Camptocormia is a trunk flexion occurring during walking that the patient can spontaneously correct in a static position. Therefore, capturing the flexed trunk posture on radiograph is difficult.
ObjectiveTo analyze the interrater reliability in different positions reflecting the dynamic phenomenon of camptocormia using a non-invasive visual three-dimensional capture tool.
MethodsSample size calculation was at least 31 participants. 34 patients who had camptocormia and were monitored in our clinical practice were included. Two different examiners performed measurements using SAM3D tool in the three following positions: Spontaneous Standing Position (SSP), Upright Standing Position (USP), and Walking-like Standing Position (WSP). Sagittal parameters were measured: arrow in C7, kyphosis, lordosis, and knee flexion. The interrater reliability was assessed using Lin's Concordance Correlation Coefficient (CCC).
ResultsRegarding the arrow in C7, the Lin's CCCs were excellent, respectively 0.96 (SSP), 0.98 (USP), and 0.97 (WSP). All the CCCs for other parameters were at least fairly good (>0.87). There were significant differences in arrows in C7 between USP and the two other positions (SSP and WSP).
ConclusionSAM3D is a non-invasive visual three-dimensional capture tool allowing safe and automatic assessments, and repeated measurements with good interrater reliability.
Camptocormia or “bent spine syndrome” is an involuntary, non-fixed, flexion of the thoracolumbar spine when standing, walking, or sitting, which is partially or completely reduced in the supine position or by straightening effort.1–4 Etiologies of camptocormia are multiple,5–8 but its frequency is particularly high in cases of Parkinsonism9–13 with a prevalence estimated between 3 % and 17.6 % of Parkinson's patients according to the studies and definition used.14–18 Camptocormia can lead to disabilities such as reduced walking speed, increased risk of falling,1,19–21 or low back pain.22–24 Nonsurgical treatments can include physical therapy and brace, but the efficacy of these methods requires more evidence.8
There is no consensus for camptocormia diagnosis and no standardized measurements for this dynamic process in a clinical setting. Recording of the dynamic forward flexion during walking requires a kinematic system.25,26 A visual perception of the forward trunk flexion when walking may be used but it remains subjective. A standardized approach involves static radiological measurements, which partially reflects the dynamic phenomenon of camptocormia.25–28 For instance, radiographic explorations including EOS system are widely used to measure the spinal sagittal balance despite this static approach. However, the reproducibility of these results, particularly for sagittal vertical axis, depends on the precise postural instructions when imaging is performed.29,30 This could induce variability in the measurements of the sagittal parameters. A better approach to explore this dynamic phenomenon is to consider the trunk inclination in 3 conditions: (i) upright standing position, (ii) spontaneous standing position, and (iii) during walking.25,26 However, no tools are available in routine clinical practice; therefore, there is still a lack in standardized assessment of camptocormia in everyday practice for physicians in orthopedics, neurology, and rehabilitation.
We hypothesized that a non-invasive visual three-dimensional capture tool could provide relevant information about trunk inclination for automatic assessment of camptocormia in everyday practice. We aimed to analyze the interrater reliability of trunk inclination measurements in patients with camptocormia, in three positions, using a non-invasive visual three-dimensional capture tool (SAM3D) and to compare these measurements to the ones obtained by EOS system.
MethodsStudy designThis methodological study explored patients included between January 2020 and September 2020 in a local cohort and was approved by local ethics committee of the University Hospital of Bordeaux (CEREBDX 2021 – 31). Every patient gave a written consent in accordance with the Declaration of Helsinki. This study followed the GRRAS guidelines.
PopulationPatients monitored for camptocormia in the orthopedic medical unit of the University Hospital of Bordeaux by a physician specialized in spinal disorders, were proposed for inclusion.
Inclusion criteria were: (i) aged more than 18 years-old and (ii) presenting with camptocormia according to usual clinical criteria8 (some degrees of forward flexion of trunk during walking that disappeared in the recumbent position), and (iii) having a recent (<15days) EOS examination performed in ambulatory care.
Exclusion criteria were: (i) inability to stand or walk three minutes without the help of another person or mobility equipment and (ii) refusal to participate in the study or inability to sign written consent.
