Recent evidence suggests that internal impingement, or rotator cuff tendon deformation against the glenoid, occurs during overhead motions and may therefore be a mechanism of pathology even in non-athletes. Clinically, knowing how movement impacts potential injury mechanisms would be useful to guide movement-based treatment strategies.
ObjectiveTo compare the distance between the glenoid and rotator cuff footprint between two groups classified based on scapulothoracic upward rotation (UR) magnitude (i.e., low, high) at 90° humerothoracic elevation.
MethodsShoulder kinematics were quantified during scapular plane abduction in 60 participants using single-plane fluoroscopy. Of these, 40 were subsequently classified as having high or low scapulothoracic UR based on the sample's distribution. The minimum distance between the glenoid and rotator cuff footprint was calculated along with the locations of closest proximity (i.e., proximity centers). Minimum distances and proximity center locations were compared between groups using 2-factor mixed-model ANOVAs. The prevalence of glenoid-to-footprint contact was also compared.
ResultsGlenoid-to-footprint distances consistently decreased as humerothoracic elevation angle increased, and the anterior aspect of the footprint was closest to the posterosuperior glenoid. Minimum distances were not significantly different between UR groups (p≥0.16). However, group differences existed in proximity center locations (p<0.01). Glenoid-to-footprint contact was identified in 75.0% of participants at an average (SD) of 133.6° (3.2°) humerothoracic elevation.
ConclusionThe results of this study suggest that decreased UR as classified and assessed in this study does not significantly impact glenoid-to-footprint distances but does alter the location of the contact, which occurred in most participants.
Rotator cuff pathology is a common finding in patients with shoulder pain.1,2 Although the etiology of rotator cuff pathology is likely complex and multifactorial, it is generally believed that repeated tendon deformation (i.e., mechanical impingement) during shoulder motion contributes to degenerative tears.3,4 One form of tendon impingement – internal impingement – occurs when the undersurface of the rotator cuff is entrapped against the superior glenoid.5,6 It was originally identified in overhead athletes when the shoulder is placed in a combination of abduction and external rotation.5 However, recent evidence suggests that internal impingement may also occur during more functional arm raising tasks.7-10 Diverse study methodologies including in vivo assessment,7,10 modeling,8 and arthroscopic evaluation,9 all show the distance between the glenoid and the supraspinatus tendon insertion (i.e., footprint) to steadily decrease during humeral elevation. Furthermore, contact between the glenoid and rotator cuff footprint may be prevalent.8-10 Taken together, this evidence suggests that internal impingement may be a mechanism of rotator cuff injury in non-athletic populations.
When a potential mechanism of injury has been identified, it is important to understand the extent to which movement factors may impact the mechanism so that more targeted prevention and rehabilitation strategies can be developed.11 For example, Saini et al.8 hypothesized that decreased scapulothoracic upward rotation (UR) may increase the incidence of contact between the glenoid and rotator cuff footprint as it would presumably orient the superior glenoid rim downwards and closer to the rotator cuff tendon insertion (i.e., footprint). If decreased scapulothoracic UR does indeed increase the incidence of glenoid-to-footprint contact and internal impingement is suspected to be underlying the patient's symptoms, then it may be prudent to focus rehabilitation on increasing scapulothoracic UR. However, the impact of decreased scapulothoracic UR on internal impingement remains unknown. Therefore, the purpose of this study was to compare the distance between the glenoid and rotator cuff footprint between two groups classified based on scapulothoracic UR magnitude (i.e., low, high) at 90° humerothoracic elevation. It was hypothesized that the low scapulothoracic UR group would have smaller glenoid-to-footprint minimum distances.
MethodsParticipantsSixty participants were recruited for this study (33 (8) years, 53% female, 50% asymptomatic). Eligible participants were aged 21–60 years without a history of shoulder surgery, fracture, dislocation, separation, inflammatory joint disease, or contraindications to MRI or radiation exposure. Individuals with shoulder pain were included if they had anterolateral shoulder pain provoked by shoulder motion for at least 4 weeks, and were excluded if they could not raise their symptomatic shoulder ≥120° humerothoracic elevation and if they had radiating pain or paresthesias in the involved arm, symptom onset following trauma, >25% reduction in range of motion compared to the contralateral side, and symptom reproduction during cervical spine screening.12 All participants provided informed written consent prior to participation. The study was approved by the University of Minnesota's Institutional Review Board.
