Newborns (NB) undergoing invasive mechanical ventilation (IMV) should be extubated as early as possible. Predictive factors for successful extubation are often considered in isolation, focusing on personal factors and the functions and structures of the NB's body, according to the International Classification of Functioning, Disability and Health (ICF).
ObjectivesTo assess the contribution of ICF components to the successful extubation of NB.
MethodA multicenter, observational and retrospective study was conducted using medical records of NB from five macroregions of Brazil. NB who underwent IMV of >24 h were included. Clinical and sociodemographic variables were organized according to ICF components, and factors associated with successful extubation were analyzed using a generalized linear model.
ResultsA total of 498 NB were included, with an extubation success rate of 82.3 %. The body functions and structures component included pH (p = 0.006), the environmental factors component included the number of prenatal consultations (p = 0.002) and mode of ventilation (p = 0.004), and the personal factors component included gestational age (p < 0.001), birth weight (p < 0.001), gestational age at extubation (p < 0.001), and weight at extubation (p < 0.001). Environmental factors increased the probability of successful extubation by 1.72 times (95 % CI: 1.26, 2.35).
ConclusionThe environmental factors component of the ICF significantly influenced extubation outcomes in NB, increasing the probability of success. These findings highlight the importance of developing extubation protocols that integrate predictive variables from all ICF components, considering both functional and structural alterations along with contextual factors.
With scientific advances, the training of health professionals, and the evolution of equipment and resources, it has become possible to offer essential and specialized care that has contributed to increasing the survival of newborns (NB).1,2 This specialized care often begins in the Neonatal Intensive Care Unit (NICU), a therapeutic environment suitable for the treatment of high-risk NB.3,4 Among the life support resources used in NICU, invasive mechanical ventilation (IMV) is indicated in cases of lung immaturity and the need for respiratory support.5,6
Despite its benefits, prolonged use of IMV is associated with significant risks, such as increased complications, morbidities, and longer hospital stays.5,7–10 To minimize these adverse effects, early extubation is recommended once the NB demonstrates the ability to breathe spontaneously and maintain gas exchange within normal parameters.11,12 However, there is no consensus in the literature on well-defined criteria for performing extubation or predicting the success of this procedure.
Successful extubation is defined as the ability of the NB to remain stable without requiring reintubation within a predetermined period.12–14 Several studies have aimed to identify predictive factors for successful extubation by evaluating them individually to determine the optimal timing for IMV withdrawal.11,15 However, these studies, primarily focused on personal factors and on the body functions and structures of NB,11,15,16 as described in the components of the International Classification of Functioning, Disability and Health (ICF), without considering other sociodemographic variables classified as environmental factors.17
The ICF provides a multidimensional and dynamic framework for organizing information in neonatal care, encompassing body functions and structures, activity and participation, as well as environmental and personal factors.17 Rather than serving as a direct assessment tool, the ICF helps guide systematic clinical reasoning by shifting the focus toward the infant’s overall functional abilities and the interplay of various contextual factors.18,19 In NICU, emerging evidence suggests that using the ICF to classify and analyze risk can support interdisciplinary collaboration and more holistic care.20 However, despite their relevance, ICF-based approaches in neonatology have only been explored to a limited extent, likely due to the complex and rapidly evolving nature of this specialty in Brazil, the increased vulnerability of this population, and the logistical challenges of integrating research into clinical practice.19 Thus far, no studies have systematically investigated factors predictive of extubation success in NB under an ICF-oriented framework. Addressing this gap could aid in identifying predictors of successful extubation, ultimately leading to more comprehensive, family-centered interventions.21 We hypothesize that systematically organizing clinical data according to the ICF may clarify which variables are most influential in NB extubation outcomes and foster a more collaborative, patient-centered approach to neonatal respiratory care.
MethodType of studyThis is a multicenter, observational, cross-sectional, and retrospective study, approved by the Human Research Ethics Committee of Universidade do Estado de Santa Catarina (CAAE 36371320.5.1001.0118) and by the internal committees of the participating hospitals and maternity hospitals.