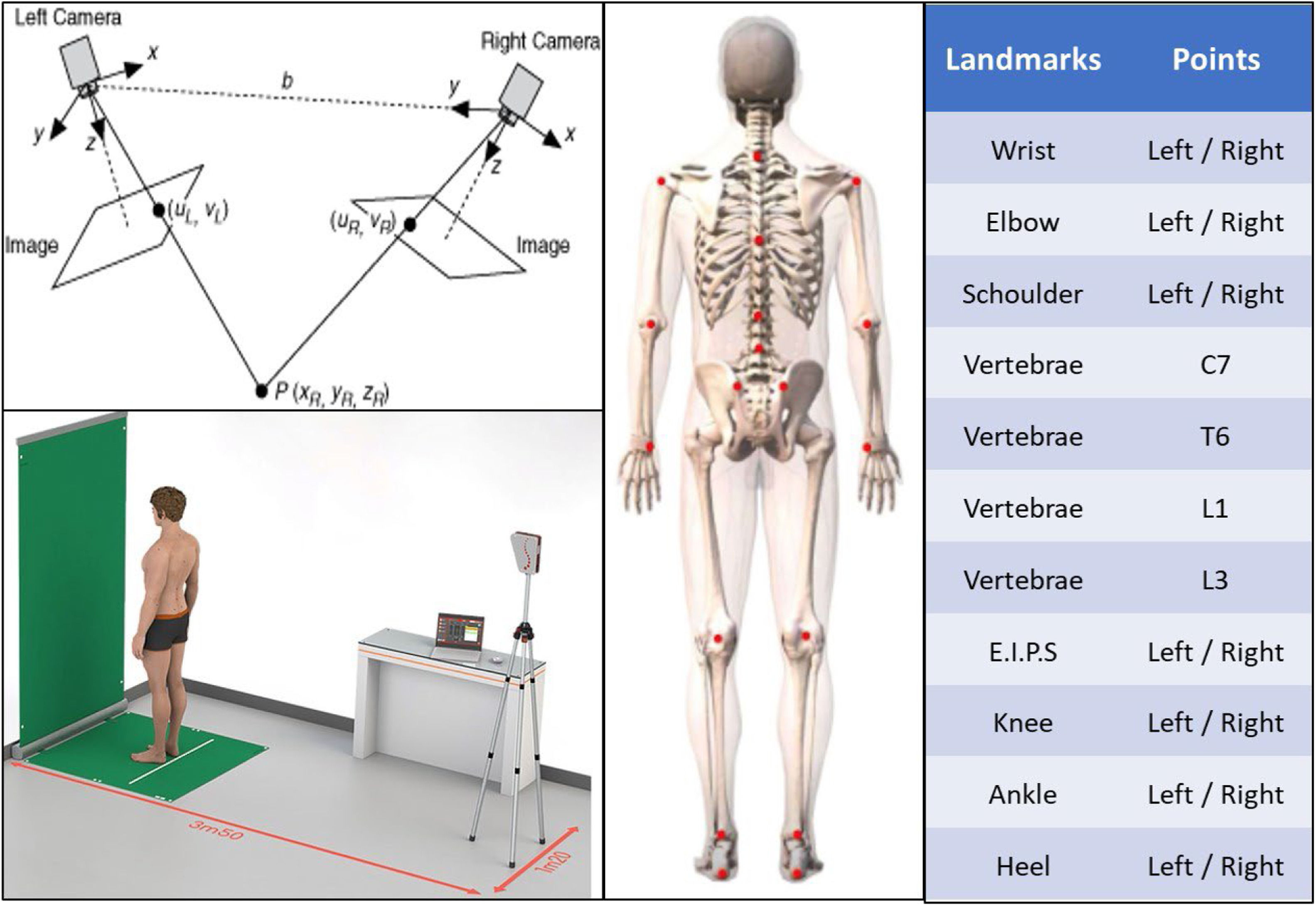
The 3D morphological analysis system (SAM3D®)SAMD3D is a non-invasive and non-irradiating measuring tool. It has been developed by the company SAM Research, which allows performing postural assessments in 3 dimensions. The SAM3D device is a mechano-optical assembly coupled with a specific software producing image acquisitions in 3D. The function of 3D reconstruction is a standard model using the fundamental triangulation principle of any 3D reconstruction from images described by Fig. 1.
