPa, 97.9kPa), and deltoid (P<.01; MD=40.9kPa; 95%CI=12.3kPa, 69.4kPa) after treatment.
ConclusionThe experimental intervention was more effective at improving PCT as measured through changes in the LF test. No benefit of the specific approach over the non-specific intervention was noted for the remaining variables.
Shoulder pain is one of the most common musculoskeletal complaints for which people seek treatment.1,2 Typical signs and symptoms include pain during reaching, weakness, and interrupted sleep.3 Often called Shoulder Impingement Syndrome (SIS), this condition is associated with several biomechanical and impairment-level factors including altered scapula or humerus kinematics, range of motion (ROM) and strength deficits, soft tissue tightness, and peripheral or central sensitization.4-10
Loss of glenohumeral joint internal rotation (IR) ROM is common in individuals with shoulder pain, in particular overhead throwing athletes,6,7,11,12 but also in the general population.4,8,13-15 Loss of glenohumeral IR is attributed to posterior shoulder muscle or posterior capsule tightness (PCT).7,8,16-18 Importantly, PCT is also associated with decreased rotator cuff strength,7 altered scapula and humerus kinematics,8,13,19-21 and sensitization8 – the same alterations noted in those with SIS. This interaction among PCT, SIS, and biomechanical and impairment-level factors suggests that an intervention specifically targeting PCT may reduce symptoms and improve movement in those with shoulder pain.
Treatment specificity, aimed to directly influence the structure contributing to symptoms, should result in better outcomes over less time. Interventions targeting PCT have demonstrated improved shoulder ROM, pain, and function,11,12,14 and there is moderate22 and weak23 evidence that posterior shoulder muscle stretching improves IR ROM deficits. Combining muscle stretching with targeted PCT mobilization improves IR ROM in those with shoulder pain,24 but the effects of specific interventions targeting PCT in individuals who also have shoulder pain has not been reported. Because PCT is regularly associated with SIS, evaluating an intervention that is specific to PCT in the presence of shoulder pain has the potential to provide valuable and clinically relevant information for those treating individuals with shoulder pain.
This study provides treatment to individuals with both PCT and shoulder pain, randomized to specific intervention (Experimental) or general intervention (Comparison) groups. To broadly explore the influence of this targeted treatment approach, the study evaluated shoulder function, kinematics, strength, ROM, and sensitization before and after the two different interventions. We hypothesized that the group receiving treatment specific to common impairments (PCT and external rotation (ER) strength deficit) would demonstrate improved kinematics and decreased impairments compared to the non-specific treatment group.
MethodsStudy designThis was a randomized clinical trial with one blinded assessor. The primary investigator, blinded to group assignment, assessed PCT, IR and ER ROM, ER strength, scapular and humeral kinematics, and pressure pain threshold (PPT) before and after the interventions were completed. Two additional investigators randomized participants into groups and provided the interventions. Participants were blinded to their group assignment.
Participants and settingParticipants were recruited through fliers posted at the local university, orthopedic clinics, and surrounding community; 153 individuals responding between March/2015 and March/2016 were evaluated for eligibility. Enrollment was voluntary with no incentives given to participants.
Participants were required to have SIS symptoms for at least 3 months, defined as being positive for at least 3 of the following:25-31 positive Neer,32 Hawkins,33 or Jobe tests,34 pain with passive or isometric resisted shoulder ER,30,35 and pain with active shoulder elevation.36 Participants were required to have PCT, determined with the Low Flexion Test (LFT).8,37 The LFT is performed with the individual's arm supported at 60° of flexion before allowing glenohumeral IR to reach the end of passive motion. Subsequently, a digital inclinometer measures the angle between the forearm and horizontal.8,37 A 7° decrease compared with the contralateral side indicates PCT.38 The LFT is a valid and reliable measurement specific to the posterior glenohumeral capsule.37-40 For kinematic data collection, participants were also required to have ∼150° of active arm elevation.
