Physical disability significantly impacts health outcomes and is linked to higher mortality in older adults. However, research on its association with hospitalization rates remains limited.
ObjectiveTo assess whether physical disability is a predictive measure of hospitalization (yes/no) in older individuals. Additionally, we tested whether physical disability predicts the frequency of hospitalizations (≤ 3 or >3).
MethodsThis is a cross-sectional analysis of a dataset from the National Health and Nutrition Examination Survey (NHANES). We analyzed data from 2009-2018 from participants older than 65 years. Hospitalization status was determined using the Hospital Utilization and Access to Care questionnaire. Physical disability was assessed (yes/no) with the 4–item physical functioning questionnaire during an in–home interview to assess the participant’s level of physical disability. The questionnaire asked about difficulty in walking from room to room (on the same level), standing up from an armless chair, eating, and dressing. Multivariable logistic regression model adjusted for age, sex, race/ethnicity, number of medications, number of comorbidities, and poverty index was used.
ResultsA total of 4346 participants met our inclusion criteria. The adjusted logistic regression model revealed that older adults with physical disability have greater odds to be hospitalized than those without physical disability (adjusted odds ratio [OR]: 2.13; 95% confidence interval [CI]: 1.74, 2.62). Secondary analysis also showed that older people with physical disability have greater odds to have 4 or more hospitalizations in one year in comparison with older adults who do not show physical disability (adjusted OR: 5.81; 95% CI: 2.40, 14.05).
ConclusionThe results reveal that physical disability is strongly associated with higher odds of hospitalization among older individuals. These data reinforce the importance of health policies and programs to prevent physical disability in this population.
Population ageing is increasing worldwide, with important implications to public health.1 Current projections indicate that by year 2030 one in every six individuals in the world will be aged 60 years and older, with an estimated population of over 2 billion by 2050.1 This implicates unprecedented economic, cultural, medical, social, public health, and public policy challenges, as this population is already prone to multiple comorbidities, chronic conditions, and functional limitations.1,2
Physical disability (i.e., the inability to adequately perform activities of daily living) has been considered a good predictor of health outcomes both in community dwelling and hospitalized older population.3-5 Indeed, functional status has been shown a strong predictor of short-term mortality in non-institutionalized older individuals, independent of age and health status.5 In hospitalized patients, physical disability has been associated with greater mortality both intra-hospital and after medical discharge.6-8 For instance, Matzen et al.9 showed that the score on the Barthel Index, assessed at hospital admission, is associated with 3- and 12-month mortality. Similarly, functional decline has been associated with higher odds of 30-day out-of-hospital mortality.9
Collectively, data suggest that physical disability plays a pivotal role in health outcomes, with the existing literature indicating an important association with mortality in the ageing population. However, data are still lacking on the possible associations between physical disability and hospitalization incidence. The present study aims to assess whether physical disability is a predictive measure of hospitalization in older individuals. Additionally, we tested whether physical disability predicts the frequency of hospitalizations in this population.
MethodsThis is a cross-sectional analysis of a dataset from the National Health and Nutrition Examination Survey (NHANES). NHANES is a large, multistage, complex survey of the civilian, noninstitutionalized US population conducted by the National Center for Health Statistics (NCHS). Briefly, it consists of a stratified, multistage probability cluster sampling designed to collect health and nutritional data from a representative sample of the US population. Detailed descriptions of NHANES methods are published elsewhere.10 The NHANES obtained approval from the National Center for Health Statistics Research Ethics Review Board and participants provided written consent.
Study sampleThe dataset included in the current study refers to five consecutive cycles of NHANES (i.e., 2009–2010, 2011–2012, 2013–2014, 2015–2016, and 2017–2018). Our exclusion criteria were the following: 1) men and women aged under 65 years; 2) missing data for disability questionnaire; 3) missing data for hospital utilization and access to care questionnaire and; 4) missing data for covariates included in the adjusted logistic regression models (i.e., age, sex, race/ethnicity, medications, comorbidities, and poverty index).11
Outcome – hospitalizationHospitalization status was determined using the Hospital Utilization and Access to Care questionnaire.12 Participants were asked whether they had been admitted to a hospital for more than one night in the past 12 months, disregarding an overnight stay in the emergency room. Those who answered affirmatively were further queried about the frequency of hospitalizations within the past year.