The acquisition system includes two high-definition image sensors (4K CMOS, 14MP, 40ms exposure time, 1mm accuracy), coupled with the “back-side-illumination” technology, a roll-up (120cm x 200cm), and a floor plate (120cm x 120cm). The two cameras are fixed one above the other 10cm apart, allowing optimal precision/distance performance. The synchronization of the two images captured by the cameras is directly ensured by the software.
Automatic detection was performed on anatomical landmarks indicated by the operator. Landmarks include a total of 18 points distributed on the back, which reflects the inflexion points of the spine, including the wrists and heels (Fig. 1).
A complete stereo camera calibration is realized during the installation of the system SAM3D.31,32 A daily-basis check was done on background task to verify if the camera intrinsic and extrinsic had changed. With the visual landmarks of which the ground-truth are known, the system can auto-calibrate its extrinsic parameters. A well calibrated SAM3D camera has a reprojection error of 0.2 pixel and the 3D reconstruction RMSE (root-mean-square error) are estimated as 0.35 mm on the X axis and 0.61 mm on the Y axis, and the depth error on the Z axis is 0.87 mm.
ProcedureFirst, the patients were asked to undress to their underwear and remain barefoot. Then, the examiner used a dermal pen to label the 18 predefined anatomical landmark points that would enable the automatic detection to establish a 3D topography after image processing. The subject was positioned about 3.5m from the image sensor (Fig. 1). Because a scoliosis is often associated with camptocormia, the measurements were performed in 3 dimensions: (i) the frontal plane, (ii) the sagittal plane, and (ii) the transverse plane. SAM3D allows reconstruction of axes and selected anatomical segments.
In our study, we decided to explore the following sagittal parameters:
- -
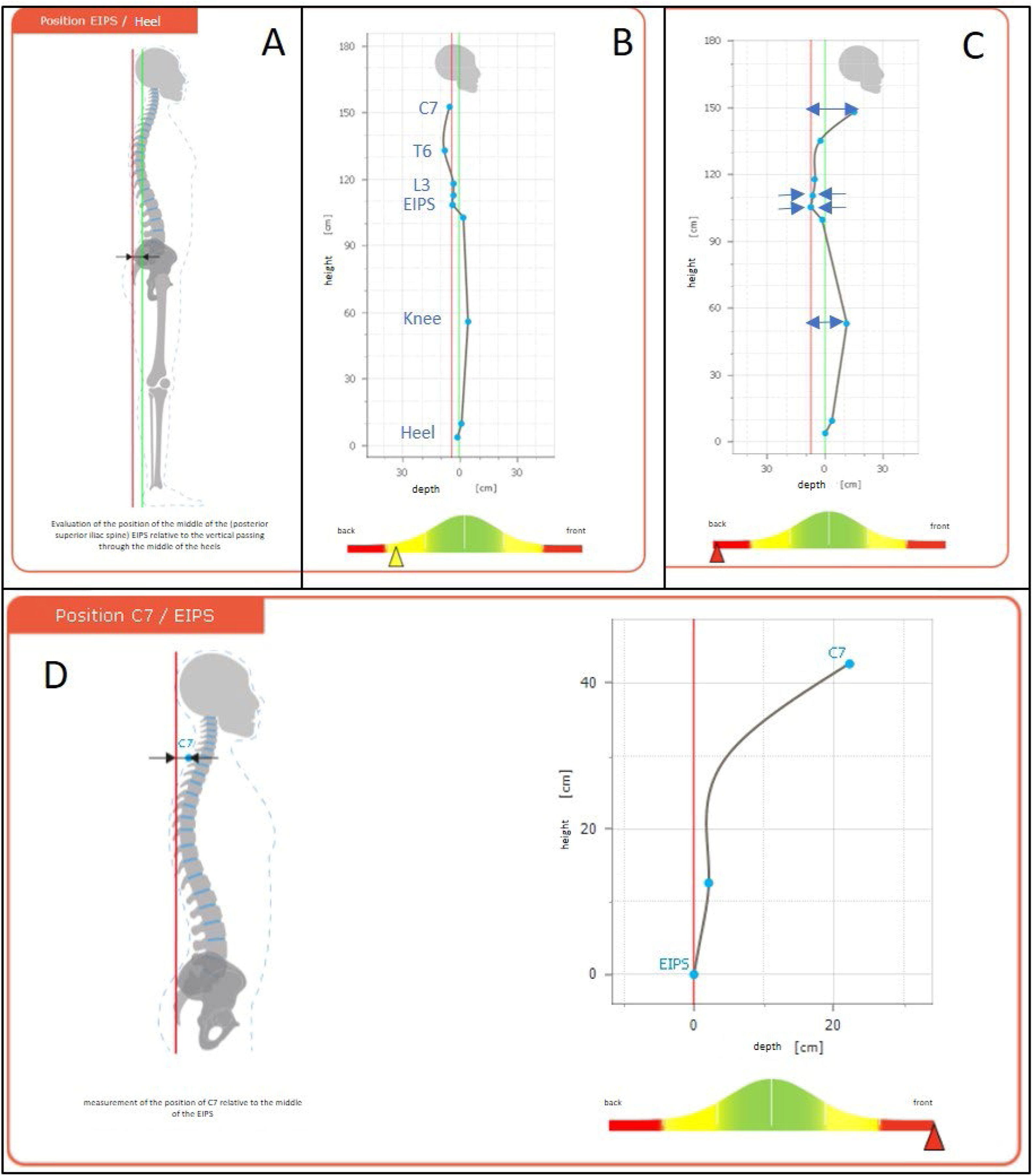
The cervical arrow in C7 (mm) to quantify trunk forward flexion in unit of length. This is the distance between the 2 vertical lines, the first passing through the spinous process of C7 and the second through the middle of the postero-superior iliac spines (PSISs) segment (Fig. 2).
- -
The angles of kyphosis and lordosis: Kyphosis and lordosis were calculated based on the tangent of the inflection points of the spine curves in the cervico-thoracic and thoraco-lumbar areas (Table 1).
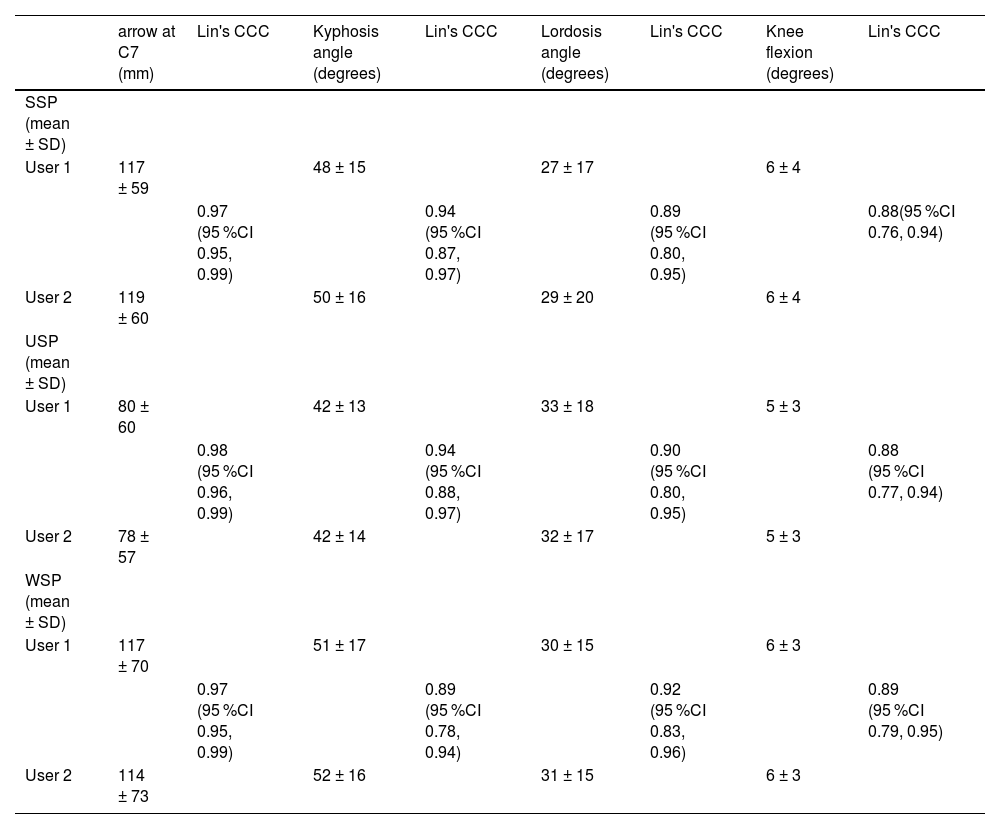
Table 1.Average measurement of the arrow at C7 made by SAM 3D.
