The Fonseca Anamnestic Index is a questionnaire used to classify individuals with temporomandibular disorders. Previous studies have shown that the Fonseca Anamnestic Index provides a multidimensional measurement of the temporomandibular disorders construct and that the main dimension presents a good fit to the model according to the item response theory.
ObjectiveTo evaluate the between-day reliability, accuracy, and best cut-off score of the Short-Form Fonseca Anamnestic Index for the diagnosis of myogenous temporomandibular disorders.
MethodsThe sample consisted of 123 women (57 with myogenous temporomandibular disorders and 66 asymptomatic), evaluated by the Research Diagnostic Criteria for Temporomandibular Disorders. The participants answered the Short-Form Fonseca Anamnestic Index on two occasions with a seven-day interval between tests. For the analysis of between-day reliability, the intraclass correlation coefficient, the standard error of measurement and the minimum detectable change were used. The Receiver Operating Characteristic curve was used to determine the diagnostic accuracy and the best cut-off point.
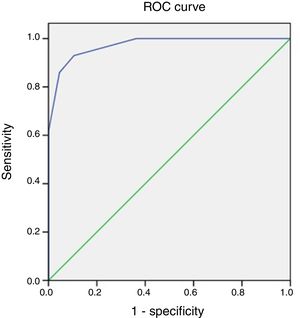
ResultsThe Short-Form Fonseca Anamnestic Index demonstrated excellent reliability (intraclass correlation coefficient≥0.95) for all items and for the total Short-Form Fonseca Anamnestic Index score (intraclass correlation coefficient=0.98; standard error of measurement=3.28; minimum detectable change=9.09). The level of accuracy of the Short-Form Fonseca Anamnestic Index for the diagnosis of myogenous temporomandibular disorders was high (area under the curve of 0.97), with a better cut-off score of 17.5 points.
ConclusionThe Fonseca Anamnestic Index should be used in its short form to classify the absence of myogenous temporomandibular disorders (scores between 0 and 15 points) or presence of myogenous temporomandibular disorders (scores between 20 and 50 points) in women.
Temporomandibular disorders (TMD) involves a series of clinical alterations involving the masticatory muscles, the temporomandibular joints (TMJ), and their associated structures.1 The most common signs and symptoms of TMD are pain in the TMJ, pre-auricular region, cervical spine, face, and/or head, fatigue of cervical muscles, craniofacial muscles, and/or masticatory muscles, TMJ mobility limitation, jaw deviation, and unusual joint sounds.2
Epidemiological studies have found that TMD-related symptoms occur predominantly in young women between the ages of 20 and 40 years.3,4 TMD presents with a multifactorial etiology that can be classified as predisposing factors when they increase the risk of developing dysfunction, beginner factors when they provoke the onset of the condition, or perpetuating factors when they interfere in the cure or favor the progression of TMD.5 In addition, because it is a multifactorial dysfunction, the diagnosis of TMD becomes complex and very controversial and therefore it is recommended that it be conducted by a multidisciplinary team composed of several allied-health professionals.6
Thus, to obtain the diagnosis of TMD, instruments such as the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) and the Fonseca Anamnestic Index (FAI)7,8 have been developed. The RDC/TMD has demonstrated a high level of accuracy and reliability in the diagnosis of myogenous TMD and has become widespread in its use as a validated and standardized diagnostic tool for TMD dysfunction.9 However, this instrument is difficult to apply because of the long protocol, the need for face-to-face evaluation,10 and the need for evaluator training and experience.11 It is important to emphasize that the RDC/TMD has been updated to the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD),12 with the purpose of improving the description of the procedures and diagnosis for clinical practice and research. However, the new version has not yet been clinimetrically tested for the Brazilian population.
The FAI is a patient-reported outcome in which a volunteer answered questions on the questionnaire. This index is a simple, easy, and low-cost tool that displayed the signs and symptoms of TMD and classified the condition according to its severity.13
In previous studies, some authors have already established information on the accuracy and reliability of the FAI, among them Berni et al.,8 who demonstrated its high accuracy for the diagnosis of individuals with or without myogenous TMD, and Campos et al.,10 who reported good to excellent reproducibility for some items of the FAI. However, the analyses of these surveys were performed using all of the items of the FAI, ruling out the possibility of its multidimensionality.