Exclusion criteria were: pregnancy; positive Sulcus,41 Speed,26,42 Apprehension43 or Anterior Drawer test;44 history of traumatic shoulder pathology, fracture, shoulder surgery, adhesive capsulitis, scoliosis, or systemic illness; bilateral symptoms; radiating pain; body mass index >28kg/m2; receiving physical therapy in the last 6 months; analgesics or muscle relaxants taken within 72 hours of the examination;10 or steroid injection in the last 6 weeks.45
The study was approved by the Ethics Committee of the Universidade Federal de São Carlos, SP, Brazil (number 860.648) and prospectively registered at ClinicalTrials.gov (NCT02353442). Data collection was performed in the Laboratory of Analysis and Intervention of the Shoulder Complex at Universidade Federal de São Carlos, SP, Brazil. Participants signed an informed consent to enroll.
RandomizationA total of 59 individuals were included and randomly divided into two groups: Experimental Intervention Group (EIG, n=31) or Comparison Intervention Group (CIG, n=28), using www.randomization.com (Fig. 1).
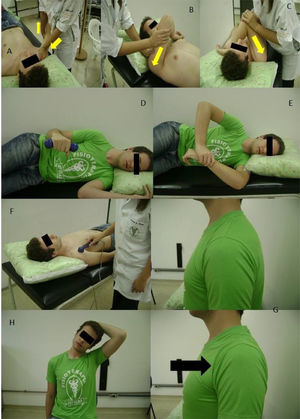
InterventionExperimental Intervention Group. This intervention consisted of three targeted techniques on the involved shoulder: anterior-posterior directed glenohumeral mobilization, active resistance exercise for the shoulder external rotators, and posterior capsule stretching. Mobilizations began with Maitland grades III and IV12,14 with the participants in supine and a towel under the scapula. Grades were progressed according to patient pain tolerance and therapist perception of increased flexibility (Fig. 2A-C).11,14,35 The mobilization oscillatory force was maintained for 30 seconds,11 followed by a 30-second rest,11 and repeated until a total of 5 minutes of mobilization was achieved. Anterior-posterior mobilizations specifically target the tight posterior capsule as measured with the LFT. Resisted ER exercise was performed in side lying with neutral glenohumeral joint and 90° of elbow flexion46,47 (Fig. 2D). Participants started without weight, and progressed to 0.5kg, 1.0kg, 1.5kg, and 2kg based on self-assessment and therapist judgement. Participants performed three sets of 10 repetitions27 with 30-seconds between sets. Resisted ER targets an impairment regularly noted in those with SIS. The posterior capsule stretch was performed with the participant lying on their involved side with the shoulder and elbow in 90° of flexion, and then applying a passive glenohumeral IR force with their opposite hand until a posterior shoulder stretch was felt. The stretch was held for 30 seconds (Fig. 2E) and repeated three times with 30-seconds between repetitions.27 This stretch targets the posterior capsule and posterior shoulder muscles, two soft tissues that contribute to decreased IR ROM.11,12
Protocols for the groups: Experimental group: A, B, and C) Progression of posterior capsule mobilization (arrows indicate the mobilization directions), D) Strengthening of the external rotators, E) Posterior capsule stretching; Comparison group: F) Sham ultrasound, G) Scapular squeezing exercise, H) Stretching of the upper trapezius.
Comparison Intervention Group. This intervention also consisted of three techniques: sham ultrasound, active scapular retraction, and upper trapezius (UT) stretching. Participants received five minutes of sham ultrasound to the anterior shoulder in supine (Fig. 2F). Afterwards, they completed three sets of 10 repetitions of isotonic scapular retraction exercises without external resistance by squeezing both scapulae together while sitting (Fig. 2G). The UT stretching was performed three times while sitting. Participants flexed and rotated their cervical spine to the opposite side and same side, respectively, of the ipsilateral UT,48 and held this position for 30 seconds with 30-second rests between repetitions (Fig. 2H).