PSISs, postero-superior iliac spines; SD, standard deviation; SSP, spontaneous standing position; USP, upright standing position; WSP, walking- like position;
- -
The leg inclination: the angle between the vertical and the segment “posterior edge of the calcaneum – posterior edge of the popliteal fossae” which shows knee flexion (Fig. 2).
The measurements were performed in the 3 best positions reflecting the dynamic phenomenon of camptocormia: (i) Spontaneous Standing Position (SSP) (defined by the spontaneous standing of the patient without instruction), (ii) Upright Standing Position (USP) (defined by the standing position when the patient was asked to be as straightened as possible), and (iii) Walking-like Standing Position (WSP) (asking the patient not to stand up straight after a short walk inducing trunk inclination).
Two separate operators, trained physicians in rehabilitation medicine, blinded to each other, applied and removed dermal landmarks then acquired the images in all 3 positions after explaining and showing each position to the patient. One out of the rater was familiarized with the tool when the other was naïve and never used SAM3D before the study. The completed time for the acquisition of the 3 positions’ images per patient took less than 5 minutes, including for the application and removal of the landmarks. From each acquisition, a 3D model from the selected axes and anatomical segments was reconstructed after thorough validation of the automatic anatomical landmark locations by the operator. Then the different parameters were computed automatically.
The Sagittal vertical axis (SVA) using EOS system was collected to put into perspective SAM3D results with those from a radiographic gold standard. These data resulted from an out-patient clinical routine examination (less than 15 days), thus the EOS procedure was not controlled.
Statistical analysisSample calculation: at least 31 patients for Lin's CCC > 0.81 and expected at 0.92 with a power of 0.80. The interrater reliability of measurements has been assessed by the Lin's Concordance Correlation Coefficient (CCC).33
According to Partik and al,34 a CCC between 0.51–0.60 is considered to be poor, between 0.61–0.70 slight, between 0.71–0.80 moderate, between 0.81 - 0.91 fairly good, between 0.91–0.95 very good, and >0.95 excellent. To explore changes between the 3 positions, we analyzed the measurements of the arrow in C7, and performed ANOVA with repeated measures and contrasts. We also explored the reliability (Lin's CCC) between arrow in C7 obtained by the SAM3D system in the 3 positions for each examiner and C7-SVA using EOS system. A p-value < 0.05 was considered significant.
Results34 patients (19 women) were included in this study, mean age 71 years (SD 7.7). Camptocormia-related etiologies were: Parkinson Disease (11), idiopathic/undetermined (7), degenerative spine (7), spine surgery (2), Lewy body disease (2), multiple system atrophy (1), neuroleptic-induced parkinsonism (1), undetermined myopathy (1), Pompe disease (1), osteoporotic vertebral collapse (1).