Data collectionShoulder kinematics were acquired using a BV Pulsera C-arm (Philips; Amsterdam, NL) synchronized to a five-camera motion-capture system (Vicon; Oxford Metrics, Yarnton, UK) using MotionMonitor software (Innovative Sports Training, Inc., Chicago, IL) as previously described.13,14 Participants were seated, a reflective marker cluster was secured to their thorax, and torso anatomical landmarks were digitized.15 Fluoroscopic images were acquired at 25 Hz while the participants performed dynamic, unloaded scapular plane abduction. Finally, an MRI was acquired of the entire scapula and proximal humerus using a 3T scanner (MAGNETOM Prisma; Siemens AG, Munich, Germany).16
Data processingThree-dimensional bone models of the humerus and scapula were reconstructed from the MRI scans using Mimics software (materialise NV, Leuven, Belgium). Anatomical coordinate systems were defined on the humerus17 and scapula18 to describe glenohumeral kinematics and, when related to the thorax, humerothoracic and scapulothoracic kinematics. A glenoid-based coordinate system was also defined for the scapula to facilitate the interpretation of glenohumeral position and proximity center locations (described below).19
Fluoroscopic image calibration and distortion correction were performed using XMALab,20 and kinematic tracking was performed using JointTrack software.21 The tracking accuracy of this protocol has been previously established (RMS errors: 0.7–3.3°, 1.2–4.2 mm).14 Glenohumeral, scapulothoracic, and humerothoracic kinematics were described using X-Z’-Y’’, Y-X’-Z’’, and Y-X’-Y’’ rotation sequences, respectively.15,22 Glenohumeral anterior/posterior and superior/inferior positions were described using the glenoid-based coordinate system and were normalized to glenoid width and height, respectively, to facilitate interpretation.23 Left-sided data were transformed to right-sided equivalence.
Participants were classified into scapulothoracic UR groups based on their magnitude of UR at 90° humerothoracic elevation during the motion trial. This angle was chosen for classification as it corresponds to the lower-bound range during which the supraspinatus tendon approachs the glenoid8 and is an angle that can be readily assessed clinically. In the absence of normative data from which to classify the participants, participants were classified as follows: the 20 participants with the highest scapulothoracic UR were assigned to the high UR group, the 20 participants with the lowest scapulothoracic UR were assigned to the low UR group, and the remaining participants were assigned to the mid UR group.13
Each participant's dynamic trial was reconstructed by animating their humeral and scapular bone models with their corresponding glenohumeral kinematics using a custom MATLAB code (The MathWorks, Inc, Natick, MA). This code also calculated distance maps for the glenoid and rotator cuff footprint at 10° increments of humerothoracic elevation (Supplementary Material 1 - Fig. S1A). The rotator cuff footprint was defined as the superior and inferior facets on the greater tuberosity, accounting for the supraspinatus and infraspinatus tendon insertions.24 During minimum distance calculations, a constraint was included to prevent the minimum distance vector from penetrating either surface, which often happened at lower elevation angles (Supplementary Material 1 - Fig. S1B), thereby ensuring that all minimum distances were physiologically plausible.
From these distance maps, the following proximity measures were calculated. First, the minimum distance was calculated as the smallest distance between the glenoid and rotator cuff footprint (i.e., glenoid-to-footprint minimum distance) (Supplementary Material 1 - Fig. S1A). Second, the location of the minimum distance (i.e., proximity center) was identified on each surface and were described relative to the glenoid-based and humeral coordinate systems, as appropriate. To facilitate interpretation, glenoid proximity centers were subsequently normalized to glenoid height or width (as appropriate), and humeral proximity centers were normalized to the diameter of a sphere fit to the humeral articular surface. Third, contact between the glenoid and footprint was defined to occur when the glenoid-to-footprint minimum distance was ≤4.3 mm, which represented the average thickness of the posterosuperior glenoid labrum.10,25 When glenoid-to-footprint contact occurred, the humerothoracic angle at which the glenoid-to-footprint minimum distance first fell below the estimate labral thickness was documented (i.e., angle of initial contact), along with the 3D distance between the biceps groove and footprint's proximity center.26,27
Statistical analysisTo help ensure a clinically meaningful difference between groups in scapulothoracic UR, only data for the low and high UR groups were included in the statistical analysis. Demographic data were compared between groups using independent t-tests or chi-square tests, as appropriate. Differences between UR groups in kinematics, glenoid-to-footprint minimum distance, and proximity center locations were assessed across humerothoracic elevation angles using two-factor mixed-model ANOVAs (groups: low, high; angles: 100°, 120°, 140°). These elevation angles were chosen because they coincide with when the supraspinatus tendon approximates the glenoid8 and because higher angles were not achieved by many participants. Tukey-Kramer adjustments were used to protect against alpha inflation. The prevalence of contact and the humerothoracic elevation angle at initial contact was compared between groups using chi-square and two-sample independent t-tests, respectively. Finally, a sensitivity analysis was performed to investigate the extent to which the humerothoracic elevation angle at which groups were classified (i.e., 90°) influenced the results (Supplementary Material 1). Statistical analysis was performed in SAS Version 9.4 (SAS Institute Inc, Cary, NC) using a type I error rate of <0.05.
