Exercise training is essential in pulmonary rehabilitation (PR) for individuals with chronic obstructive pulmonary disease (COPD). In Brazil, physical therapists typically deliver exercise in PR. This document presents ASSOBRAFIR recommendations for prescribing exercise training for patients with COPD.
ObjectiveTo provide evidence-based recommendations for structuring exercise training programs for people with COPD.
MethodsThe guideline panel followed the Guidelines International Network (GIN) principles and the Appraisal of Guidelines for Research & Evaluation (AGREE-II) to ensure methodological rigor. The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach was employed to assess the certainty of evidence (CoE). This method assessed evidence quality and developed recommendations for five key questions addressing aspects of exercise training for people with stable COPD. Treatment effects were evaluated using systematic reviews and meta-analyses.
ResultsThe following conditional recommendations were drawn: 1. Combined exercise training (aerobic + resistance) is suggested over aerobic training alone (very-low CoE); 2. No suggestion for or against adding inspiratory muscle training, non-invasive ventilation, or supplemental oxygen to combined exercise training (moderate to very-low CoE); 3. Either interval or continuous training is suggested, with no preference for partitioned or nonlinear training (moderate to very-low CoE); 4. Maintenance exercise programs are suggested as an alternative to usual care after PR (very-low CoE); 5. Minimal resource exercise training, especially with elastic resistance, or conventional exercise training is suggested (very-low CoE).
ConclusionThe results of the present guideline can aid clinicians in structuring exercise training for people with COPD.
Exercise training has long been recognized as the cornerstone of pulmonary rehabilitation (PR) programs for people living with chronic obstructive pulmonary disease (COPD).1,2 Despite this, various trials report individuals who do not respond to the intervention.3–5 Over the past two decades, many studies have explored strategies to optimize training responses.6,7 Common strategies include combining exercise modalities (e.g., aerobic and resistance training) and adding other interventions ("add-ons") such as oxygen supplementation, non-invasive ventilation (NIV), and inspiratory muscle training (IMT). Additionally, studies have focused on various exercise delivery methods for people with COPD, including interval, partitioned, and non-linear training. The variability in protocols and outcomes across different clinical trials presents a significant challenge for clinicians in determining the most appropriate strategy to adopt.
Current evidence in PR reports that fewer than five percent of eligible individuals are enrolled in PR programs.8 To improve access, exercise modalities using minimal equipment have emerged as a low-cost alternative.9 Another challenge in PR is the duration of programs. Recommendations suggest that at least eight weeks are necessary for patients to experience physiological gains in musculoskeletal function, with greater benefits in longer programs.2 However, longer programs tend to be more costly and may reduce the equity of the intervention. Moreover, the current available recommendations are not either supporting or opposing the use of maintenance programs after PR programs.10 The latter, however, did not limit trials of at least eight weeks of exercise training.
In Brazil, the availability of PR centers is not fully known, but reports indicate a scarcity and uneven distribution across the country. An editorial published in 2017 estimated around 150 PR centers in Brazil,11 while a 2018 study in Latin America identified 124 PR centers, corresponding to only 0.05 centers per 100,000 inhabitants.12 Additionally, access to these programs is primarily restricted to large urban areas, limiting their reach. Many challenges remain in enhancing the delivery of PR. This evidence-based guideline aims to provide recommendations to help clinicians deliver exercise training, the key component of PR, to patients with COPD, considering locally available resources and logistics. The goal is to improve accessibility, optimize resource use, and ensure high-quality care, addressing the current scarcity and uneven distribution of PR centers, especially in underserved areas.
Five key questions regarding exercise delivery methods, duration, and required equipment were addressed to evaluate the benefits of different exercise protocols for people with COPD.
MethodsProtocol and enrollmentThis clinical practice guideline was developed following the Appraisal of Guidelines for Research & Evaluation (AGREE-II) recommendation and the principles outlined by the Institute of Medicine and the Guideline International Network.13,14 The guideline panel used the Grading of Recommendations Assessment Development and Evaluation (GRADE) approach to appraise evidence quality along with the Evidence to Decision (EtD) Framework to formulate recommendations.15 The proposal to write the ASSOBRAFIR Clinical Practice Guidelines in Respiratory Physical Therapy was endorsed by the ASSOBRAFIR General Executive Board.