Both groups received this physical therapist supervised intervention three times per week (approximately 20min each session) for 4 weeks. PCT and pain were assessed at the beginning and end of each session with the LFT and a Visual Analog Scale (VAS), respectively. Anchors for the 0 to 10 VAS were ‘No Pain’ (0) and ‘worst pain imaginable’ (10). Treatments were stopped if participants reported no pain for two consecutive sessions and the LFT was no longer >7° from the uninvolved side. These participants received their postintervention assessment by the primary assessor at this session.
Outcome measuresReliability of the measuresTen asymptomatic individuals (5 women, 5 men) and 10 individuals with shoulder pain (5 women, 5 men) were evaluated by the primary assessor on 2 occasions, separated by 4 weeks. Between-day reliability of the SPADI, LFT, IR and ER ROM, ER strength, and PPT measurements was determined using the Intraclass Coefficient Correlation (ICC3,2), Standard Error of the Measurement (SEM), and Minimal Detectable Change90% (MDC90).
3DScapular kinematics and humeral translationsScapular kinematic and humeral translation data were captured and analyzed with the Flock of Birds® (miniBird®) hardware (Ascension Technology Corporation, Burlington, VT) integrated with MotionMonitor™ software (Innovative Sports Training, Inc. Chicago, IL). The methods used to capture 3D scapular and humeral motion are described elsewhere.8,9,30,49,50 Scapular IR/ER, upward/downward rotation, and anterior/posterior tilt relative to the trunk were described using a YX'Z” Euler sequence.51 Humeral plane of elevation, elevation angle, and IR/ER were described with a YX'Y” Euler sequence. For humeral translations, the helical axis was determined and its anterior-posterior and superior-inferior vector components used to describe humeral head position.50 During data capture, participants performed three repetitions of sagittal plane arm elevation and lowering while standing. This procedure has been shown to be reliable in individuals with SIS.28
Shoulder pain and disabilities index (SPADI)The SPADI assessed shoulder pain and function.52 It is reliable for assessing individuals with shoulder pain.53 The final score is provided as a percentage and a maximum score of 100 implies the worst possible condition.52 Between-day ICC, SEM, and MDC90 were 0.9, 5.8, and 13.5, respectively.
Glenohumeral IR and ER range of motionGlenohumeral IR and ER ROM were quantified with a digital inclinometer (Acumar ™, Lafayette Instrument Company, Lafayette, IN). Participant motion was measured in supine in 90° of arm abduction and 90° elbow flexion. The inclinometer was positioned on the dorsal forearm surface for IR ROM and palmar surface for ER ROM. Participants actively rotated into maximum IR and ER ROM, and the amount of motion was read and recorded by a second assessor.54,55 A second investigator stabilized the scapula during the IR ROM measurement.8,54 Each measurement was taken twice.8 Between-day ICC, SEM, and MDC90 were 0.8, 5.1°, and 11.7° for IR ROM and 0.9, 3.3°, and 7.7° for ER ROM, respectively.
Shoulder ER strengthShoulder ER strength was quantified using a handheld dynamometer (Lafayette, IN, USA) with individuals seated, shoulder at 0° abduction/adduction, and elbow at 90° of flexion.8 The dynamometer was positioned between the dorsal wrist surface (2cm below the radial styloid process) and a wall. Two submaximal repetitions with 10-second rest interval were used for familiarization, followed by two maximal 5-second isometric contractions with a 30-second rest between repetitions. Verbal encouragement was used to maximize effort during data collection.8 A second investigator recorded the results to maintain blinding. Between-day ICC, SEM, and MDC90 were 0.9, 7.7 N, and 17.9 N, respectively
Pressure Pain Threshold (PPT)A digital pressure algometer (model OE-220, ITO, Japan) was used to determine PPT in the muscle bellies of the UT, infraspinatus, supraspinatus, middle deltoid, levator scapulae, and tibialis anterior. These shoulder muscles were selected because they are often painful to palpation in those with shoulder pain and the tibialis anterior was evaluated as a remote site to assess central sensitization.9,10 The precise testing location for each muscle is described elsewhere.10 Between-day ICC, SEM, and MDC90 ranged from 0.7-0.9, 25.1kPa-142.6kPa, and 58.3kPa-330.7kPa, respectively.
