Foot deformities are highly prevalent in older adults and negatively impact their mobility and quality of life. However, the association between foot problems and physical function is still unclear.
ObjectiveTo investigate whether structural foot deformities and plantar tactile sensitivity are associated with lower extremity physical function impairment in community-dwelling older adults.
MethodsWe included 200 men and women aged 60 years and older from a community-based program. The foot assessment included toe deformities and calluses inspection and evaluation of plantar tactile sensitivity using monofilaments. The Short Physical Performance Battery (SPPB) was used to assess lower extremity physical function. We conducted a multivariate logistic regression analysis to investigate the association between foot problems and lower extremity physical function.
ResultsHallux valgus was the most prevalent deformity among older adults. Those participants with reduced plantar tactile sensitivity (OR= 2.77; 95% CI: 1.38, 5.55) and a hallux valgus (OR= 2.23; 95% CI: 1.10, 4.52) were more likely to present poor lower extremity physical function.
ConclusionHallux valgus and impaired plantar sensitivity were associated with reduced lower extremity physical function in older adults. Further studies are necessary to identify this causality and to what extent management of these foot problems can improve general mobility and quality of life of older adults.
Foot problems are highly prevalent with advancing age,1-3 and 50% to 80% of community-dwelling older adults present at least one structural, cutaneous, toenail foot condition, or foot pain.3-5 Foot disorders related to aging include reduced plantar tactile sensitivity, hyperkeratosis, and musculoskeletal foot disorders, such as hallux valgus, lesser digits deformities, pes planus, or cavus.2,3,6-10 Hallux valgus is the most common deformity observed in older people,4 and is characterized by lateralization of the first digit and medial deviation of the first metatarsal.3 Overall, these foot disorders are associated with decreased strength of the intrinsic foot muscles, which negatively impact balance control2 and gait speed,11,12 ultimately increasing the risk of single and recurrent falls in older individuals.2,12-15
Somatosensory information from the sole of the feet also plays an important role in balance control and functional mobility in daily activities (e.g., stepping or walking on uneven surfaces).16-20 Plantar tactile sensitivity decreases with aging, especially under the forefoot region, due to the reduced number and density of tactile receptors and myelinated peripheral nerve fibers.21-23 Therefore, it would be plausible to consider the importance of evaluating plantar tactile sensitivity8,13,15 and foot structural problems in clinical practice due to its possible implication to functional mobility among older people.14 However, the impact of foot problems on the physical function of older adults is still debated. While some studies suggest that reduction in plantar tactile sensitivity12,24 and structural foot disorders12 may be associated with limitations in physical functional of older people12,18,24 other studies did not find an association between physical function and hallux valgus4 or with plantar sensitivity.25
The association between lower extremity physical function and foot problems (hallux valgus and plantar tactile sensitivity impairment) using an overarching instrument such as the Short Physical Performance Battery (SPPB) that captures stability in a standing position, gait speed, and strength has not been investigated yet. Furthermore, hallux valgus, which is highly prevalent7,26 particularly among women over 65 years6,9,27 is commonly considered a natural consequence of aging2,12 and often neglected in older adults assessment. The improper evaluation of foot problems, particularly hallux valgus, may be critical for older adults' mobility3,11,18,28 and identifying those at a high risk of falling.2,12-15
In the present study, we aimed to investigate whether foot problems are associated with lower extremity physical function in community-dwelling older adults. We addressed foot problems among women and men, whether foot sensitivity impairment is associated with age and differences in SPPB score for individuals with and without foot problems. We hypothesized that decreased plantar tactile sensitivity and hallux valgus would be associated with reduced physical function. An association between foot problems and lower extremity physical function would suggest that the management of foot problems is an important component of mobility in this population.
MethodsParticipantsThis cross-sectional study included 200 men and women aged 60 years or older who lived in the geographical area of a community-based primary health care program (called Family Health Strategy, FHS) linked with the Basic Health Care Center (Unidade Básica de Saúde, UBS), in Novo Juazeiro neighborhood, Ceará, Brazil. We invited older adults to participate using the UBS list, and those who accepted to participate were visited at home. We excluded individuals if they: i) presented cognitive decline as determined by the Mini-Mental State Examination (MMSE),29 adjusted for education level (i.e., participants who are illiterate, have 1–7 years of education, or have ≥ 8 years of education were considered having a cognitive decline if their MMSE score was ≥ 13, ≥ 18, and ≥ 26 points, respectively); ii) self-reported diabetes and neurological disorders (e.g., peripheral neuropathy, stroke, and Parkinson's disease); iii) presented severe venous insufficiency or skin or venous ulcers at the foot sole observed by visual inspection; iv) reported regular use of alcohol; v) had severe communication problems (i.e. hearing loss, visual impairment) and were unable to walk even with the use of an assistive device. We determined the presence of diabetes by asking the participants about medications used to control diabetes and the presence of peripheral neuropathy by inquiring participants about numbness and neuropathic pain.