Eligibility criteriaThis guideline specifically addresses exercise training for people with COPD. It does not apply to other chronic lung diseases. Studies comparing interventions to placebo, sham, or no intervention were excluded, as pulmonary rehabilitation is already a well-established therapy for COPD. This approach is supported by the Cochrane review by McCarthy et al.16 and the editorial by Lacasse,17 both of which concluded that additional trials on the efficacy of pulmonary rehabilitation in COPD are unnecessary.
The task force developed five PICO questions (wherein P: population, I: intervention, C: comparison, and O: outcome). The guideline panel prioritized these questions based on their relevance to the Brazilian context and their importance for clinical decision-making using GRADE methodology on a scale from 1 to 9, with categories including ‘critical’ (7–9), ‘important’ (4–6), or ‘of limited importance’ (1–3), based on their relative significance to patients. A list of potentially relevant outcomes for each PICO question was created. The five PICO questions used the same keywords for the “P”, thus, the definition of COPD was the same to all questions. Detailed methods are provided in the Supplementary Materials.
Stakeholder involvementThe guidelines were developed by 43 professionals, including the ASSOBRAFIR general executive board, a management committee, a panel of eight voting members, a methodology team, and an executive committee. The board, management committee, and methodologists did not interfere with the systematic review or recommendations. The executive committee consisted of 25 professionals selected through a public process, focusing on experts in systematic reviews and meta-analyses. The panel included physical therapists, university professors, and researchers. No patients were directly involved in the present recommendations. Whenever applicable, the panelists reported the patients' preferences and values (upon direct consultation to patients) in the recommendations. The guidelines are intended for physical therapists responsible for exercise prescription in patients with COPD. The Supplementary Material includes a list of all participants, their roles, and declarations of potential conflicts of interest.
Approach to evidence review and selectionSystematic reviews for each PICO question used the Covidence platform, with all stages (screening and extraction) conducted in duplicate, as were the RoB2 and Note assessments.18 The search strategy included defining PICO questions, keywords, sources, and the time range in the literature. Electronic databases used were Medline, CENTRAL, EMBASE, BVS/LILACS, Web of Science, Scopus, along with hand-searched journals and conference abstract reviews. Only randomized clinical trials in English were included. Additionally, systematic reviews on related topics were also screened and appraised for quality using the AMSTAR-2 checklist. Only reviews rated as medium to high quality were considered for inclusion.19
Evidence summaries and formulation of recommendationsThe methodological team created evidence summaries for each PICO, including effect estimates and quality ratings. In two online meetings, the panel used the EtD20 to formulate recommendations, reaching consensus on their direction, strength, and any observations. Disagreements required at least 80 % panel approval for recommendations.
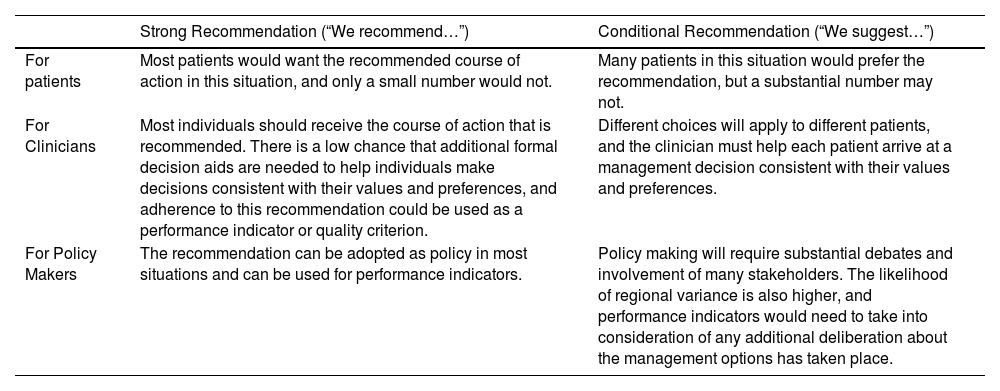
Interpretation of strong and conditional recommendationsThe recommendations were labeled as either “strong” or “conditional” according to the GRADE approach.20 The expressions “the guideline panel recommends” were used for strong recommendations, and “the guideline panel suggests” for conditional recommendations. Table 1 provides the suggested interpretation of strong and conditional recommendations by patients, clinicians, and healthcare policymakers. The accompanying remarks clarify each recommendation, balancing health benefits and harms to provide effective guidance for exercise training in COPD while minimizing potential risks and maximizing patient well-being.