Sample SizeTwenty-five individuals per group were required to identify a clinically meaningful angular change of 5° in scapular upward rotation (UR) and achieve a statistical significance level of 0.05 with power of 0.8.28,30,56 With potential attrition of 15%, we targeted 29 participants per group.
Statistical analysisData were analyzed using the SPSS statistical 17.0 version. Mean ± standard deviation (SD) values were calculated for all variables and used for statistical analysis. Data were normally distributed (P>.05) as verified by Kolmogorov–Smirnov test. For scapular IR, UR, and posterior tilt (PT) and humeral anterior and superior translations, a mixed repeated measures 3-factor Analysis of Variance (ANOVA) tested for group (EIG and CIG) x time (pre and postintervention) x angle (rest, 30°, 60°, 90°, 120°) interactions. If no interactions were observed, the main effect of time was analyzed. For SPADI, LFT, ROM, ER strength, and PPT, a mixed repeated measures 2-factor ANOVA tested for interactions of group x time. If no group x time interaction was observed, the main effect of time was analyzed. Bonferroni post-hoc analysis was used when indicated and P<.05 was considered statistically significant.
All data were analyzed according to the principle of Intention-to-Treat. Missing values were imputed using the expectation-maximization method, which estimates the values to impute with an algorithm based on initial and observed values.57
ResultsTable 1 reports descriptive data for both groups. Seven individuals were lost to postintervention assessment because of undisclosed personal reasons (Fig. 1). The average number of treatment sessions was 11.3 ± 1.4 and 11.3 ± 1.1 for the EIG and CIG, respectively. Two individuals from EIG received fewer than 12 sessions because they achieved the pre-determined pain and LFT thresholds to stop treatment.
Descriptive data of the individuals.
| Experimental Intervention group (n=31) | Comparison Intervention group (n=28) | |
|---|---|---|
| Sex | 9 women; 22 men | 11 women; 17 men |
| Age (years)* | 41.1 ± 12.9 | 40.1 ± 11.8 |
| Height (m)* | 1.7 ± 0.2 | 1.7 ± 0.1 |
| Weight (kg)* | 76.9 ± 13.7 | 76.19 ± 14.9 |
| Evaluated shoulder | 27 dominant; 4 non-dominant | 25 dominant; 3 non-dominant |
| Duration of pain (months)† | 41.9 ± 53.9 (3-180) | 40.2 ± 35.0 (3-120) |
For scapular IR and PT, triple and double interactions were not significant (P>.05) and there was no main effect of time (P>.05).
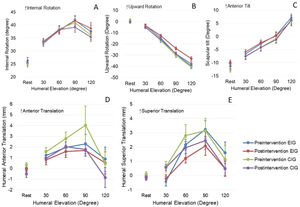
For scapular UR, there was no significant triple interaction (P=.68). However, there was a significant group x time interaction (P=.03), with the EIG having greater UR than the CIG at postintervention (3.1°) (Fig. 3B). An angle x time interaction was also found (P<.01) with increased UR at postintervention compared to preintervention at 90° (3.2°) and 120° (4.8°) of elevation (Fig. 3B).
Pre and Postintervention scapular internal rotation (A), upward rotation (B), and tilt (C); and humeral anterior translation (D) and superior translation (E) during elevation of the arm in the sagittal plane for both groups. Values are mean (standard error). Abbreviations: EIG, experimental intervention group; CIG, comparison intervention group.
For humeral anterior and superior translations, there was no significant triple interaction (P>.05) or significant group x time or angle x time interactions (P>.05). However, a main effect of time was demonstrated for both translations (P<.01). Less anterior and superior humerus translation (-0.7mm and -0.6mm, respectively) was found at postintervention when compared to preintervention (Fig. 3D-E).
SPADI questionnaireThere was no significant group x time interaction (P=.07), but the main effect of time showed decreased SPADI scores for both groups at postintervention (P<.01, Table 2).