Physical disabilityPhysical disability (yes/no) was assessed with the 4–item physical functioning questionnaire during an in–home interview to assess the participant’s level of physical disability. The questionnaire asked about difficulty in walking from room to room (on the same level), standing up from an armless chair, eating, and dressing. A participant's answer to a given question was coded as “no difficulty”, “some difficulty”, “much difficulty”, or “unable to do”. Response was set to missing when participants answered “unknown” or “do not do” the activities. The responses were based on a participant's subjective self-assessment without further explanations. Physical disability was defined as any difficulty in performing one or more items.13,14
Statistical analysisThe primary analysis of the study aimed to assess whether physical disability is a predictive measure of hospitalization (yes/no) in older individuals. Additionally, as a secondary analysis, we tested whether physical disability predicts the frequency of hospitalization (≤ 3 or ≥ 4) in this population. A multivariable logistic regression model adjusted for age (<80 or ≥80 years), sex (male or female), race/ethnicity (Mexican-American, other Hispanics, non-Hispanic whites, non-Hispanic blacks, and others), number of medications (<3 or ≥3), number of comorbidities (1 or ≥2), and poverty index (≤1 or >1) was used to assess the potential association between variables.15-17
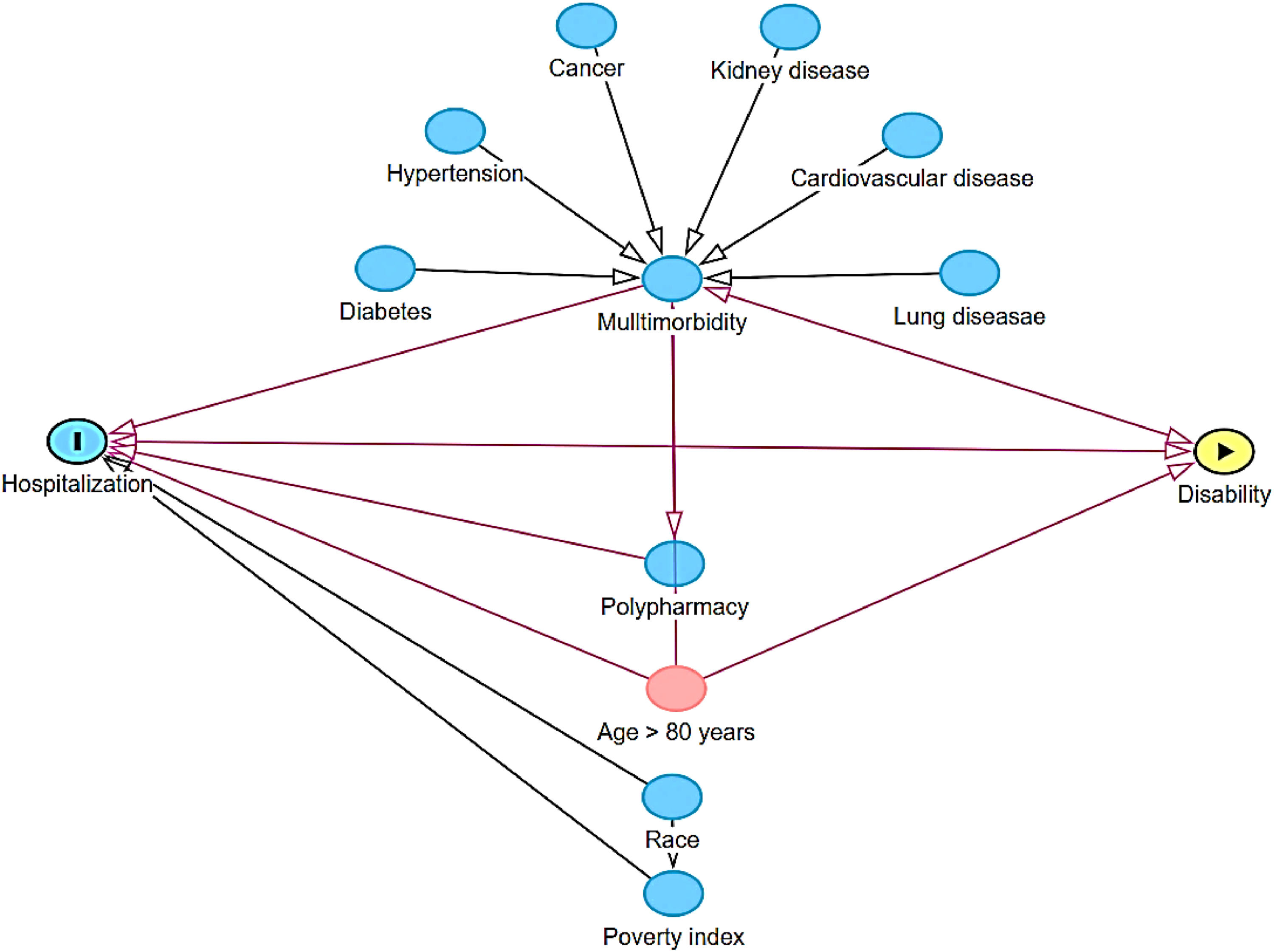