Implications of strong and conditional recommendations: from the grading of recommendations, assessment, development and evaluation working group.
Following the generation of recommendations, the panel was divided into working groups for each PICO question and provided a narrative summary of the evidence and issues raised in the EtD, if any. The panel agreed on the final draft of all recommendations.
Document reviewThe ASSOBRAFIR Scientific Board and the General Coordination of Scientific Documents reviewed the manuscript before submission for peer review and publication.
Dissemination and implementation toolThe dissemination will be implemented during ASSOBRAFIR local, regional, and national events, as well as through social media and monitoring via Altimetric®. These events will also serve as consultation forums for implementing the guidelines, with numbers reported in the following meetings for monitoring and auditing purposes.
Editorial independenceThe manuscript was written by the guideline panel in accordance with AGREE-II and GRADE recommendations. It was prepared following the submission guidelines of the Brazilian Journal of Physical Therapy and underwent an independent evaluation process, including external peer review.
Funding and updatingThe ASSOBRAFIR General Executive Board covered all the expenses associated with the current guideline and facilitated the involvement of its members, with no industry participation. All authors disclosed potential conflicts of interest, including financial, intellectual, and personal conflicts. ASSOBRAFIR will reassess the guideline in three years to determine whether an update is necessary.
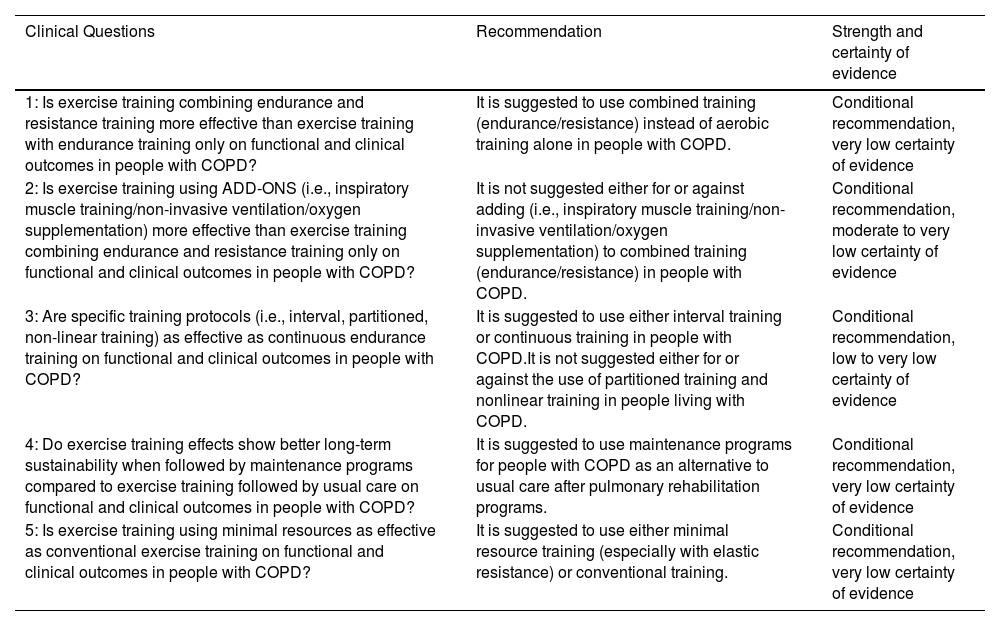
ResultsSystematic reviews were conducted for each PICO question using standard methodology.21 As recent systematic reviews on the investigated PICO questions exist,22,23 the data from those reviews were used to provide the recommendations in the current clinical guideline. Quality appraisal of the reviews was done using the AMSTAR-2 checklist.19Table 2 summarizes the recommendations. The Supplemental Materials provide detailed information on the evidence supporting each recommendation.