Results of SPADI, Low Flexion Test, Internal and External Rotation ROM, ER strength, Pressure Pain Threshold (kPa) of each muscle for both groups at Preintervention and Postintervention Evaluations.
| Experimental | Comparison | Between-Group Differences in Change Scores | |
|---|---|---|---|
| SPADI | -8.6 (-18.2, 1.1) | ||
| Preintervention | 46.2 ± 21.7 (37.9, 54.5) | 45.5 ± 24.3 (36.8, 54.2) | - |
| Postintervention | 18.0 ± 13.8(11.4, 24.6) | 26.5 ± 22.4(19.6, 33.5) | - |
| Low Flexion test (°) | 4.7 (0.7, 8.6) | ||
| Preintervention | 18.2 ± 6.7 (15.6, 20.9) | 19.2 ± 8.1 (16.4, 21.9) | - |
| Postintervention | 22.6 ± 8.7(19.9, 25.3) | 17.9 ± 6.1(15.1, 20.8) | - |
| Internal Rotation (°) | 2.35 (-4.14, 8.8) | ||
| Preintervention | 60.2 ± 13.1 (55.8, 64.1) | 53.7 ± 11.7 (48.9, 58.4) | - |
| Postintervention | 62.8 ± 14.2 (58.3, 67.3) | 60.5 ± 10.1 (55.8, 65.2) | - |
| External Rotation (°) | -6.8 (-14.6, 0.9) | ||
| Preintervention | 87.7 ±16.1 (81.3, 94.1) | 88.8 ± 19.3 (82.1, 95.5) | - |
| Postintervention | 81.8 ± 14.6 (76.4, 87.2) | 88.6 ± 15.3 (82.9, 94.3) | - |
| External Rotation strength (N) | 11.9 (-3.9, 27.7) | ||
| Preintervention | 95.0 ± 32.2 (83.5, 116.6) | 89.7 ± 32.0 (77.5, 101.8) | - |
| Postintervention | 101.6 ± 27.9 (90.7, 112.5) | 89.7 ± 32.8 (78.3, 101.2) | - |
| Upper Trapezius (kPa) | -68.9 (-142.3, 4.5) | ||
| Preintervention | 304.3 ± 134.1 (262.8, 345.8) | 282.8 ±114.8 (239.1, 326.4) | - |
| Postintervention | 355.6 ± 150.1* (299.0, 412.1) | 351.7 ± 164.6* (292.2, 411.2) | - |
| Infraspinatus (kPa) | -62.3 (-148.7, 24.1) | ||
| Preintervention | 409.9 ± 192.6 (344.7, 463.2) | 342.8 ± 126.9 (280.5, 405.2) | - |
| Postintervention | 436.3 ± 176.7* (368.7, 503.9) | 405.1 ± 199.7* (334.0, 476.3) | - |
| Supraspinatus (kPa) | 8.4 (-70.1, 86.8) | ||
| Preintervention | 309.7 ± 138.8 (267.6, 351.9) | 259.1 ±118.8 (215.6, 304.3) | - |
| Postintervention | 352.8 ±150.0* (298.7, 406.8) | 344.4 ±150.6* (287.5, 401.3) | - |
| Deltoid (kPa) | 5.7 (-65.9, 77.3) | ||
| Preintervention | 305.5 ± 142.1 (261.4, 349.6) | 295.2 ± 96.5 (248.8, 341.7) | - |
| Postintervention | 344.11 ± 133.20* (294.8, 393.4) | 338.4 ± 141.4 (286.5, 390.3) | - |
| Levator Scapulae (kPa) | -14.6 (-63.5, 34.2) | ||
| Preintervention | 250.7 ± 123.3 (212.3, 289.1) | 269.2 ± 101.8 (232.4, 305.9) | - |
| Postintervention | 252.8 ± 84.7 (212.4, 293.2) | 267.4 ±102.7 (228.7, 306.1) | - |
| Anterior Tibialis (kPa) | 30.0 (-99.3, 159.4) | ||
| Preintervention | 709.0 ± 246.4 (623.1, 794.9) | 690.3 ± 230.2 (599.9, 780.7) | - |
| Postintervention | 745.9 ± 239.3 (656.8, 835.1) | 715.9 ± 256.9 (622.1, 809.7) | - |
Results are mean ± standard deviation (95% confidence interval).