The study was approved by the Ethics Committee of the Universidade Cidade de São Paulo (UNICID), São Paulo, Brazil (protocol number: 16109013.2.0000.0064) and was conducted according to the principles of the Declaration of Helsinki. All participants provided written, informed consent to participate in the study.
ProceduresSociodemographic assessment included age, sex, education level, and monthly income. We identified comorbidities using the Functional Comorbidity Index.30 The participants were also asked about number of medications used regularly, number of falls in the last 12 months, and physical activity level was assessed using the Incidental and Planned Exercise Questionnaire (IPEQ) version W.31 The 12-item questionnaire of the World Health Organization Disability Assessment Schedule (WHODAS) 2.0 was used to evaluate health and disability.32 This version of the questionnaire is divided into six domains: cognition, mobility, self-care, getting along with other people, life activities (household and work), and community participation.33 Each item was scored based on a 0–4 scale, where 0=none, 1=mild, 2=moderate, 3=severe, and 4=extreme, and the final is the sum of the 12 items. Thus, the total score, which indicates the degree of functional limitation, could range from 0 to 48 points. A higher score indicates higher disability. The total score was classified using the 20th percentile. Participants above the 20th percentile were considered to have severe disability.
Foot structural problemsWe assessed the presence of structural foot problems by visual inspection. A checklist34,35 was used to classify the problems considering the following items: foot pain (as dichotomic answer "yes" or "not"); hallux valgus severity ranging between 0 to 3, where zero was considered absence of deformity and three most severe deformity. The metatarsal and phalanx deformities and plantar regions were classified by skin thickness, callosity, or joint deformities.
Plantar tactile sensitivity evaluationWe assessed the plantar tactile sensitivity using the Semmes-Weinstein monofilament on the right foot while the participant was seated with their right leg lying on a cushioned stool. A screen (length 60 cm × width 35 cm) was placed in front of the participant's eyes to prevent their use of visual cues. The screen bore a colored photo (length 30 cm × width 22 cm) of a foot sole, and then the participant could indicate the site of the plantar foot that they perceived the touch of the monofilament. We used the photo to avoid any possible problems that the participants might have in naming the various foot sites (Fig. 1).
The foot sites sensitivity was assessed by placing the 4g aesthesiometer (SORRI®) on five plantar foot locations (Fig. 1).8 When the foot had calluses at these regions, we chose a nearby-uncallused area. The aesthesiometer was applied perpendicular to the foot surface for 1–2 seconds until the monofilament bent into a C-shape. The monofilament was held at this position for about 1 second before being withdrawn. We considered an invalid trial if the monofilament slipped during the procedure. In this case, another trial was performed.
The sequence of sites was randomized. We instructed the participants to answer "yes, I did" if they felt the touch and "no, I did not" if they did not feel.36 Each monofilament was applied three times at intervals of 5 seconds on the same site. The foot site sensitivity was considered normal if the participant felt touch sensation over the respective site at least two of the trials.36 We did not inform participants whether they identified the monofilament correctly. We classified the plantar tactile sensitivity as not impaired if the participant perceived the sensation under all the plantar sites and impaired sensitivity if the perception was absent in one or more plantar site.
Physical function assessmentThe SPPB was used to assess lower extremity physical function37 and consists of three tests: balance stability in a standing position, usual gait speed, and the strength in the lower limbs, as determined by the chair stand test. Each category score ranged from 0 (worst performance) to 4 points (best performance), with a maximum score of 12 points.37,38 A cutoff of ≤ 7 points was used to identify impairment of the lower extremity physical function.39,40
All assessments were performed by the same evaluator.