ParticipantsNB who received IMV for at least 24 h during their hospitalization in the participating NICU between 2017 and 2019 were included. The selected period of hospitalization refers to the last years before the Covid-19 pandemic.
NB who had been discharged or transferred to another facility with IMV support and whose medical records were therefore incomplete were excluded.
Data collection proceduresData were collected from the medical records of NB admitted to NICU in six Brazilian cities, representing the five macroregions. A designated professional from each NICU, selected for convenience and proximity to the researchers, completed a standardized form with NB data. Ventilatory and gasometric parameters were recorded at least 24 h before the first extubation, and extubation failure was defined within 48 h.
Due to the multicenter nature of this study, some data were not routinely documented in the medical records of certain centers. Therefore, these unrecorded variables were reported as ‘not registered’ in the tables.
Sample calculationA total annual estimate of 1540 hospitalizations was established, based on information obtained from each center, and a conservative proportion rate of 0.5. Thus, adopting a critical value for the degree of confidence of 95 % (Z〈/2 = 1.96), a margin of error of 3 % (∑= 0.03) and a possible loss of data of 15 %,22 the sample calculation obtained was 498 NB, distributed by random proportional stratification by center.
VariablesThe variables included in the data collection form were selected following a literature search that identified pre-extubation assessment elements that could influence outcome, with maternal, neonatal, ventilatory, and gasometric data prior to extubation related to the extubation process and NICU service. This form was reviewed by specialist physical therapists who agreed on the final format for recording.
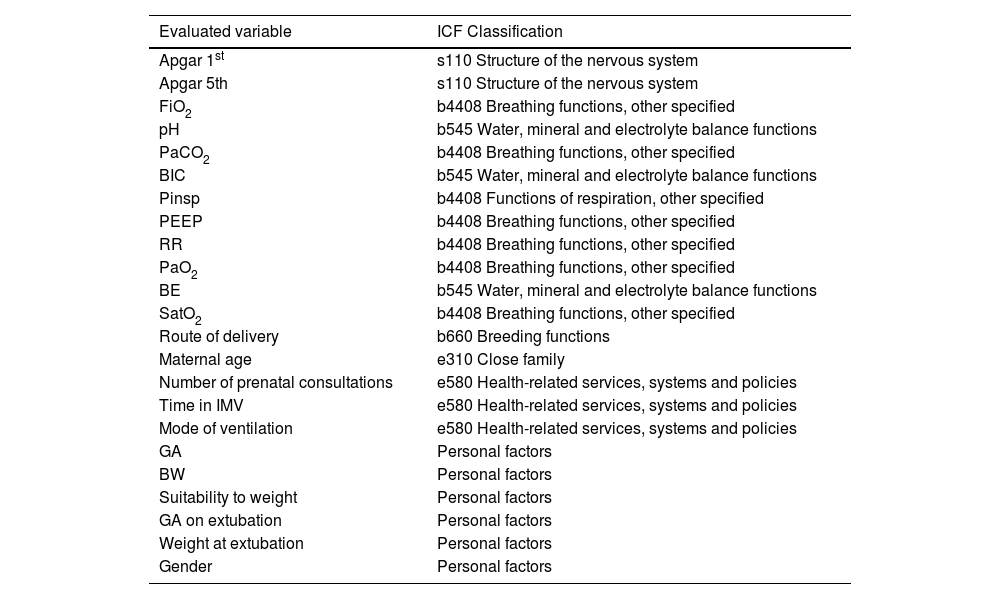
Concordance and linkage of variables with the ICFTo match and link the variables recorded on the form with the ICF components, a table was created in the Office Excel® program and forwarded to two independent evaluators. Each rater cataloged the meaningful concepts related to the items required for extubation and then categorized and described the respective items based on the components of body structures (s), body functions (b), environmental factors (e), and personal factors and their corresponding coding.17,23 The level of agreement calculated using he Kappa coefficient (Statistical Package for the Social Sciences – SPSS® 23.0) was 0.854. In case of inconsistencies in the classification, a third rater reviewed the work and clarified existing differences. The instruments were linked to the ICF according to the rules proposed by Cieza et al.24 The classifications are described in Table 1.