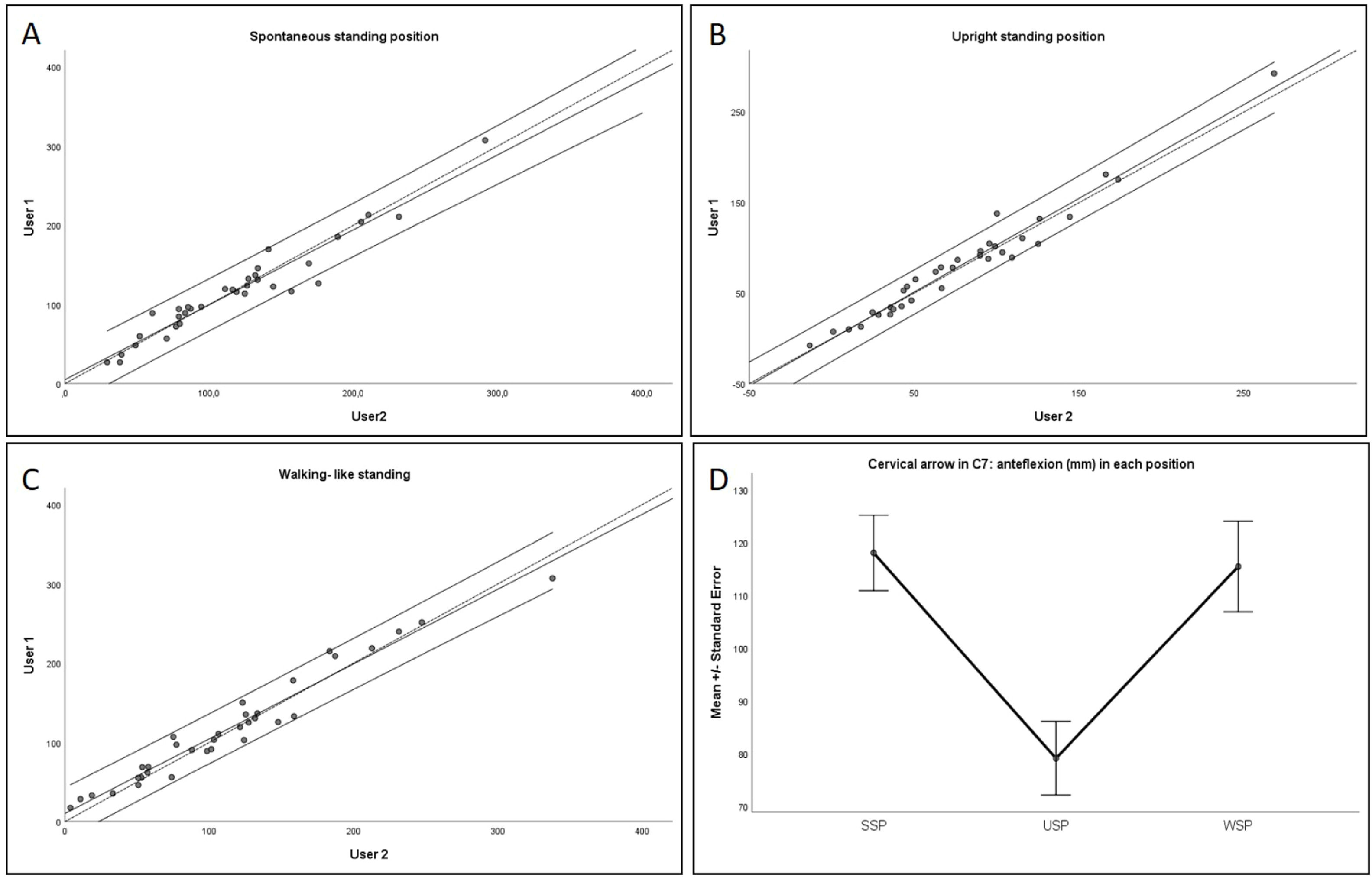
A good interrater reliability was noted for the measurement of the arrow in C7 and Lin's CCC was excellent for the 3 positions: SSP = 0.97 (95 % confidence interval [CI] 0.95, 0.99); USP = 0.98 (95 % CI 0.96, 0.99); WSP = 0.97 (95 % CI 0.95, 0.99) (Fig. 3). Fig. 3A-C show a small dispersion between the 2 users in the 3 positions. Table 1 shows the mean of all measurements by the 2 operators for the 3 positions and the Lin's CCC.
The means of the arrow at C7 was 118 mm (SD = 59) in SSP, 79 mm (SD = 58) in USP, and 115 mm (SD = 71) in WSP. A significant difference was noted between USP and the 2 other positions (F(2, 134) = 54.287, p < 0.001) and no significant difference was noted between SSP and WSP (F(67) = 0.432, p = 0.513) (Fig. 3D).