There was a significant group x time interaction for PCT (P=.02). The EIG showed increased LFT values at postintervention when compared to the CIG (P=.02, Table 2). Between-day ICC, SEM, and MDC90 were 0.8, 2.7°, and 6.48°, respectively.
Glenohumeral IR and ER range of motionNo group x time interaction was observed for IR ROM (P=.14). However, the main effect of time demonstrated greater IR at postintervention (P<.01) when compared to preintervention (Table 2).
No significant interactions (P=.32) or main effect of time (P=.28) were demonstrated for ER ROM (Table 2).
Strength of the shoulder external rotatorsShoulder ER strength did not show a significant group x time interaction (P=.23) or main effect of time (P=.22, Table 2).
Pressure pain thresholdNo group x time interaction was demonstrated for PPT (P>.05). A main effect of time (P<.05) was noted for UT, infraspinatus, supraspinatus, and deltoid with increased UT (60.1kPa), infraspinatus (47.3kPa), supraspinatus (63.7kPa), and deltoid (40.9kPa) PPTs after the intervention period regardless of group assignment (Table 2).
DiscussionThis study showed that a specific intervention targeting PCT was successful in improving PCT and scapula UR, two factors commonly noted in those with shoulder pain. The magnitude of increased scapula UR was not considered to be clinically meaningful. Our findings also demonstrated improved humeral translations, SPADI scores, ROM, strength, and PPT outcomes in both the specific and the non-specific intervention groups, with no between-group differences in these factors.
For scapular kinematics, the EIG showed increased UR after intervention. However, the improvement was below the minimal clinically important difference (MCID=5°) described in the literature.28,30,56,58 Other studies evaluating the effects of different treatment approaches on scapular kinematics in individuals with shoulder pain,9,29-31,33,59-62 have shown inconsistent results. Some studies have demonstrated no scapula UR differences,30,33,61,62 while others have noted increased scapula UR that was not clinically meaningful,9,29,31,60 consistent with the present study. The variability in scapular UR described in individuals with shoulder pain44,63,64 may contribute to the lack of clinically important changes. Although reliability of scapula kinematics was not estimated for the present study, we believe the standardized data collection methods, broadly used in many previous studies,9,29-31,33,56,58 allow us to assume consistency of kinematic data.
Anterior and superior humeral head translations decreased in both groups after intervention (-0.7 mm and -0.6 mm, respectively). The translation change in the present study is within the between-day SEM confidence interval previously reported for humeral translations in individuals with shoulder pain (0.3mm to 2.3mm).50 Without MDC and MCID calculations for humeral translations in individuals with PCT and shoulder pain in the literature, we are unable to suggest that the decrease in anterior and superior translations is clinically meaningful. A recent study8 showed that individuals with shoulder pain only demonstrated less anterior translation (1.7mm) and lower SPADI score (22.4) compared to individuals with pain and PCT. Considering the limited dimensions of the subacromial space (∼7mm),65 the small translation changes noted may have clinical relevance for the pain and function improvement on the SPADI in both groups.
The SPADI scores demonstrated decreased pain and improved function in both groups after intervention. A change of 8-13 points on the SPADI is considered clinically significant53 and the decrease of 23.6 points in this study, combined across groups, suggests a meaningful improvement in pain and function. Although significant between-group differences were not demonstrated, the EIG showed a reduction of nearly 10 points more than the CIG, suggesting that a specific intervention might be better than a non-specific intervention to improve pain and function in those with PCT and shoulder pain.
The EIG LFT increased 4.3° after treatment, which may indicate less tightness of the posterior capsule from the targeted treatment approach. The change in the EIG group surpassed the SEM but not the MDC90 calculated in this study. With no previous studies reporting an MCID for the LFT, we are unable to suggest that the change seen was meaningful to participants. In addition, with two treatments in the EIG protocol targeting PCT, the change in LFT in the EIG cannot be directly attributed to either mobilization or stretching.