Statistical analysesThe Kolmogorov-Smirnov test was used to verify the normality of the data. Due to the non-normal distribution, the descriptive analysis was done using median, interquartile ranges values, and frequencies except for age, clinical and physical activity data. We conducted the univariate logistic regression analysis to investigate the association between foot structural problems (hallux valgus, toes deformities), plantar tactile sensitivity, presence of digital calluses and corns, feet pain, and the lower extremity physical function (SPPB score with a cutoff point of ≤ 7 points).40 Two multivariate logistic regression models were conducted: 1) Model 1 tested the association between foot problems (hallux valgus, impairment in tactile sensitivity of the foot, digit calluses, and corns) and lower extremity physical function (SPPB) using a univariate analysis; 2) Model 2 examined the association between variables, considering those from Model 1 with a p< 0.05, and physical function of the lower limb (SPPB), and this model was adjusted by the following confounders: female sex, number of comorbidities (Functional Morbidity Index), history of falls, depression, obesity (body mass index [BMI] ≥ 30 kg/m2), and low back pain. We reported odds ratios with lower and upper 95% confidence intervals (95% CIs) and p-values. The fit of the multiple logistic regression models was evaluated using the Hosmer-Lemeshow goodness-of-fit test. The Fisher's exact test was used to verify plantar sensitivity and foot problems among men and women. We used point-biserial correlation to verify the association between age and impaired tactile sensitivity of the foot (0 and 1 or more sites) for men and women. The Mann-Whitney U tested differences in the SPPB sub-domains scores (balance, gait speed, and strength of the lower limbs), between individuals with and without impaired foot sensitivity or foot problems. Statistical analyses were performed using the software SPSS (version 19.0, SPSS Inc., Chicago, IL), all tests were two-tailed, and a significance level was set at α<0.05.
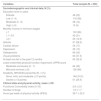
ResultsTwo hundred and sixty-nine participants living in the family health strategy program's catchment geographical area were enrolled. Fifty-four were excluded, and 15 refused to participate in the study. Reasons for exclusion were: severe hearing problems (n=3), diabetes (n=29), stroke (n=4), alcohol consumption (n=2), Alzheimer's disease (n=7), and cognitive decline measured by MMSE (n= 9). Of the 200 participants included, the participants' mean ± standard deviation age was 69.8 ± 6.6 (range, 60–94) years. The mean age for men was 69.8 ± 6.8 and for women was 69.8 ± 6.5. One hundred and sixty-two (81%) participants were illiterate or had a low educational level (1-4 years of schooling). Table 1 shows the demographic and clinical characteristics of the sample. The mean ± standard deviation of Functional Comorbidity Index of the participants was 2.8 ± 2.0.
Characteristics of the participants (n= 200).
Abbreviations: IPEQ, Incidental and Planned Exercise Questionnaire; SPPB, Short Physical Performance Battery; WHODAS, World Health Organization Disability Assessment Schedule.
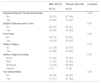
We first performed a univariate regression analysis to determine the association between foot impairments and SPPB score. In this analysis, we verified that impaired plantar tactile sensitivity (OR= 2.55; 95% CI: 1.34, 4.84), hallux valgus (OR=2.16; 95% CI: 1.11, 4.19), and digital calluses and corns (OR=1.94; 95% CI: 1.05, 3.58) were significantly associated with reduced lower extremity physical function (SPPB ≤ 7 points). Therefore, we included only these variables in the multivariate regression analysis as predictors. The multivariate analysis revealed that plantar tactile sensitivity and hallux valgus were independently and significantly associated with the SPPB in Model 2 (Table 2). Although digital calluses and corns were associated with SPPB on univariate analysis, this foot impairment did not enter the final model as a predictor for lower extremity physical function impairment.
Univariate and multivariate logistic regression models for the association between poor lower extremity functionality (SPPB≤ 7 points) and foot problems amongst community-dwelling older adults from a community-based health program (n=200).
Adjusted by: female sex, the number of comorbidities (Functional Morbidity Index), history of falls, depression, BMI ≥ 30 kg/m2, low back pain. Hosmer and Lemeshow test - Model 2 (p=0.249).
Table 3 describes foot problems by sex. The most common structural foot problem found among participants was hallux valgus, followed by toes deformities, digital calluses, and corns. The prevalence of foot problems was similar between men and women, except for the plantar sensitivity of the foot.