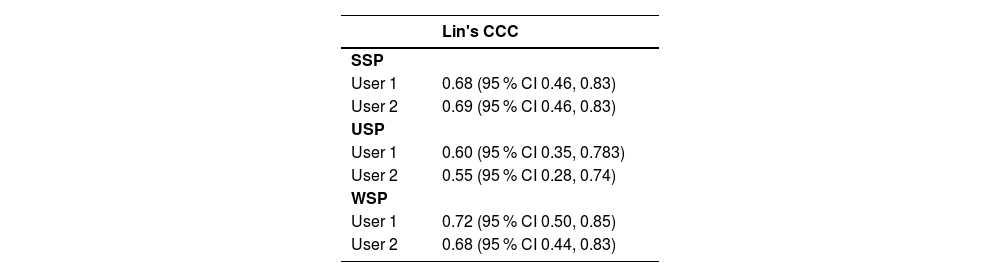
Regarding the measurements of the C7-SVA obtained by EOS system in a clinical routine, the mean for our patients was 102 mm (SD = 76). Reliability between these measurements and those obtained by SAM3D was globally slight (Table 2)
All data are available on request.
DiscussionThe aim of this study was to analyze the interrater reliability of trunk inclination measurement in patients with camptocormia. This was assessed using three conditions aiming to reflect the three kinematic conditions previously described by using a non-invasive visual three-dimensional capture tool (SAM3D). All the measurements by SAM3D had an excellent interrater reliability in the three positions.
There were significant differences between USP and the two other conditions (SSP and WSP), however no differences have been noticed between SSP and WSP. This result suggests that two positions should be distinguished: upright25 and a natural position. Walking does not seem to change anything in this natural static position measured by SAM3D. Indeed, this tool was unable to capture the worsening of trunk forward flexion during walking described by kinematic analysis.25,26 The present study reports also measurement reflecting the knee flexion, known to participate to the compensation in sagittal imbalance.35 Such a measurement is also reproducible.
SAM3D is an optical system allowing safe and automatic assessments, and repeated measurements. These repeated assessments are useful for the management of conservative treatments, such as braces. These treatments are initially aiming to limit the forward collapse of the trunk in natural standing posture and during walking,36–39 but they need to be frequently adjusted for the best correction. Radiographs or EOS do not allow such repeated assessment contrary to SAM3D, but are useful for long term follow-up.
Some factors such as the level of training in each device, the nature of the actions required by the rater for the measurement in each device can affect the reliability. Our results show good inter-rater reliability even if one out of the two raters was naïve from this tool and confirm that SAM3D does not require specific and long training.
Several limitations should be taken into account. First, our sample is small but the sample calculation for a fairly good or better CCC was 31 participants. Moreover, the reliability of the device SAM3D should be considered: the estimated precision, based on repeatability measurements (50 pairs of images) was less than a millimeter (3D reconstruction error mean X: 0.58mm [SD 0.25]; Y: 1.04mm [SD 0.29]; Z: 1.43mm [SD 0.39]). In addition, measurements of the C7 arrow using SAM3D were slightly reliable to the SVA obtained in EOS. Because the standardization of postural instructions given to the patients are known to be crucial to avoid variability of EOS measurements,29,30 the absence of such standardization in a clinical routine in this study can explain the slight reliability. Hence, the reliability was not explored regarding other usual radiographic parameters. Such comparison with radiography was not our first objective, and would require standardized and simultaneous examination, not performed here. Due to this limitation, we only explored SVA and not all sagittal parameters from the radiographs. Such a longitudinal study should be performed in the future.
ConclusionThis study showed good interrater reliability of measurements of trunk inclination in different positions using a non-invasive visual three-dimensional capture tool (SAM3D) in patients with Camptocormia, aiming to reflect the dynamic phenomenon, and underlying that this kind of device could provide relevant information about trunk inclination for automatic assessment of camptocormia in everyday practice.
The authors declare no competing interest.
DI MASCIO Gérard from the SAM research company who lent the SAM3D tool. No funding was received for this work.