ResultsDemographicsParticipant demographic data are presented in Table 1. There were no significant differences between scapulothoracic UR groups in any demographic variable.
Participant demographics by scapulothoracic upward rotation group. Data are presented as mean (SD) unless otherwise indicated.
Groups were classified as having high or low UR based on their ST UR magnitude at 90° HT elevation. Groups were compared using independent 2-sample t-tests or chi-square tests, as appropriate. Confidence intervals are calculated as high UR minus low UR group. Abbreviations: CI, confidence interval; HT, humerothoracic; NA, not applicable; ST, scapulothoracic; UR, upward rotation.
Participants achieved an average humerothoracic elevation angle of 152.4° (8.4°) without a significant difference between UR groups (95% CI: −1.3°, 9.3°, p=0.13) (Table 1). However, 7 participants were not able to achieve 140° humerothoracic elevation (Table 2).
Comparison of the prevalence of contact between the glenoid and rotator cuff footprint. Overall prevalence indicates that contact occurred at any time during the motion trial (i.e., including contact that occurred above 140° humerothoracic elevation).
Note that the sample size decreases in both groups at 140° humerothoracic elevation as not all participants achieved the angle during the motion trial. Data are presented as frequency (prevalence).
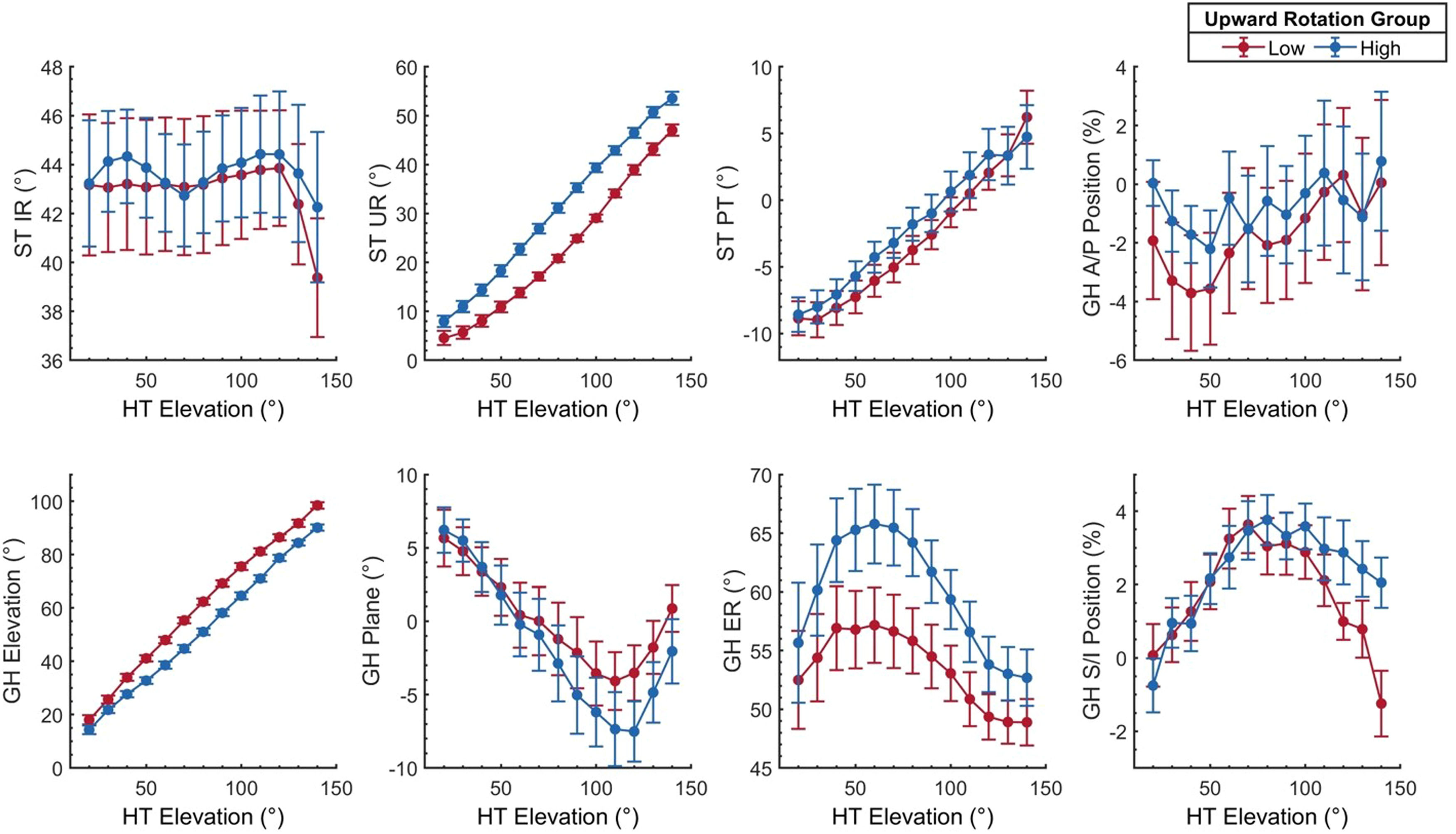
Consistent with the group classification, individuals in the low UR group were in an average of 10.4° less scapulothoracic UR at 90° humerothoracic elevation (i.e., the angle at which participants were classified) compared to those in the high UR group (95% CI: 8.1°, 12.7°, p<0.01). This group difference decreased as humeral elevation angles increased but remained statistically significant (interaction: p<0.01, all pairwise comparisons: p<0.01; mean differences at 100°, 120°, and 140° humerothoracic elevation: 10.3°, 7.6°, and 5.3°) (Fig. 1). Groups were not statistically different in scapulothoracic internal rotation (interaction: p=0.33; group main effect: p=0.74) or tilt (interaction: p=0.07; group main effect: p=0.77).