Rodrigues-Bigaton et al.14 recently demonstrated the multidimensionality of the FAI and established that its main dimension was composed of items 1, 2, 3, 6, and 7. Therefore, the present study proposed to evaluate the reliability and accuracy of the Short-Form Fonseca Anamnestic Index (SFAI), taking into account the importance of establishing an ideal cut-off score for the diagnosis of individuals with myogenous TMD, for the possible use of a short version of the index, and considering that there have been no reports on the accuracy and best cut-off score of this dimension. It is also important to calculate the diagnostic accuracy of the SFAI instrument to ensure that researchers and/or clinicians can use it with confidence. Thus, this study hypothesized that the SFAI would present adequate reproducibility, sensitivity, and specificity in the diagnosis of myogenous TMD.
MethodsStudy designThis study was a cross-sectional observational study analyzing the accuracy and diagnostic reliability of the SFAI. The study was approved by the Research Ethics Committee of Universidade Metodista de Piracicaba (UNIMEP), Piracicaba, SP, Brazil (protocol number 15/11). All subjects were informed about the evaluation procedures and signed an informed consent. It is important to note that this study followed the recommendations of the STAndards for the Reporting of Diagnostic accuracy studies (STARD),15 the Guidelines for Reporting Reliability and Agreement Studies (GRRAS)16 and the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN).17
SampleBetween 2006 and 2016, a total of 123 women were recruited from the city of Piracicaba, SP, Brazil. The invitation was made through verbal invitation, posters, and dissemination via websites. After recruitment and screening of the eligibility criteria, the subjects were allocated to the myogenous TMD Group (n=57) and assymptomatic group (n=66) according to the RDC/TMD.
Inclusion criteriaAfter administration of the RDC/TMD, women with a myogenous TMD diagnosis were selected for the study: myofascial pain (Ia) or myofascial pain with limitation of mouth opening (Ib). Associated diagnoses, such as disk displacement (IIa, IIb, and IIc) and arthralgia (IIIa), were also allowed.
Exclusion criteriaWomen were excluded from the study if they were under general orthodontic or pharmacological treatment (i.e. analgesic, anti-inflammatory, and/or muscle relaxant drugs) or physiotherapeutic treatment for TMD, used a partial or total dental prosthesis, or had tooth loss, trauma to the face and TMD, had a history of subluxation or dislocation of TMJ, or had a arthrogenous TMD diagnosis (IIIb – osteoarthritis or IIIc – osteoarthrosis) according to the RDC/TMD.
Instruments used for evaluationResearch Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD)The RDC/TMD is a diagnostic tool for TMD that allowed the classification of individuals into three groups: I – myogenous disorder, II – disc displacement, and III – other joint conditions. The RDC/TMD was used as a reference standard instrument in the present study and the volunteers diagnosed with a myogenous disorder (Ia and Ib) were included due to the already established record of reliability (kappa>0.75, excellent level)18 and accuracy (sensitivity>0.75; specificity>0.95, appropriate level)18,19 of this instrument in the diagnosis of muscular origin dysfunction of the TMJ. The physical examination, axis I of the RDC/TMD, was administered by trained evaluators in the use of the instrument, and axis II was answered by the volunteers individually in a well-lit and air-conditioned laboratory without time restriction.
Fonseca Anamnestic Index (FAI)The FAI was developed in the Brazilian-Portuguese language to assess the severity of TMD, based on its signs and symptoms. This Index was created with 10 items with 3 options of answers (specific scores): “yes (10 points)”, “sometimes (5 points)” and “no (0 points)”.13 The final score of the instrument is determined by the sum of the scores of all items, allowing the following classifications: absence of signs and symptoms of TMD (0–15 points), mild TMD (20–45 points), moderate TMD (50–65 points), and severe TMD (70–100 points).20 In the present study, this total score was not considered, since the accuracy analysis was evaluated in the main dimension of the FAI (items 1, 2, 3, 6, and 7),14 designated the Short-Form Fonseca Anamnestic Index (SFAI) in this study, to determine the best cut-off score for the instrument or considering the possible total score of 50 points (5 items).
The main dimension items selected for evaluation were as follows: (line [I]1) Do you have difficulty opening your mouth?; (I2) Do you have difficulty moving your jaw to the side?; (I3) Do you have muscle fatigue/pain when you chew?; (I6) Do you have pain in your ear or your joints (TMJ)? (I7) Have you ever noticed if you have noises in the TMJ when you chew or when you open your mouth?
ProceduresAfter the evaluation according to the RDC/TMD, the subjects answered the SFAI in the laboratory, and the second evaluation was carried out via telephone by a single rater. It is important to note that after the first administration of the SFAI, it was readministered seven days later by means of a telephone call in order to evaluate its reproducibility (i.e. between-day reliability). The subjects were asked to answer the five items of the SFAI (in both evaluations) with “yes”, “sometimes”, or “no”, emphasizing that only one answer was to be marked for each item. There was no time limit for completing the questionnaire the first time.