Variable evaluated, ICF classification, and relationship with extubation success.
ICF, International Classification of Functioning, Disability and Health; s, body structure; b, body functions; e, environmental factors; FiO2, inspired fraction of oxygen; pH, hydrogen potential; PaCO2, partial pressure of carbon dioxide; BIC, bicarbonate; Pinsp, inspiratory pressure; PEEP, positive pressure at end of expiration; RR, respiratory rate; PaCO2, partial pressure of oxygen, SatO2, Oxygen saturation; IMV, invasive mechanical ventilation; GA, gestational age.
The data were tabulated and saved in the program Office Excel® and analyzed with the software Statistical Package for the Social Sciences – SPSS® 23.0 and JASP 0.18.3.0. The variables were analyzed descriptively, using the absolute (n) and relative ( %) frequency, as well as the mean value and the 95 % confidence interval of the mean value.
The analyses of the association of the variables with extubation success were performed using biserial correlation tests per point and chi-square test, according to their characteristics.22 The variables structured the three components of the ICF, i.e., body functions and structures, environmental factors, and personal factors. To condense the information of the variables of each component of the ICF to a smaller dimension, the Principal Component Analysis (PCA) was performed. This multivariate analysis technique transforms an original set of variables into a reduced number of components that explain most of the variance in the data. Although it was developed for quantitative data, Kalantan & Alqahtani25 have demonstrated its use for mixed data. This analysis provides coefficients that represent the weighting of each variable in each component. Thus, using the coefficients of the principal components (PC), an index was created for each component of the ICF. To determine the goodness of fit of the model and the number of PC, the criterion that at least 80 % of the data variability was found was established.