Scapulothoracic (A) and glenohumeral (B) kinematics for the high and low scapulothoracic upward rotation groups plotted over the humerothoracic elevation range of motion. Glenohumeral anterior/posterior and superior/inferior position represents the humeral head center relative to the glenoid coordinate system and is normalized as a percentage of glenoid width and height, respectively. Data are presented descriptively as mean and unpooled standard error. Scapulothoracic upward rotation and glenohumeral elevation and external rotation are transformed to positive values to facilitate interpretation. Groups were compared statistically at 100°, 120°, and 140° humerothoracic elevation. Abbreviations: A/P, anterior/posterior, DR, downward rotation; ER, external rotation; GH, glenohumeral; HT, humerothoracic; IR, internal rotation; PT, posterior tilt; ST, scapulothoracic; S/I, superior/inferior; UR, upward rotation.
Although groups were classified based on scapulothoracic UR, group differences were also observed in glenohumeral kinematics (Fig. 1). Specifically, individuals in the low UR group were in an average of 7.1°−11.0° more glenohumeral elevation between 100°−140° humerothoracic elevation compared to those in the high UR group (interaction: p<0.01) (Fig. 1). Furthermore, between 100°−140° humerothoracic elevation, the humerus was positioned an average of 1.9% more inferior on the glenoid in individuals in the low UR group compared to those in the high UR group (95% CI: 0.2%, 3.5%; group main effect: p=0.04). No significant group differences existed for glenohumeral plane of elevation (interaction: p=0.41; group main effect: p=0.24), axial rotation (interaction: p=0.41; group main effect: p=0.13), or anterior/posterior position (interaction: p=0.59; group main effect: p=1.00).