Continuous variables were described as mean and standard deviation, and categorical variables as absolute and relative frequency. Confounders were selected based on a Direct Acyclic Graph (DAG, www.dagitty.net), which is a causal diagram based on causal relations between the exposure, outcome, and potential confounders.18 The DAG was developed from a priori knowledge to identify a minimum, yet sufficient, set of covariates to remove confounding factors from the statistical analysis19-21 (Fig. 1). Odds ratios (OR) were calculated along their corresponding 95 % confidence intervals (95 % CI). Significance level was set at 0.05. All analyses were performed in the statistical environment R (version 3.5.3; R Core Team 2020), using tidyverse22 and survey23 packages. Data were analyzed using the survey design. Proper weighting procedures for weighting multiple years of NHANES data (i.e., 8 years) were employed for this study considering the complex survey design according to NHANES guidelines considering complex sample design and sample weight.24
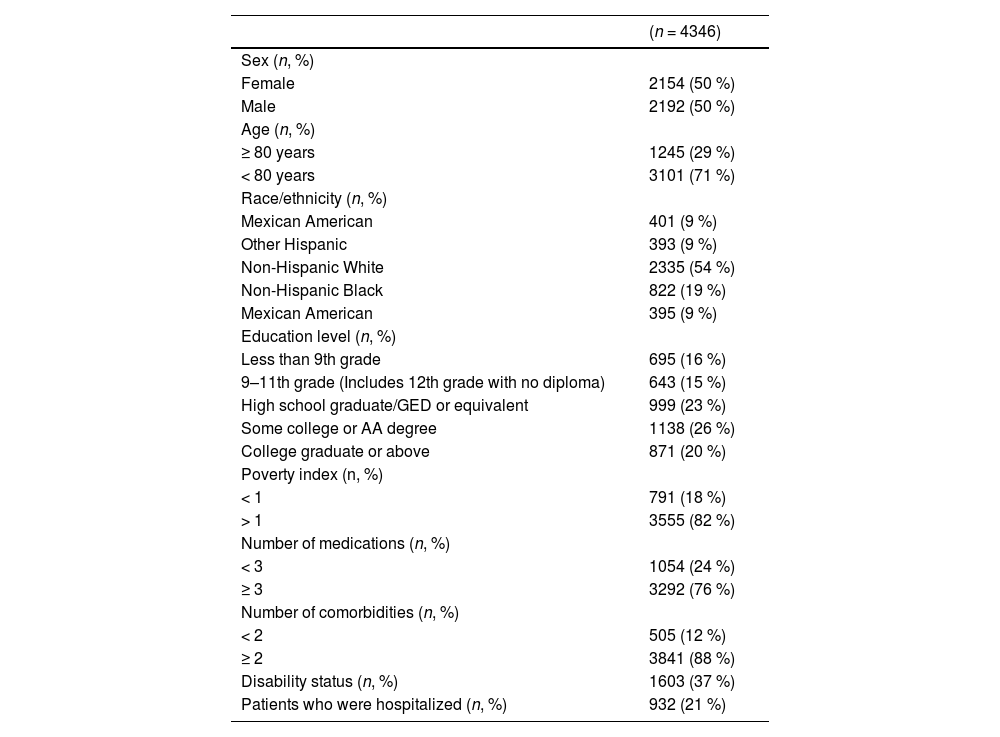
ResultsA total of 49,693 individuals were assessed in NHANES 2009–2018, of which 4346 were older adults and met our inclusion criteria. Overall, the sample included older adults of both sexes (50 % female) with a mean (SD) age of 73 (5) years. Eighteen percent of participants were below the poverty line, 76 % were using at least 3 chronic medications, and 88 % had at least 2 comorbidities. The prevalence of diabetes, cancer, heart attack, stroke, congestive heart failure, kidney disease, and liver disease was 29 %, 26 %, 12 %, 11 %, 10 %, 8 %, and 5 %, respectively. Thirty-seven percent of the older adults had at least one physical disability, and 21 % had been hospitalized at least once in the past 12 months. Table 1 presents detailed demographic, clinical, and disability data of the participants.