A generalized linear model was used to investigate how the components of the ICF of body functions and structures, environmental factors, and personal factors influence the outcome of extubation. In this modeling, the logit linkage function and the binomial distribution probability were used. The predictive factors determined in the logistic regression were expressed as odds ratios (OR) with their respective 95 % confidence intervals (95 % CI). Missing data reported as 'not registered' in the tables were treated as 'missing-at-random' and the pairwise deletion procedure was used in the analyzes.26 The significance level applied was 5 %.
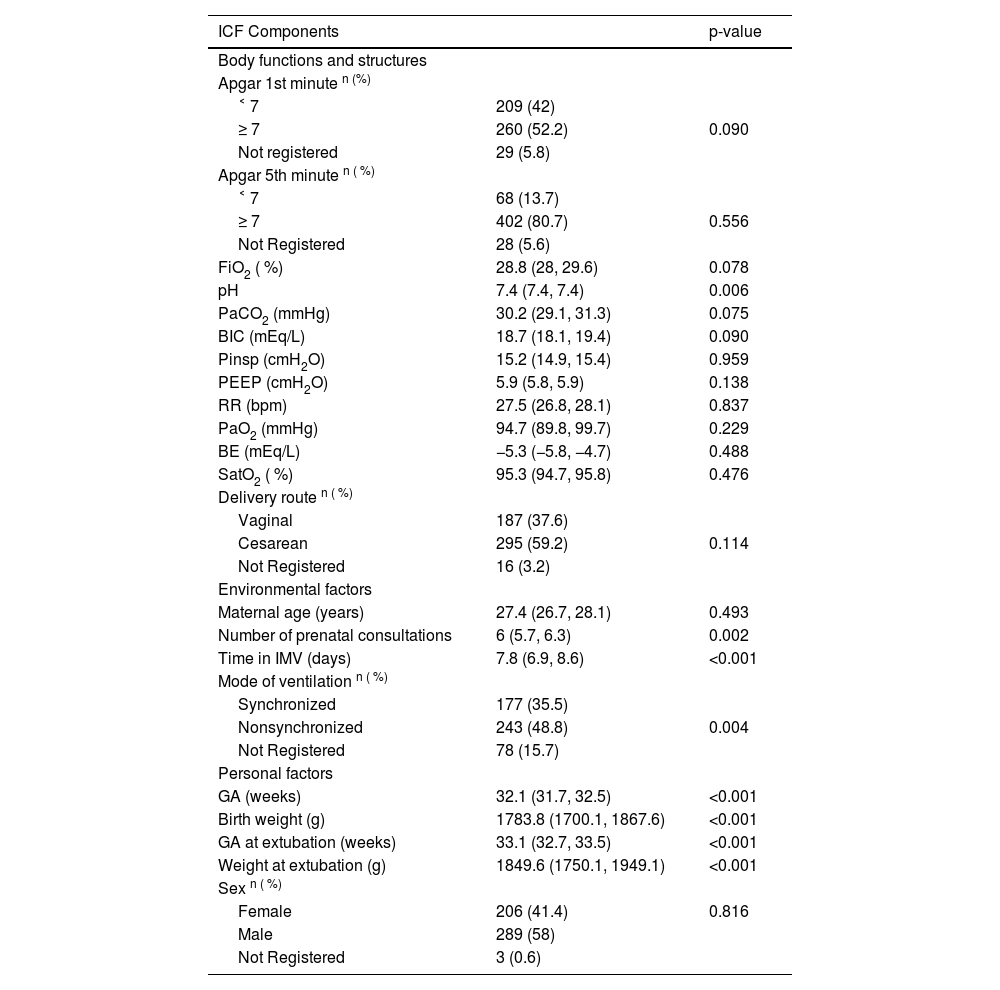
ResultsThe medical data of 516 NB were collected. After reviewing the data, 18 NB were excluded because they had remained in the IMV for <24 h. There were a total of 498 NB, of which 135 (27.11 %) were from two cities in the South, 108 (21.69 %) were from one city in the Southeast, 102 (20.48 %) were from one city in the Midwest, 97 (19.48 %) were from one city in the Northeast and 56 (11.24 %) were from one city in the North. Of the NB, 410 (82.3 %) were successfully extubated and 88 (17.7 %) required a return to IMV within 48 h. The profile of the NB and the association between the variables and successful extubation were organized according to the ICF components and are described in Table 2.
Profile of NB and association of variables with successful extubation.
Data are mean and 95 % confidence interval of the mean unless otherwise indicated.
n ( %), absolute and relative frequency; ICF, International Classification of Functioning, Disability and Health; FiO2, fraction of inspired oxygen; pH, hydrogen potential; PaCO2, partial pressure of carbon dioxide; BIC, bicarbonate; Pinsp: inspiratory pressure; PEEP, positive end-expiratory pressure; RR, respiratory rate; PaCO2, partial pressure of oxygen, SatO2, Oxygen saturation; IMV, invasive mechanical ventilation; GA, gestational age; g, grams.
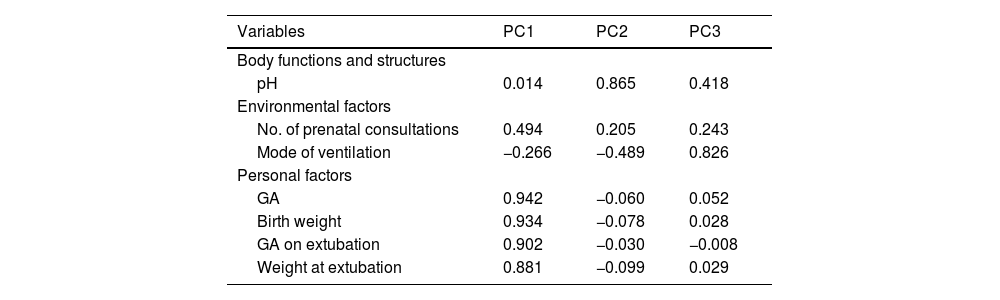
Three components from the PCA were required to explain 80.5 % of the variance, 52.3 % from component 1 (PC1), 15.0 % from component 2 (PC2), and 13.2 % from component 3 (PC3). The factor loadings and weights assigned to each variable in each component of the PCA are shown in Table 3.