Summary of key recommendations.
The guideline panel suggests using combined training (endurance/resistance) instead of aerobic training alone in people with COPD (conditional recommendation, very low certainty of evidence [CoE]).
Summary of the evidenceA total of nine studies were used for the final analysis. Details from exercise prescription for resistance and aerobic training are described in Table S1 of the Supplemental Materials. The effects on exercise tolerance were similar in both modalities for peak oxygen uptake (peak VO2) from cardiopulmonary exercise test (four studies involving 98 participants, standardized mean difference (SMD) of 0.14 [95 % confidence interval (CI) −0.44, 0.72]; and walking tests (five studies, involving 105 participants, SMD of 0.01 [−0.38, 0.39; 95 %CI]). Likewise, there were no significant differences between the two modalities for health-related quality of life (HRQoL) assessed through questionnaires (three studies, 73 participants, SMD of 0.28 [−0.39, 0.96; 95 %CI]). Additional benefits of the combined intervention were observed for lower limb muscle strength (nine studies, 183 participants, SMD of 1.0 [0.56, 1.43; 95 % CI]), symptoms using the SGRQ (one study, 24 participants, mean difference (MD) of −14.5 [−33.21, 4.21; 95 % CI]) and, dyspnea using the MRC scale (three studies, 74 participants, MD of 0.47 [0.27, 0.67; 95 % CI]). Effects on body composition were reported and described in the supplemental materials.
JustificationThe panel voted for a conditional recommendation in favor of the intervention, considering the very low overall CoE. Desirable effects were evaluated as moderate to large, while undesirable effects were deemed trivial. The suggestion by the guideline panel was established due to the observed improvements in several functional and clinical outcomes for individuals with COPD.
Other criteria and implementation considerationsThe outcomes had similar results between the two modalities, except for improvements in lower limb muscle strength and dyspnea, which were better in the group receiving both types of exercise training. Additionally, combined therapy is well accepted by people with COPD and can be beneficial if resources are available in rehabilitation centers. The panel recommends that clinicians should aim for high intensity aerobic exercise (i.e. >60 % maximal work rate or a BORG fatigue and dyspnea scores between 4 and 6) and resistance exercise commencing with loads equivalent to 60–70 % of 1RM.2
Recommendation 2The guideline panel does not suggest either for or against adding (i.e., IMT/NIV/oxygen supplementation) to combined training (endurance/resistance) in people with COPD (conditional recommendation, moderate to very low CoE).
Summary of the evidenceFour studies examining the effects of combined exercise training (i.e., aerobic + resistance training) with additional therapies were included for the final analysis: IMT (three studies), NIV plus supplemental oxygen (one study), and supplemental oxygen alone (one study). The effects of adding IMT to the combined intervention were not superior for the exercise tolerance (i.e., 6MWT) (three studies involving 240 patients, MD 20.42 m, −9.40, 50.24; 95 % CI), dyspnea (2 studies using different tools, 214 patients, not possible to run meta-analysis) and HRQoL, maximum expiratory pressure (MEP), or forced expiratory volume in the first second (FEV1) found in one study each (Supplementary Material). A meta-analysis of three RCTs indicated that IMT alongside combined exercise training might increase inspiratory muscle strength, as represented by maximal inspiratory pressure (MIP) (MD 9.48cmH2O, 2.78, 16.17; 95 % CI), but not exceeding the MID for the outcome (17.2cmH2O). The evidence was of very low certainty for the influence of supplemental oxygen and NIV plus supplemental oxygen as adjunct therapies to combined exercise training, with only one trial (21 participants) identified. This study found no difference in exercise capacity (6MWT, ISWT, and ESWT), respiratory muscle strength, quality of life, or rate of perceived effort (Borg dyspnea) when comparing exercise training with or without additional therapies.