Foot problems according to sex amongst community-dwelling older adults from a community-based health program (n=200).
| Men (N=61) | Women (N=139) | p-values | |
|---|---|---|---|
| N (%) | N (%) | ||
| Impaired Plantar Tactile Sensitivity | 0.03* | ||
| No | 19 (31) | 67 (48) | |
| Yes | 42 (69) | 72 (52) | |
| Digital Calluses and Corns | 0.91 | ||
| No | 29 (47) | 65 (47) | |
| Yes | 32 (53) | 74 (53) | |
| Foot Pain | 0.24 | ||
| No | 46 (75) | 93 (67) | |
| Yes | 15 (25) | 46 (33) | |
| Hallux Valgus | 0.75 | ||
| No | 21 (34) | 52 (37) | |
| Yes | 40 (66) | 87 (63) | |
| Hallux Valgus severity | 0.87 | ||
| None | 21 (34) | 52 (37) | |
| Mild | 21 (34) | 40 (29) | |
| Moderate | 15 (25) | 36 (26) | |
| Severe | 4 (7) | 11 (8) | |
| Toe Deformities | 0.05 | ||
| No | 30 (49) | 48 (34) | |
| Yes | 31 (51) | 91 (66) |
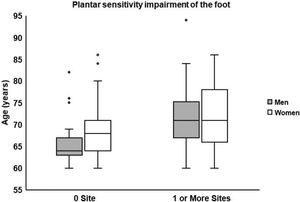
Fig. 2 shows the impairment sensitivity (0 and 1 or more sites) according to age for men and women. The point-biserial correlation revealed association between age and impaired tactile sensitivity of the foot for men (rpb = 0.37; p = 0.003) and women (rpb = 0.26; p = 0.002).
We found significant differences in the median score of SPPB subdomains between older adults with and without foot problems. Older adults with impaired tactile sensitivity presented lower median scores for gait speed and lower-limb strength than participants without sensitivity impairment (gait speed median scores 3 and 4, respectively; p = 0.03; lower-limb strength median scores 1 and 2, respectively; p = 0.008). Older adults with hallux valgus exhibited lower median scores for gait speed subdomain than those without foot problem (median score 3 and 4, respectively; p = 0.02).
DiscussionThe main aim of this study was to investigate whether foot structural disorders and plantar tactile sensitivity were associated with lower extremity physical function impairment in community-dwelling older adults enrolled in a primary health care program. Our results confirmed that older adults with hallux valgus and reduced plantar tactile sensitivity were more likely to present poor physical function. Surprisingly, the prevalence of foot deformities was similar between men and women, and tactile sensitivity impairment was more prevalent among men. Furthermore, tactile sensitivity impairment was associated with age regardless of sex.
Similar to previous studies, hallux valgus, toes deformities, and callosities were the most common foot problems among our participants.2,3,6,7,9 However, we identified only a univariate association between the digital calluses and corns and lower extremity physical function performance that did not persist in the final model. A study by Keysor and collaborators5 performed a similar physical function test in older adults, and they did not find an association between functionality and great toe (bunions, hammer toe, cock-up hallux) or lesser toe deformities.
The implication of an hallux valgus to the lower extremity physical function found in the present study, particularly for the gait speed test, may be attributed to the mechanical importance of such foot region for this motor ability.12 Reduction in range of motion at the first toe region, intrinsic foot muscle weakness,3,11,28 and decrement in propulsive force during walking,11,18,28 have been reported in patients with moderate to severe hallux valgus.3,28 This foot structural problems affect gait speed, the adoption of motor strategies during standing, and it is associated with increased postural sway and risk of falling.2,11,12,18,28 Ultimately, hallux valgus negatively impact the physical function of older adults with potential limitation in overall mobility status.
Plantar sensitivity of the foot also plays an essential role in postural control during standing, walking, and stepping under unpredicted postural perturbations.41,42 Plantar sensitivity impairment, which is considered a marker of the somatosensory system integrity, is strongly associated with an increased risk of falling, impaired mobility, and gait problems.12,43 Cutaneous sensory receptors can provide detailed information about the support surface characteristics in contact with the feet. These receptors also provide sensorial feedback regarding plantar pressure variations and skin stretch, and these somatosensory cues enable subjects to adjust their body configuration in relation to the environment.19 This may explain why our participants with reduced plantar sensitivity exhibited worse performance during the gait speed and chair stand tests.