Factor loadings of each component of the principal component analysis.
PC, principal components; GA, gestational age; pH, hydrogen potential.
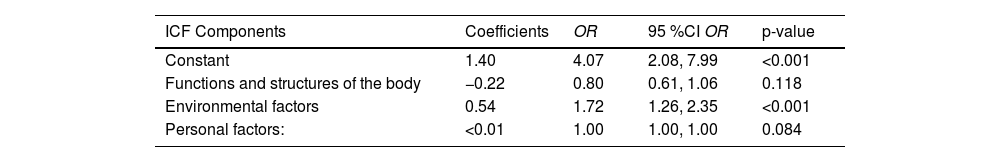
Based on the factor loadings, the scores that defined each of the ICF components were obtained by multiplying the factor loadings by the value of each person variable. Multivariate association analysis using a generalized linear model showed that only the ICF component of environmental factors was significantly associated with the outcome of extubation, contributing to a 1.72-fold increase in the probability of success, as shown in Table 4.
Multivariate association analysis between ICF component scores and extubation success.
OR, odds ratio; 95 % CI, 95 % confidence intervals.
The aim of this study was to assess the contribution of ICF components to successful extubation of NB. Multivariate association analysis revealed that only the environmental factors component was associated with successful outcome (95 %CI: 1.26, 2.35). In the overall analysis, the variables number of prenatal consultations and mode of ventilation can contribute to a 1.72-fold increase in the probability of success. Thus, the importance of knowledge of the environmental factors by the health professionals responsible for this care can be emphasized, because the greater the probability of success, the lower the complications in NB.11
The other associations between the ICF components of body function and structure and personal factors were not significant, although in this and previous studies, variables such as pH, GA, birth weight, GA at extubation, and weight at extubation considered in isolation were predictive of extubation failure in NB.11 Of the 498 NB, 82.3 % had a successful extubation outcome, confirming the findings of Jurkevicz et al. and Carvalho et al., in which the frequency of successful extubation outweighed that of failed extubation.13,27
The rate of failed extubation increases the lower the GA of the NB.11 In this study, extubation failure and the need to return to IMV in <48 h was observed in 17.7 % of the NB. Fu et al.11 found that the incidence of failure at first extubation was 26.5 % and the time interval to characterize failure varied from 48 h to 7 days. In light of this, there is a need for standardization between health services and studies regarding the time considered as failure at extubation, whereby the consensus of this outcome would affect the reproducibility and reliability of the studies.11
Maternal age, number of prenatal consultations, mode of delivery, time on IMV, and mode of ventilation were organized in the ICF component of environmental factors. In isolation, the variables associated with extubation success were number of prenatal consultations (p = 0.002) and mode of ventilation (p = 0.004). Regarding the number of prenatal consultations, the average of six consultations found is consistent with the recommendations of the World Health Organization and the Brazilian Ministry of Health.28 In national population-based studies, the majority of Brazilian women have more than six prenatal consultations, showing that the level of care is considered to be high in all regions of the country, regardless of demographic, social, or reproductive characteristics.29,30 The adequate number of prenatal consultations in the population of this study, which correlates with successful extubation, reflects the need for maternal follow-up during pregnancy and consequently the reduction of neonatal morbidity and mortality.31
In this study, 48.8 % of the NB received nonsynchronized ventilation, while 35.5 % received synchronized ventilation. Synchronized ventilation is associated with a lower risk of air leaks and a reduction in IMV time compared to nonsynchronized ventilation, making it the preferred approach for NB.10,32 However, despite these benefits, a substantial proportion of NB in this study received nonsynchronized ventilation. This finding could be due to different institutional protocols, availability of equipment, or clinical preferences of the NICU teams in different institutions.33 In addition, 15.7 % of the records lacked information on the mode of ventilation, which is a limitation and a potential source of bias. These missing data could indicate inconsistencies in documentation between centers. To mitigate this limitation, the authors treated the missing data as the condition of missing-at-random using the pairwise deletion procedure.26 Future studies should investigate the underlying reasons for these differences in mode of ventilation and their impact on clinical outcomes.