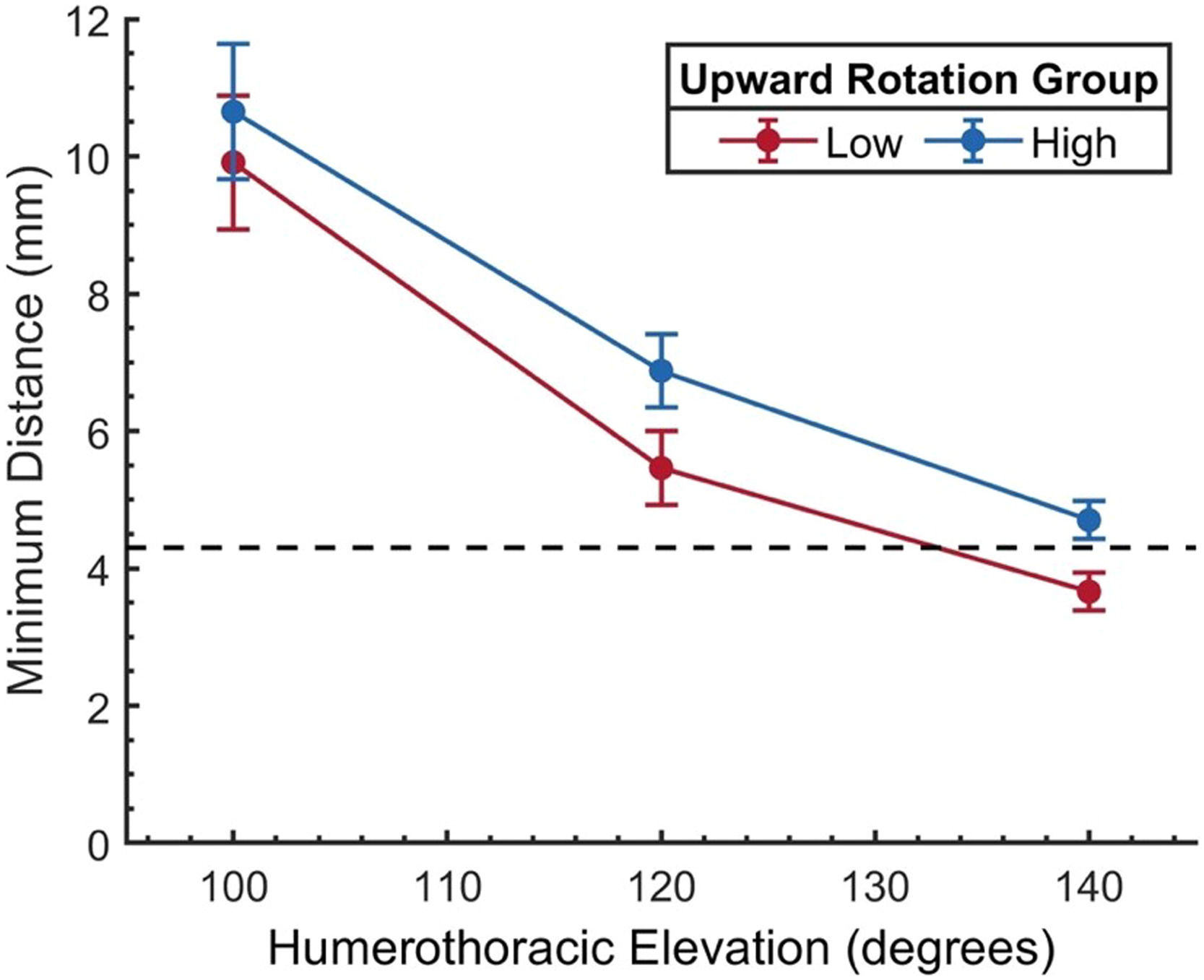
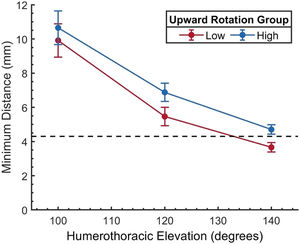
Distance between the glenoid and rotator cuff footprintThe glenoid-to-footprint minimum distance decreased consistently in all participants as the humerothoracic angle increased (angle main effect: p<0.01). Although the footprint tended to be closer to the glenoid in individuals in the low UR group, the effect was not statistically significant (95% CI: −0.4, 2.5 mm; group main effect: p=0.16; interaction: p=0.50) (Fig. 2).
The minimum distance between the glenoid and rotator cuff footprint for the high and low scapulothoracic upward rotation groups. Data are presented as mean and standard error. The glenoid-to-footprint minimum distance decreased consistently in all participants as the humerothoracic angle increased (angle main effect: p<0.01). Although the footprint tended to be closer to the glenoid in individuals in the low UR group, the effect was not statistically significant (group main effect: p = 0.16, group-by-angle interaction: p = 0.50). The dashed line represents the estimated labral thickness (4.3 mm).25
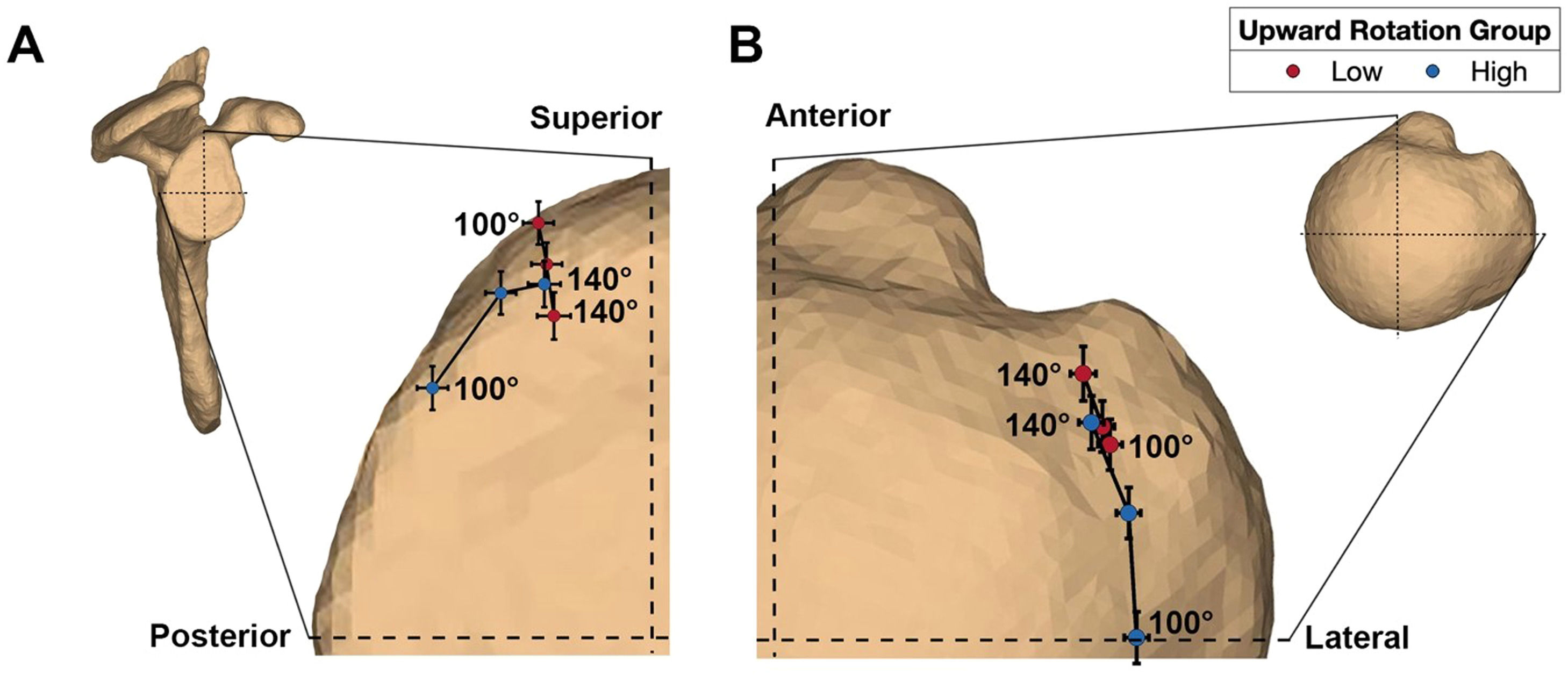
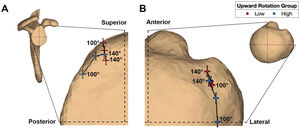
Between 100–140° humerothoracic elevation, the anterior aspect of the rotator cuff footprint was generally proximate with the posterior/superior aspect of the glenoid (Fig. 3). Group differences in the glenoid's anterior/posterior proximity center location depended on the humerothoracic elevation angle (interaction: p<0.01). At 100° humerothoracic elevation, the proximity center was located 16.4% more posterior in the high UR group compared to the low UR group (95% CI: 9.8%, 23.0%, p<0.01). However, this group difference