JustificationThe panel voted for a conditional recommendation for the interventions, considering the moderate to very low overall CoE. Desirable effects were evaluated as “don’t know”, while undesirable effects were deemed trivial. The guideline panel suggestion was based on the very low certainty of evidence from the few available studies, which showed no significant or clinically important differences for most outcomes, regardless of the add-on therapy.
Other EtD criteria and implementation considerationsThe evidence for IMT included 87 % of individuals with inspiratory muscle weakness (MIP <60 cmH2O or <70 % of predicted). Despite the very limited evidence for NIV and supplemental oxygen (only one small study for each), it is important to note that patient and therapist acceptance of NIV may vary. Additionally, it is not clear which patients might benefit from supplemental oxygen. A more conservative approach might involve ceasing exercise if peripheral oxygen saturation falls below 85 % or 88 % and considering oxygen use based on the local context.24 The panel agreed that the three therapies investigated entail varying costs, ranging from moderate to high, which could impact equity.
Recommendation 3The guideline panel suggests using either interval training or continuous training in people with COPD. It is not suggested either for or against the use of partitioned training and nonlinear training in people living with COPD (conditional recommendation, moderate to very low CoE).
Summary of the evidenceEleven studies examining the effects of interval training (eight studies), non-linear training (two studies), and partitioned training (one study) were included. The effects of interval training were not superior to continuous training regarding dyspnea (one study using mMRC scale and involving 42 patients) or health-related quality of life reported by the Chronic Respiratory Questionnaire (CRQ) (two studies, 101 patients). Likewise, similar results were found in the two interventions for exercise tolerance (eight studies including 263 patients) in various outcomes (peak power output, Watts), peak VO2, peak ventilation, peak heart rate (HR), lactate threshold, 6MWD, and endurance time (i.e., duration of cycling at 80 % of the peak workload). Nonlinear training improved endurance time more than continuous training (MD = 359.95 s; [261.69, 458.21 s; 95 % CI]). None of the trials comparing continuous and interval, partitioned or non-linear training included in the present meta-analysis reported data about balance, functional performance, activities of daily living, peripheral or inspiratory muscle strength and endurance, body composition, physical activity level, self-management, and self-efficacy.
JustificationThe panel voted for a conditional recommendation for the interventions, considering the moderate to very low overall CoE. Desirable effects were evaluated as trivial (interval training) or “don’t know” (partitioned and non-linear training), while undesirable effects were deemed trivial for all three interventions. The guideline panel suggestion for either continuous or interval training was based on the similar effects of both modalities in people with COPD. The panel was unable to recommend for or against the use of partitioned and non-linear training for people with COPD as there is a paucity of available information (particularly randomized clinical trials) to provide a recommendation in this field.
Other EtD criteria and implementation considerationsCurrent evidence cannot assure that specific training protocols increase equity in rehabilitation services, and studies have not reported undesirable effects for any of the three alternative protocols. Interval training is well tolerated by people with COPD, but there are no data on patient acceptability for partitioned and non-linear protocols. All three protocols are feasible for clinical practice, requiring only a cycle ergometer, unlike treadmills, which pose a fall risk. However, insufficient expertise makes partitioned and non-linear training less accepted by professionals. Therefore, physical therapists must be trained on these protocols' objectives, applicability, and benefits. Interval, partitioned, and non-linear training require a cyclical-based program, making unsupervised performance potentially unfeasible, though this has not been tested.
Recommendation 4The guideline panel suggests using maintenance programs for people with COPD as an alternative to usual care after pulmonary rehabilitation programs (conditional recommendation, very low CoE).