Apgar score at the 1st and 5th minute, fraction of inspired oxygen, hydrogen potential (pH), partial pressure of carbon dioxide and bicarbonate were organized in the ICF component of body functions and structures. In isolation, only pH was associated with extubation success (p = 0.006). The NB had an average pH of 7.4, which is within the normal range.34,35 This value is similar to that found when characterizing the profile of the NB in the study by Costa et al.16 It is considered that a pH in the normal range indicates success, confirming the relationship found in this study, and that the opposite, when lower, in cases of persistent acidosis (pH<7.20 - 7.25), indicates the need for reintubation.11,12 In general, the decision to extubate depends on clinical judgment through interpretation of ventilatory support, gasometry, and overall clinical stability of the NB.11,36
Gender, GA, birth weight, GA at extubation, and weight at extubation were organized into the ICF component of personal factors. In isolation, the variables associated with successful extubation were GA (p < 0.001), birth weight (p < 0.001), GA at extubation (p < 0.001), and weight at extubation (p < 0.001). The mean GA of the NB in this study was 32.1 weeks and the mean GA at extubation was 33.1 weeks. In confirmation of these findings, GA is known to be a significant predictor variable for extubation outcome, with higher GA being associated with success11,37 due to greater brain maturation and consequent improvement in respiratory control and regulation.38 Spaggiari et al. state that the risk of extubation failure decreases by 27 % with each additional week of GA, which is clinically significant and should be considered at the time of extubation.37
The NB had an average birth weight of 1783.8 g, classified as low birth weight,39 and an average extubation weight of 1849.6 g. These values are similar to those found when characterizing the profile of NB in the study by Costa et al.; however, in that study the predictive factors for the outcome of extubation failure were determined.16 In addition, the study by Giaccone et al. suggests that the observation window for the need for reintubation should be increased in NB with a birth weight of <1000 g, as the failure rate increases with a longer observation window in these NB.12
In light of the above, the scientific basis for determining NB extubation readiness is still imprecise and the factors assessed are often based on clinical judgment, professional experience, and blood gas analysis.11 This fact leads to considerable variation in hospital practice, especially in a large and heterogeneous country such as Brazil, where the lack of standardized protocols makes it difficult to systematically manage the components of the pre-extubation process.11 The results of this study emphasize the need to develop a protocol that comprehensively integrates the factors and variables that predict successful extubation, taking into account all components of the ICF and considering functional and structural changes associated with contextual factors.
Among the limitations of this study, we highlight the sample loss during data collection and gaps in the completion of medical records. To mitigate potential biases and errors related to sample size, missing data were treated under the condition of missing-at-random.26 It is necessary to emphasize the importance of complete and accurate documentation in maternal and neonatal medical records, as well as the integration of this information. For future multicenter studies, we recommend rigorous standardization of data collection procedures across institutions with different routines. Additionally, prospective studies can provide complementary insights by enabling the simultaneous recording of relevant variables during the initiation and discontinuation of IMV, facilitating a more comprehensive assessment of the predictors of extubation success or failure.
ConclusionThe environmental factors component of the ICF, represented by the variables number of prenatal consultations and mode of ventilation, had a positive influence on the outcome of extubation of NB, helping to increase the probability of success.
None to declare.
This work was carried out with the support and financial assistance of the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Funding Code 001, a Brazilian government entity focused on training human resources. This study was also funded by the Fundação de Amparo à Pesquisa e Inovação do Estado de Santa Catarina (FAPESC), through Public Call No. 05/2019 – Master's Scholarship Program. Additionally, we acknowledge the support of the Conselho Nacional de Desenvolvimento Científico e Tecnológico – CNPq (National Council for Scientific and Technological Development).