Statistical analysisConsidering the SFAI, the intraclass correlation coefficients (ICC) statistic was used for the SFAI between-day reliability analysis (ICC3,1; model: two-way mixed; type: absolute agreement – single measurement). The ICC values were evaluated on each item of the SFAI, as well as the total score.
The reliability level was determined according to the classification proposed by Weir21 ranging from: 1.0 to 0.81 (excellent realiability); from 0.80 to 0.61 (very good reliability); from 0.60 to 0.41 (good reliability); from 0.40 to 0.21 (reasonable reliability); and from 0.20 to 0.00 (poor reliability). The standard error of measurement (SEM) was calculated using the equation: SEM=standard deviation∗(1−ICC), and the minimum detectable change (MDC) was calculated using the equation: MDC=1.96*SEM*2.
The Receiver Operation Characteristic curve (ROC curve) was calculated to determine the diagnostic accuracy (by measuring the area under the curve – AUC), the best cut-off score, sensitivity (i.e. the proportional value that measures the instrument's ability to diagnose true-positive cases) and specificity (i.e. the proportional value that measures the instrument's ability to diagnose true-negative cases). The values used for AUC classification followed the recommendations of Greiner et al.22 and Akobeng23: 0.5 (due to chance); >0.5 to 0.7 (low level of accuracy), >0.7 to 0.9 (moderate level of accuracy), and >0.9 to 1.0 (high level of accuracy). The best cut-off score was determined according to the lowest value obtained with the equation: (1−sensitivity)2+(1−specificity)2.
The following percentages were also calculated for the SFAI: positive predictive value (i.e. the ratio of true-positives to true-positives added by false-positives diagnosed by the analyzing instrument); negative predictive value (i.e. the ratio of true-negatives to true-negatives added by false-negatives diagnosed by the analysizing instrument); positive likelihood ratio (i.e. the ratio between the probability of a true-positive and the probability of a true-negative, calculated using the equation: Sensitivity1−Specificity, with high values indicating a better index validity), and the negative likelihood ratio value (i.e. the ratio between the probability of a true-negative and the probability of a true-positive, calculated using the equation: 1−SensitivitySpecificity, with low values indicating better index validity).
All data were processed using SPSS software, version 13.0 (Chicago, IL, USA).
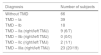
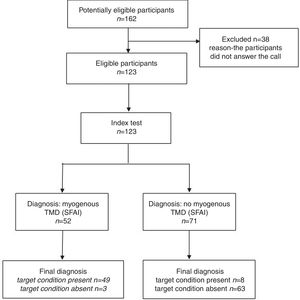
ResultsA total of 160 women were recruited, 37 of whom were excluded because they refused to complete the SFAI at the second evaluation of this study (i.e. by telephone call), according to Fig. 1. Thus, 123 women were evaluated and divided into myogenous TMD group (n=57, mean age=24.5, SD=5.2) and asymptomatic group (n=66, mean age=25.1, SD=5.2). According to the RDC/TMD (Table 1), the subjects with TMD were diagnosed with myofascial pain (Ia) or myofascial pain with limited mouth opening (Ib) and simultaneous diagnoses of disk displacement (IIa, IIb and IIIc) or arthralgia (IIIa).
Diagnosis of TMD in subjects based on to the Research Diagnostic Criteria for Temporomandibular Disorders, n=123.
| Diagnosis | Number of subjects |
|---|---|
| Without TMD | 66 |
| TMD – Ia | 39 |
| TMD – Ib | 18 |
| TMD – IIa (right/left TMJ) | 9 (6/7) |
| TMD – IIb (right/left TMJ) | 0 (0/0) |
| TMD – IIc (right/left TMJ) | 2 (1/1) |
| TMD – IIIa (right/left TMJ) | 23 (20/19) |
TMD, temporomandibular disorder; TMJ, temporomandibular joint; Ia, myofascial pain; Ib, myofascial pain with limited mouth opening; IIa, disc displacement with reduction; IIb, disc displacement without reduction; IIc, disc displacement without reduction and without limited mouth opening; IIIa, arthralgia.
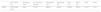
Table 2 shows the reliability values of each index question, with values very close to 1 demonstrating excellent reliability.