was no longer significant at 120° or 140° humerothoracic elevation (p≥0.29). Group differences in the glenoid's superior/inferior proximity center location also depended on the humerothoracic elevation angle (interaction: p<0.01). At 100° humerothoracic elevation, the proximity center was located 19.3% more inferior in the high UR group compared to the low UR group (95% CI: 12.2%, 26.3%, p<0.01). However, this group difference was no longer significant at 120° or 140° humerothoracic elevation (p≥0.93).
Average contact center location on the A) glenoid (lateral view), and B) humeral rotator cuff footprint (superior view). The proximity paths are labeled to indicate the first (100°) and last (140°) humerothoracic elevation angle assessed statistically. Between 100–140° humerothoracic elevation, the anterior aspect of the rotator cuff footprint was generally proximate with the posterior/superior aspect of the glenoid. Differences between groups existed in the anterior/posterior and superior/inferior location of the proximity center on the glenoid and the anterior/posterior location of the proximity center on the rotator cuff footprint.
Group differences also existed for the proximity center location on the rotator cuff footprint. The footprint's anterior/posterior proximity center location shifted anteriorly in both groups between 100°−140° humerothoracic elevation but shifted significantly more in the high UR group (interaction: p<0.01). Specifically, at 100° humerothoracic elevation, the proximity center in the high UR group was located 19.5% more posterior than the low UR group (95% CI: 12.3%, 26.6%, p<0.01). However, this group difference was no longer significant at 120° or 140° humerothoracic elevation (p≥0.17). Finally, there were no significant group differences in the medial/lateral proximity center location (interaction: p=0.43; group main effect: p=0.18).