Previous studies found that older adults with an increased risk of falling were those with decreased ankle flexibility, severe hallux valgus deformity, decreased plantar tactile sensitivity, and muscle weakness of the plantar flexors of the toes.2,12,15 The association between reduced plantar tactile sensitivity and fall risk may reflect an age-related structural and functional decline in the somatosensory system (i.e., the cutaneous mechanoreceptors),23 which may impair the feedback from the feet mainly during dynamic tasks.16 Reduced plantar tactile sensitivity was also previously associated with slow walking speed and difficulty going up and downstairs.24,43 Barr and collaborators43 observed that reduced plantar tactile sensitivity and ankle flexibility were strongly associated with postural instability and fall.12 Thus, interventions that increase ankle flexibility, strength of the plantar flexor muscles, and in particular, enhancement of the sensory information under the plantar region of the foot may improve balance and physical function of older adults, thereby ultimately decreasing their risk of falling.2,12,15
Hallux valgus is usually more prevalent among older women than in men,6,9 and wearing high-heels 27 is a risk factor for feet deformity in women. In our study, we did not find a higher prevalence of hallux valgus in older women. However, there was a trend of toe deformities being more frequent among them (callosity or joint deformities, p-value = 0.05). In a multiethnic community of older adults, differences in foot deformities amongst sex and race/ethnicity were found.44 Different cultures and climate (tropical countries) may influence wearing habits, for example, wearing open-toed footwear. The prevalence of foot deformities may vary between studies, possibly due to these cultural or racial/ethnic disparities and the effects of individual's footwear. However, we could not address this hypothesis with the current design study, and further investigations are necessary to clarify possible etiologic factors of foot deformities and their prevalence between sexes.
Similar to other studies, we verified that plantar sensitivity impairment was more prevalent among men.44 Skin hardness and epidermal thickness of the foot sole are very common with aging due to the physiological modifications of the dermis, it reduces plantar sensitivity,14 and it is associated with higher threshold perception during the monofilament test.45 Considering that men presented thicker skin under the foot, it could explain why, in our study, the impaired plantar tactile sensitivity was more prevalent for men. We also found that the plantar sensitivity impairment was associated with age, regardless of sex. Indeed, plantar tactile sensitivity is progressively affected by aging8,10,21 due to decreased Pacinian and Meissner's receptors and loss of distal large myelinated sensory fibers and receptors,23 in addition to the hyperkeratosis on the sole of the feet.
Multifaceted podiatry interventions and multifactorial interventions involving referral to podiatry have proven to reduce falls among older people.46 Therefore, structural foot problems should be carefully evaluated, and proper interventions should be conducted, such as foot orthoses, foot and ankle exercise programs, and recommendations of adequate footwear for the older population.46
Our results suggest that both hallux valgus and plantar tactile sensitivity impairment were associated with lower extremity physical function (as measured by SPPB) of older adults. Due to the cross-sectional nature of this study, we cannot determine the causality of this association. Therefore, additional studies with different designs are necessary to elucidate this issue. We did not run the regression analysis for men and women separately due to the reduced number of participants, which would affect the statistical power of our results. However, we included sex as a confounder in our regression model. Further studies with a larger sample size are necessary to verify whether the association between foot problems and lower extremity physical function is similar for men and women.
We also recruited a convenient sample of community-dwelling older people, limiting the external validation of our results. Another possible limitation was that the same evaluator assessed foot problems and conducted the physical function tests. Although valid and reliable measures could imply a certain level of subjectiveness, we are confident that the lack of blinding did not influence our regression estimates. The strength of our study lies in the fact that participants were enrolled in a primary health care setting where the integrated pathway of care should take place according to the World Health Organization's recommendation to promote healthy aging trajectories.47 Our results highlight the importance of identifying foot problems in older adults due to its association with lower extremity physical function decline and mobility loss. Future clinical trials should investigate the effectiveness of interventions combining plantar tactile sensitivity enhancement and podiatry interventions to improve the overall mobility of older adults.
ConclusionHallux valgus and impaired plantar sensitivity were associated with reduced lower extremity physical function in older adults. Foot problems in older adults can be a potential factor for loss of mobility, and physical therapists could include these foot assessments in their clinical practice for older adults. Further studies are necessary to identify the nature of this relationship and to what extent management of these foot problems can improve general mobility and quality of life of older adults.
Prado-Rico is thankful to Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES - Finance Code 001) for her scholarship. Perracini is thankful to the National Council for Scientific and Technological Development CNPq for her Research Productivity Scholarship. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.