Reliability statistics applied to the selected items of the SFAI.
| ICC3,1 (95% CI) | SEM (score) | MDC (score) | Classification | |
|---|---|---|---|---|
| Item 1 | 0.97 (0.96–0.98) | Na | Na | Excellent reliability |
| Item 2 | 0.95 (0.93–0.97) | Na | Na | Excellent reliability |
| Item 3 | 0.96 (0.94–0.97) | Na | Na | Excellent reliability |
| Item 6 | 0.95 (0.93–0.97) | Na | Na | Excellent reliability |
| Item 7 | 0.97 (0.96–0.98) | Na | Na | Excellent reliability |
| Total SFAI score | 0.98 (0.98–0.99) | 3.28 | 9.09 | Excellent reliability |
ICC, intraclass correlation coefficient; SEM, standard error of mean; MDC, minimal detectable change; Na, not applicable; CI, confidence interval.
Fig. 2 shows a ROC curve with distribution of the SFAI scores in the upper left quadrant of the graph.
Table 3 shows a high sensitivity value (49 cases of TMD diagnosed by the SFAI compared to 57 cases of TMD diagnosed by the RDC/TMD), a high positive predictive value (49 TMD cases diagnosed by the SFAI confirmed by the RDC/TMD, of 52 cases of TMD diagnosed in total by the SFAI) and high positive likelihood ratio (PLR=19.11; 95% CI=6.23–57.42). There was also a high specificity value (63 cases of absence of TMD diagnosed by the SFAI compared to 66 cases of absence of TMD diagnosed by the RDC/TMD), high negative predictive value (63 cases of absence of TMD diagnosed by the SFAI confirmed by the RDC/TMD of 63 cases of absence of TMD diagnosed in total by the SFAI), and low negative likelihood ratio (NLR=0.14; 95% CI=0.08–0.28).
Area under the ROC curve (AUC), best cut-off score, sensitivity, specificity, predictive values, and likelihood ratios of the SFAI (from the first session).
| AUC (95% CI) | Standard error | Cut-off point (score) | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | PLR | NLR | |
|---|---|---|---|---|---|---|---|---|---|
| SFAI | 0.97 (0.95–0.99) | 0.02 | 17.50 | 86.00 | 95.50 | 94.20 | 99.70 | 19.11 | 0.14 |
CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value; PLR, positive likelihood ratio; NLR, negative likelihood ratio.
A high level of accuracy of the SFAI for diagnosis of myogenous TMD was observed, with the best cut-off score established with a value of 17.50. With this cut-off score and considering the multiple SFAI score of five with its main dimension totaling a maximum of 50 points, the score was set from 0 to 15 for the diagnosis of women without myogenous TMD, and the score of 20–50 for women with myogenous TMD. It is important to emphasize that in the readministration of the SFAI, used for the reliability analysis, a high level of accuracy (AUC=0.94; 95% CI=0.89–0.98) was also observed, with the best cut-off score established with a value of 17.50 points.
The mean total score obtained in the first administration of the SFAI was 6.67 (SD=9.66) for the asymptomatic group and 33.9 (SD=10.3) for the myogenous TMD group. Therefore, in the readministration of the SFAI (i.e. by telephone), the scores were 6.97 (SD=9.91) for the asymptomatic group and 33.6 (SD=10.6) for the myogenous TMD group.
DiscussionRegarding the analysis of between-day reliability, the present study found an excellent level of reliability for the items of the main dimension of the FAI. The findings of Campos et al.,10 a study that investigated and estimated the internal consistency and reproducibility of the FAI, corroborate those of the present study, as they found adequate reliability for items 1, 2, 3, 5, 6, 7, and 9 of the FAI. Moreover, the authors explain that the use of the RDC/TMD in large epidemiological studies might become unfeasible depending on the interview technique and/or the time available for data collection, therefore the FAI could be an important practical instrument.