Demographic and clinical characteristics of older adults.
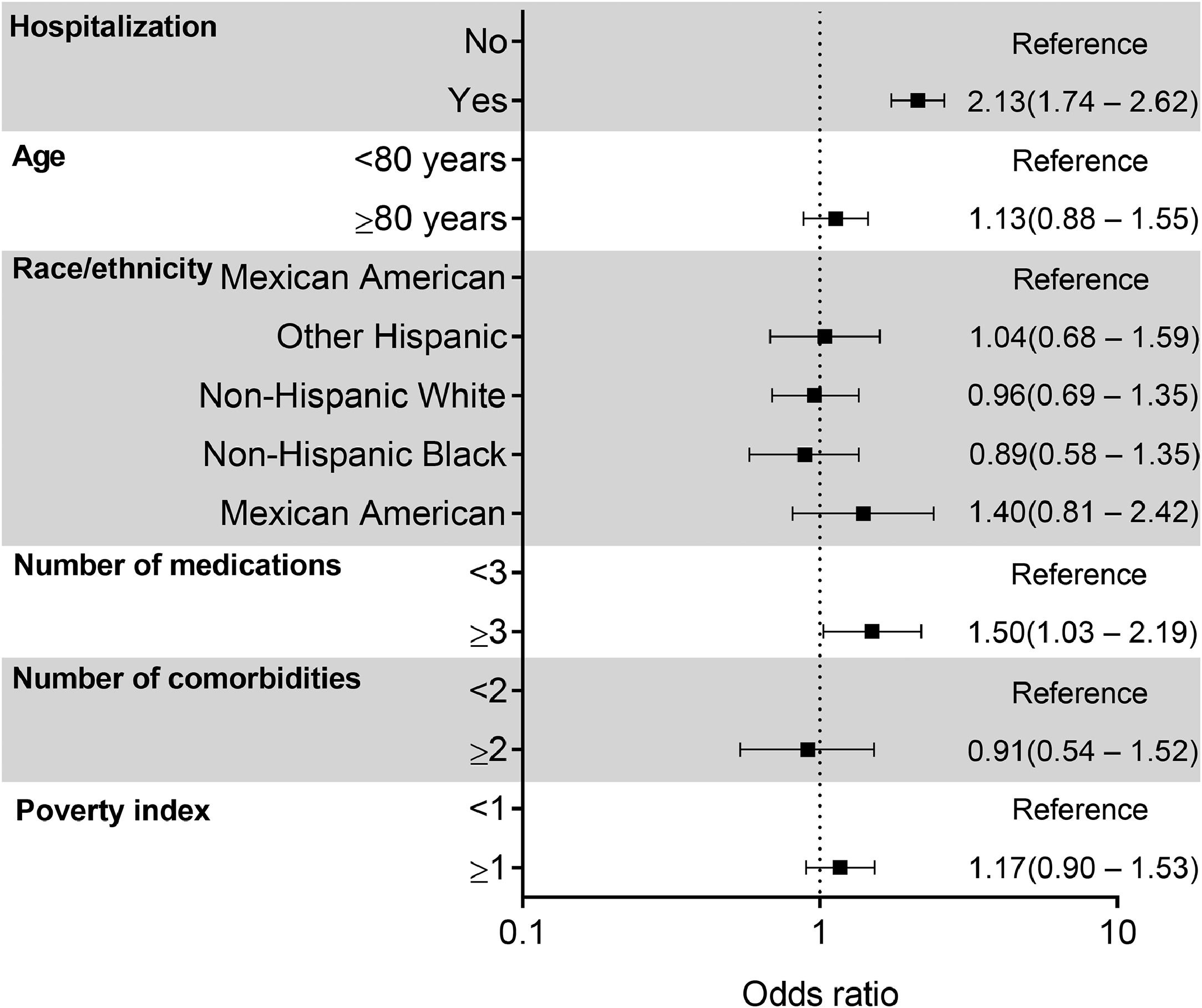
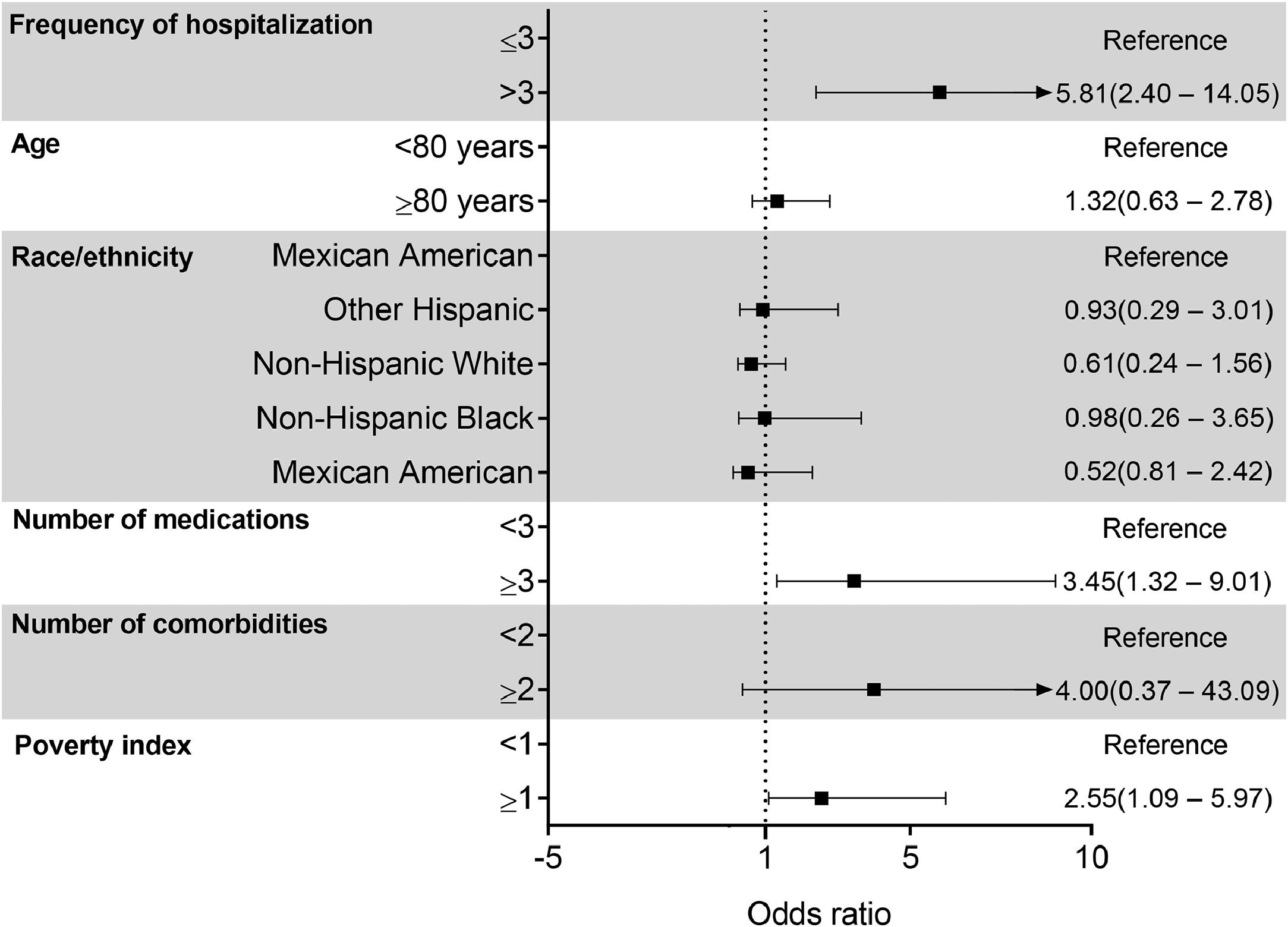
The adjusted logistic regression model revealed that older adults with physical disability (any difficulty in completing one or more items of the questionnaire) had greater odds to be hospitalized than those who did not present physical disability (adjusted OR: 2.13; 95 %CI: 1.74, 2.62) (Fig. 2). For secondary analysis, the adjusted model also showed that older individuals with physical disability had greater odds to have 4 or more hospitalizations in one year in comparison with those not showing physical disability (adjusted OR: 5.81; 95 % CI: 2.40, 14.05). Additionally, the secondary analysis revealed that both the number of medications and poverty index are significant predictors of hospitalization frequency. Specifically, older adults who take three or more medications, or display a poverty index higher or equal to 1, are more likely to experience frequent hospitalizations (≥ 4) within a year compared to those who take fewer than three medications (adjusted OR: 3.45; 95 %CI: 1.32, 9.01) or display a poverty index lower than 1 (adjusted OR: 2.55; 95 %CI: 1.09, 5.97) (Fig. 3).