Both groups had increased glenohumeral IR ROM at postintervention. This result did not support our hypothesis and is inconsistent with previous studies that demonstrated increased glenohumeral IR ROM after specific posterior shoulder mobilizations and stretching.11,12,14 The different techniques used compared to the previous investigation's technique may explain the divergent results. Cools et al.11 used passive stretching for 15 min and also included cross-body stretching. This protocol11 may apply more stress on the capsule and posterior shoulder muscles to increase IR ROM. The intervention in our study was supervised, but we cannot ensure that the capsule was adequately targeted during the sleeper-stretch. Patient's tolerance to pain might have influenced our results as well. Another study12 included a home care approach in addition to physical therapy sessions to increase IR ROM in individuals with internal impingement and PCT. In this case, the number of sessions (3 times per week with therapist + daily home exercises) may explain the IR ROM increase.
The fact that we did not control mobilization and stretching loads might have contributed to the IR ROM results. Although no techniques were used in the CIG to specifically increase IR ROM, they improved after treatment. This change may relate to decreased SPADI scores in this group, considering that IR ROM was previously associated with shoulder pain and PCT.8 It is important to note that this group also had less IR ROM at preintervention compared to EIG, which may explain the larger, although not significant, change in motion.
Although ER ROM values in the EIG were lower at postintervention, the groups were not statistically different. Because neither intervention included a specific technique to influence ER ROM, this 5.9° decrease in the EIG lacks a direct interpretation. It is possible that while performing ER strengthening the EIG group developed a movement pattern that avoided end-range ER motion, and this influenced the ER measurement. Measurement error at postintervention may also explain this change but we would expect error to be evident in both groups, not only for the EIG.
Shoulder ER strength in the EIG increased mildly after the intervention, as expected with performing resistance exercises, but the increase was not enough for statistical significance between groups. It is possible that the amount of resistance used was not adequate to promote larger strength increases. Participants self-selected the amount of resistance for this exercise and perhaps using a 10-Repetition Maximum as in prior studies66,67 may have resulted in greater and more effective resistance loads being applied.
Both groups had improved UT, infraspinatus, supraspinatus, and deltoid PPT. The long mean duration of pain (∼40 months) for individuals in the present study does not appear to have compromised their ability to improve with treatment. These results also suggest that individuals were mostly free of central sensitization despite the chronic nature of symptoms. It is possible that the active treatments in both interventions explains some PPT improvement, considering the critical role movement has in the rehabilitation of individuals with shoulder pain.9,30 With the MCID for PPT improvements in individuals with shoulder pain unknown, we cannot be certain that a meaningful improvement in sensitivity can be attributed to the interventions.
The natural recovery process, the placebo effect and the real effect of the intervention are potential explanations for the improvement observed in the CIG. Future studies could evaluate natural recovery by including a control group and adding long-term follow-up testing. Although the comparison group received a non-specific intervention, they performed active exercise and stretching, which supports the importance of motion to decrease shoulder dysfunction. The placebo effect could also have contributed to the CIG improvement, with the patient's expectations and the therapist beliefs influencing outcomes.68
ConclusionThis study showed that the specific intervention was more effective for improving PCT in individuals with PCT and SIS, as assessed by LFT. Increased scapular UR was also observed in the experimental group following treatment, but these changes were not considered clinically meaningful. Both interventions were effective in changing humeral translations and improving SPADI scores, IR ROM, and local pain sensitivity in individuals with shoulder pain and PCT, demonstrating that there was no additional benefit to a specific targeted intervention on these variables.
The authors would like to thank the volunteers who participated in this study. This study was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo (process 2014/10355-3; 2014/18118-0 and 2014/24388-0) and by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES).
This study was approved by the Institutional Review Boards of the Federal University of São Carlos (number 860.648).
This study was registered at ClinicalTrials.gov: identifier NCT02353442 (https://clinicaltrials.gov/ct2/history/NCT02353442?V_6=View)