It is known that TMD represented a group of conditions of orofacial pain with prevalence of 5% in the American population,4 80–90% in Brazilian university students,24 and a higher prevalence in females.4 Over the years, studies have evaluated the accuracy of several instruments for the diagnosis of TMD.25 Although the RDC/TMD is currently the reference standard for the diagnosis of myogenous TMD,9 it is difficult to use because of the long administration protocol and the need for training and experience by the evaluator.10
In order to justify the aims of this study, it is worth noting that a systematic review of the literature has shown that the low methodological quality of most studies addressing the accuracy of assessment tools for the diagnosis of TMD has rendered the support or rejection of commonly employed tests impossible,26 thus reinforcing the importance of studies investigating the accuracy of TMD diagnostics.8
Based on the above disadvantages, it is important to evaluate the accuracy of the FAI given that it is simple, quick, and inexpensive, and does not require evaluator experience, making it possible to administer it even in epidemiological studies.27 However, previous studies observed that FAI items 4, 5, 8, 9, and 1024,25,28 had limitations for the evaluation of TMD signs and symptoms and Rodrigues-Bigaton et al.14 verified the multidimensionality of the index by establishing its main dimension with adequate values of internal consistency and well-adjusted to the model according to the analysis of the theory of response to the item (i.e. a Rasch analysis). Therefore, the present study evaluated the accuracy, best cut-off point, and reproducibility of the Short-Form FAI (i.e. the main dimension of the FAI), which have not yet been analyzed in the literature, as previously suggested.14,29
It is also important to highlight the need to define a dichotomous classification (i.e. the presence or absence of myogenous TMD) for the use of the main dimension of the FAI, in order to counteract the classification of TMD severity previously proposed by Fonseca et al.13 Thus, with the high level of accuracy found and a cut-off score of 17.5 points in the SFAI, the present study was the first to determine that individuals should be diagnosed with myogenous TMD when they reached scores between 20 and 50 points and should not be diagnosed with myogenous TMD if they do not exceed the 15-point score. It is noteworthy that the SFAI demonstrated a greater ability to diagnose women without myogenous TMD than women with the disorder, expressed by the higher negative predictive value compared to the positive predictive value. In addition, these SFAI scores should be used for myogenous TMD and not for arthrogenous TMD (i.e. osteoarthritis and osteoarthrosis), since these subtypes were not allowed in this study.
The findings of Berni et al.8 corroborate the present study, since they found high accuracy of the FAI (AUC=0.94). Two hundred and three female volunteers participated in their study, 117 with myogenous TMD and 86 without TMD. All volunteers were evaluated with the RDC/TMD as the reference standard for the diagnosis. They found that the best cutoff score was a score of 47.50. Thus, scores ranging from 0 to 45 points corresponded to the absence of myogenous TMD and scores ranging from 50 to 100 points identified individuals with the disorder. However, the authors used the 10 items to perform the analysis of accuracy, disregarding the multidimensionality of the index, which differs from the present study which used multidimensionality as the main dimension of the index, making it difficult to compare the findings.
Another study also evaluated the accuracy of the FAI for the diagnosis of TMD in children and adolescents,30 however, the authors found inadequate levels of accuracy and attributed the results to difficulty in understanding the language used in the self-explanatory items of the index, which corroborates with the present study, since perhaps the real reason for the inadequate accuracy found by these authors was due to the fact that the FAI was administered in full and not just its main dimension.
Based on the results, the SFAI replaces the use of the long-form of the FAI with a short form (SFAI) as it was, much easier and faster to administer and discarded the old assessment of the severity of the disorder. Therefore, it is important to emphasized that the short-form could be used as a quick and reliable screening tool in scientific and clinical settings, but an appropriate diagnosis to guide the treatment of the myogenous TMD should be determined by using the reference standard instrument (DC/TMD).
There are a few factors in the present study that could be considered limitations, such as: the restriction of the results to women, the extrapolation of the structural results found here to other TMD subtypes according to the RDC/TMD (i.e. arthrogenous TMD) and limitation in the comparison of the findings with the international literature, since the index was developed in Brazilian-Portuguese without other language versions, restricting its administration to Portuguese speakers. It is still important to note that the new DC/TMD12 is intended for use within any clinical setting and supports the full range of diagnostic activities from screening to definitive evaluation and diagnosis. However, as it has not yet been clinimetrically tested for the Brazilian population and, to maintain an adequate evaluation methodology, the reference standard instrument used in this study was the RDC/TMD.
Finally, the SFAI presented properties of important measures for a Brazilian questionnaire that should be used to conduct well-designed clinical trials and prevalence studies in the area of physical therapy in individuals with myogenous TMD. For future studies, it would be useful to translate the SFAI into another language and perform the accuracy analysis of the SFAI using the DC/TMD as the reference standard instrument.
ConclusionThe Short-Form Fonseca Anamnestic Index (SFAI) shows a high level of diagnostic accuracy and may be used as a new version of the index for the diagnosis of myogenous TMD. Women with scores between 0 and 15 points should be considered to not have a diagnosis of myogenous TMD, and those with scores between 20 and 50 points should be diagnosed as having myogenous TMD. The short-form can be used as a screening tool and indicates the diagnosis of myalgia, however, it is important to have a proper diagnosis to guide the treatment of the disorder using the DC/TMD.
Conflicts of interestThe authors declare no conflicts of interest.