Contact between the glenoid and rotator cuff footprintThe minimum distance fell below the estimated labrum thickness (suggesting glenoid-to-footprint contact) in 75.0% of participants (Table 2) and did so at an average humerothoracic elevation angle of 133.6° (95% CI: 127.3°, 139.9°, min: 89.7°, max: 164.9°). This angle of initial contact was an average of 20.4° lower than the participants’ maximum humerothoracic elevation angle without any difference between groups (95% CI: 17.2°, 23.5°, p=0.77). There were no significant group differences in the overall prevalence of contact between scapulothoracic UR groups (p=0.47; low UR: 80%, high UR: 70%) or the humerothoracic elevation angle at which contact initially occurred (p=0.33; low UR: 130.7°, high UR: 137.0°, 95% CI: 6.8°, 19.5°). Furthermore, there was no significant difference in the prevalence of contact between symptom groups (p=0.58; asymptomatic: 79.0%, symptomatic: 71.4%). In individuals with contact, the proximity center on the footprint at initial contact occurred an average of 11.7 (0.5) mm posterior to the biceps groove.
DiscussionThis study investigated the kinematic mechanisms of rotator cuff internal impingement by calculating the distance between the glenoid and rotator cuff footprint during scapular plane abduction and comparing this distance between groups classified based on scapulothoracic UR. In all participants, the glenoid-to-footprint distance steadily decreased during the motion trial and in 75%, the distance fell below the estimated labral thickness, suggesting glenoid-to-footprint contact. Moreover, contact typically occurred at an average of 133.6° (3.2°) humerothoracic elevation, which was an average of 20° below the maximum humerothoracic elevation. This finding suggests that contact occurs well-within available range of motion, is consistent with previous investigations,8-10 and provides further evidence that internal impingement could be a more prevalent mechanism of rotator cuff injury or symptom provocation than what is currently believed. Unfortunately, the angle at which pain was provoked during the motion trial in symptomatic participants was not recorded, which would have allowed for correlation with symptoms. However, the high prevalence of pain in symptomatic individuals in overhead elevation angles28 suggests it may be prudent for clinicians to carefully consider how to counsel patients regarding how much pain to tolerate if internal impingement is suspected (e.g., whether to “push through” pain).
Although glenoid-to-footprint minimum distances decreased consistently in all participants, individuals in the low UR group tended to have smaller distances than those in the high UR group (Fig. 2) and made contact at a lower humerothoracic elevation angle. However, these effects did not achieve statistical significance despite modest mean differences due to high between-subject variability. One factor that likely contributed to the inconclusive findings of the current study was the manner in which groups were classified. For example, the angle at which participants were classified (i.e., 90° humerothoracic elevation) is arguably subjective; however, the results of the sensitivity analysis suggest that classifying participants based on other relevant humerothoracic elevation angles (i.e., 100°, 110°, 120°) would not have substantially altered the results of the study (Supplementary Material 1). This is likely because over 65% of participants remained in the same group classification regardless of the angle. Additionally, we chose to investigate glenoid-to-footprint distances and contact centers between 100°−140° humerothoracic elevation as it coincides with when the supraspinatus tendon approximates the glenoid.8 However, the statistical effect may have been underestimated by including the 100° angle, when glenoid-to-footprint distances remained large and variable between participants.
But perhaps a more important consideration when interpreting the inconclusive findings is that the analysis was likely confounded by attempting to assess the effect of a single kinematic variable (i.e., UR) within the complex three-dimensional, multi-joint system of the shoulder girdle. For example, group differences in glenohumeral kinematics were also observed despite being classified based on scapulothoracic kinematics. Specifically, individuals in the low UR moved more inferiorly on the glenoid and tended to have decreased glenohumeral external rotation (Fig. 1). Therefore, it is possible the effect of decreased UR was offset by the effect of other kinematic variables and by the influence of anatomical morphology (e.g., glenoid version, inclination, footprint shape). Herein lies a major challenge when assessing the effect of a single movement variable within a complex system, and why dismissing the importance of UR based on the results of this study may be premature. Instead, it may be beneficial in future studies to first investigate the effect of a single movement variable on mechanisms of rotator cuff pathology so that confounding variables can be controlled. Once those effects are elucidated, then the investigation can be broadened to determine how these effects manifest within the more complex in vivo movement system. Finally, translational studies would be needed to develop and validate techniques to identify and quantify relevant movement patterns within a clinical environment.
Another approach to investigating the impact of movement impairments on mechanisms of rotator cuff pathology may be to adopt another method of classification entirely. The ideal movement-based classification system identifies impairments that presumably contribute to or result from a patient's pain or dysfunction,29 which may be better suited when classification is performed within an individual using movement modification tests (e.g., scapular assistance test)30,31 instead of by interpreting kinematics based on normative or distributive values. For example, the current study classified individuals as “low” or “high” UR based on the magnitude of UR at 90° humerothoracic elevation, and it is possible that individuals in the low UR group had other kinematic or anatomical factors (e.g., high glenoid inclination) that allowed the low UR to be sufficient, even if it was considered “low” across the study's sample. In other words, it is possible that the objective magnitude of UR is not as important to a movement-based classification as the effect of modifying the movement on the patient's symptoms. Future research attempting to elucidate the effect of movement impairments on mechanisms of pathology may benefit from a within-subject classification as it may be more consistent with the goals of a movement-based classification system, and thus has a higher potential for clinical translation.