The present study aimed to investigate whether physical disability is a predictive measure of hospitalization in older individuals. Our main findings indicate significant associations between physical disability and likelihood of hospitalization. Moreover, physical disability was also predictive of re-hospitalization episodes within a year.
Preserving the ability to perform home and community daily activities is of paramount importance for independence at an older age.25 Conversely, physical disability is associated with adverse health outcomes, including increased mortality.5-9 Although multifactorial26 disability relates to common causes of hospitalization among older individuals, such as chronic diseases, sedentary behavior, and age-related sarcopenia.26 Our data extend this notion by showing that older adults with any level of physical disability were found to have more than twice the odds of being hospitalized compared to their non-disabled counterparts.
We have also demonstrated that having functional impairment implied significantly higher chances of experiencing several hospitalizations over the course of a year, indicating that functional impairment is not only a predictor of initial hospitalization but also of recurrent hospital admissions. Hospitalization per se is thought to have significant impacts to overall health,27 including impaired functional mobility,3,28,29 as it increases sedentary time, a major driver of physical disability.30 Also, this increased vulnerability exacerbated by disability translates into higher chances for frequent hospitalization, leading to an additional burden on health systems, with higher costs of healthcare.31
Although our findings indicating a significant association between physical disability and hospitalization are relevant, some caution is needed when extrapolating these results to other nations like Brazil. For example, in a probabilistic sample of the Brazilian population, physical disability increased the odds of hospitalization by 277 %,32 which is higher than values observed in the current study (113 %). This disparity can be analyzed from several perspectives, including cultural, and healthcare infrastructure differences between countries. These factors can influence how individuals with physical disabilities are treated and, consequently, affect the odds of hospitalization. Additionally, individuals with physical disabilities in Brazil may encounter greater barriers to healthcare access, which could lead to higher hospitalization rates.
In this context, our data suggest that public health policies should be directed at ensuring prevention, early identification, and management of physical disabilities, thereby reducing hospital admissions, enhancing resource allocation, and ultimately improving well-being and independence among older people.33,34 Additionally, it also warrants further research considering targeted interventions and support systems that could adequately respond to these vulnerabilities, hence looking at the long-term benefits that such strategies will have in reducing healthcare costs and improving patient outcomes among older individuals.
The current study presents some limitations. Firstly, the cross-sectional nature of the data does not allow causal inference between physical disability and hospitalization, while self-reports might induce recall bias or inaccurate reporting. The specific types and reasons for hospitalization are not detailed, which limits the understanding of the nature of the associations observed. Even though models were adjusted for covariates, there may be other unmeasured confounding variables that would affect the results. In addition, although being representative of the United States population, our data are non-generalizable to other populations. Nonetheless, the current findings concur with the existing literature at pointing to the negative impact of physical disability on health. The present study moves one step further by showing the relationship between functional impairment and hospitalization incidence to provide a better understanding of the health trajectories of older persons with disabilities.
ConclusionThe results of the present study show that physical disability is strongly associated with higher odds of hospitalization. Our analyses of NHANES data from 2009 to 2018 suggest that older adults with any level of physical disability are more than two times more likely to be hospitalized compared to those without physical disability. Moreover, functional impairment not only significantly predicts initial hospital admissions, but it is also a strong predictor of re-hospitalizations within a year. These results suggest that tackling physical disability could contribute to reduce the burden on healthcare systems and increase the quality of life in this population.
None to declare.
H.R is supported by grants from CNPq (306995/2022-0).



![Multivariate-adjusted logistic regression analysis (odds ratio [95 % CI]) of the association between disability with hospitalization. Multivariate-adjusted logistic regression analysis (odds ratio [95 % CI]) of the association between disability with hospitalization.](https://static.elsevier.es/multimedia/14133555/0000002900000006/v1_202510310759/S1413355525000838/v1_202510310759/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w90NRiOl/KnYC22JyCfllZoM=)
![Multivariate-adjusted logistic regression analysis (odds ratio [95 % CI]) of the association between disability with frequency of hospitalization. Multivariate-adjusted logistic regression analysis (odds ratio [95 % CI]) of the association between disability with frequency of hospitalization.](https://static.elsevier.es/multimedia/14133555/0000002900000006/v1_202510310759/S1413355525000838/v1_202510310759/en/main.assets/thumbnail/gr3.jpeg?xkr=ue/ImdikoIMrsJoerZ+w90NRiOl/KnYC22JyCfllZoM=)