Although glenoid-to-footprint minimum distances were not significantly different between scapulothoracic UR groups, differences were observed in the proximity center location on the glenoid and footprint surfaces. Between 100–140° humerothoracic elevation, the proximity center remained more centralized within the anterior footprint and posterosuperior glenoid in individuals with low UR compared to those with high UR (Fig. 3). The consistent localization is an interesting finding. Presumably, a larger distribution of contact would help distribute the stress within the tissue, which may help prevent (or delay) any associated tissue microtrauma. However, this supposition is highly speculative in the absence of measures of tendon deformation and longitudinal analyses. In all participants, the proximity center was located an average of 11.7 mm posterior to the biceps groove at initial contact, which corresponds to the region where tears are thought to originate,26,27 and may help to explain the occurrence of undersurface tears.1,2,5,32,33 While these findings may suggest that internal impingement is a potential mechanism for degenerative rotator cuff tears, causation cannot be inferred from the results of this study. Future work that aims to longitudinally assess kinematics and proximity center locations in combination with diagnostic imaging may help clarify the role of internal impingement in rotator cuff pathology.
The findings that glenoid-to-footprint contact was observed in most participants without a significant difference between individuals with and without shoulder pain raises the question of whether internal impingement is pathological. However, several factors preclude the ability of this study to address the question including the study's cross-sectional nature, relatively young sample, and lack of diagnostic imaging. Furthermore, other factors that may contribute to rotator cuff tendon degeneration were not assessed (e.g., genetics,34 comorbidities,26,35 exposure36,37). Consequently, it is possible that contact between the rotator cuff and glenoid itself is not outright pathological, but the consequences likely depend on the frequency and nature of contact, and the ability of the tissues to withstand the associated stresses.38 More research is needed to understand how a combination of these factors (and others) may contribute to the etiology of rotator cuff pathology.
The following limitations need to be considered when interpreting the results of this study. First, single-plane fluoroscopy likely resulted in out-of-plane kinematic tracking errors.14 However, kinematic tracking was performed blinded; therefore, errors are not expected to influence group comparisons. Second, the relatively small and young sample may limit the generalizability of the results. Third, 7 participants did not achieve 140° humerothoracic elevation during the motion trial. It is possible that the seated posture may have limited range of motion; however, the average maximum elevation angle in this group (152.4°) agrees with studies using similar methodologies.10 Fourth, this study calculated bone-to-bone distances to investigate a potential mechanism of soft tissue pathology, and it is likely that the measure is an oversimplification of a complex phenomenon. More complex methodologies (e.g., finite element analysis) are likely necessary to better elucidate the role of internal impingement in rotator cuff pathology. Fifth, an average labral thickness was used to estimate the incidence of glenoid-to-footprint contact given the labrum was not well-visualized in the MRI images. However, a prior sensitivity analysis suggests that the estimated thickness did not significantly alter the prevalence of contact.10 Ultimately, our understanding of potential mechanisms of rotator cuff injury would benefit from methodology that can simultaneously account for soft tissue deformation, kinematics, and morphology.
ConclusionThe results of this study suggest that groups classified based on scapulothoracic UR at 90° humerothoracic elevation exhibit differences in the glenoid-to-footprint proximity center location, but not in the magnitude of the minimum distance when considered between 100 and 140° humerothoracic elevation. However, the effect of UR on glenoid-to-footprint distances may be confounded by concurrent group differences in glenohumeral kinematics. Glenoid-to-footprint contact was identified in most participants and well-within their humeral elevation range of motion. Taken together, these findings provide further evidence that glenoid-to-footprint contact likely occurs during functional overhead motions and could therefore be a more prevalent mechanism of rotator cuff injury than what is currently believed.
This work was supported the National Institutes of Health (F31-HD087069, F31-AR079259, T32-AR050938, UL1-TR002494, P41-EB015894), Foundation for Physical Therapy, Minnesota Partnership for Biotechnology and Medical Genomics, a research infrastructure grant from the University of Minnesota Office of the Vice President for Research, and the University of Minnesota Department of Orthopaedic Surgery and Clinical and Translational Science Institute. Neither the NIH nor any of the other funders played a role in the design, conduct, or reporting of this study.