Summary of the evidenceExercise capacity was assessed using the 6MWT (nine studies1-9) and the ESWT and ISWT (two studies). Maintenance programs may result in small but significant differences in exercise capacity measured by the 6MWT at 6 months (MD 22.6 m; 95 % CI [6.1, 39.1 m]), 9 months (MD 33.8 m; 95 % CI [13.8, 53.8 m]), and 12 months (MD 32.6 m; 95 % CI [0.4, 64.8 m]). No differences in ESWT and ISWT performance were observed between the maintenance and usual care groups. HRQoL was assessed using the SGRQ in two studies, with no differences between groups in total scores or domains at 6 and 12 months. Two studies reported HRQoL using the CRDQ at 12 months and found no significant differences between groups across all domains. Dyspnea (mMRC), physical activity in daily life, functional performance, and peripheral muscle strength were reported in a few studies, but the data were insufficient for reasonable effect estimates, preventing any recommendations.
JustificationThe panel voted for a conditional recommendation for the intervention, considering the very low overall CoE. Desirable effects were evaluated as small while undesirable effects were deemed as “don’t know”. The guideline suggestion was based on improving exercise capacity, while no additional effect on quality of life was found. Given the long-term nature of maintenance interventions, evidence is generally limited by imprecision; however, these results are consistent with other systematic reviews.25–27
Other EtD criteria and implementation considerationsMaintenance training programs may involve additional costs depending on the chosen protocol. Evidence is limited regarding ideal maintenance program components, such as supervision frequency, required infrastructure, and method of delivery (in-person or remote). Professionals should weigh in on the best way to conduct maintenance, as it will likely affect participants' acceptability, feasibility, and equity.
Recommendation 5The guideline panel suggests using minimal resource exercise training (especially with elastic resistance) in people with COPD as an alternative to conventional training (conditional recommendation, very low CoE).
Summary of the evidenceSix studies compared resistance training using elastic tubes or bands with weight machines. Only one study compared aerobic training modalities: ground walk versus cycle ergometer training. Four studies involving 133 patients investigated exercise capacity using the 6MWT, ISWT, ESWT, incremental cycle, and endurance cycle tests. Except for the ESWT (based on one study involving 32 patients), which showed a significant difference in favor of minimal equipment (MD 301 s; 95 % CI [45.14, 556.86]), none of the other tests showed differences between interventions. Three studies involving 85 patients investigated differences using the CRDQ. There were no differences in the domains of the questionnaire, but there was a significant difference in the CRDQ total score (based on one study involving 32 patients) in favor of minimal equipment (MD 15 points; 95 % CI [3.99, 26.01]). No differences were found between the interventions for peripheral muscle strength (three RCTs, n = 101), dyspnea (one RCT, n = 38), and physical activity levels (one RCT, n = 48). The complete set of results can be seen in the online supplement.
JustificationThe guideline panel suggestion was based on very few studies, with very low certainty of evidence of no significant or clinically important difference for the majority of outcomes. Due to the limited available evidence of other interventions, the decision was based on studies evaluating only elastic tubes or bands as minimal interventions, limiting the recommendation based on other minimal resources.
Other EtD criteria and implementation considerationsTraining with minimal resources, can be considered an alternative to conventional training for people with COPD. It brings similar effects and is well tolerated by patients. However, the panel emphasizes the importance of ensuring supervision and maintaining the same volume of physical training. Additionally, minimal equipment training programs can be performed in domestic environments and community spaces, potentially increasing adherence to pulmonary rehabilitation, especially for individuals with reduced mobility or those from disadvantaged socioeconomic backgrounds. The panel agrees that minimal resource training with elastic components is viable for clinical practice due to its lower cost, accessibility, and potential to enhance equity in access to physical training programs.
DiscussionIn this Clinical Practice Guideline (CPG), we provide recommendations for exercise training programs for people living with COPD based on five PICO questions. Although this document does not cover all the relevant questions regarding exercise prescription and delivery in PR, the panel understands that these questions tackle at least in part the most frequent topics in PR for Brazilian physical therapists.
The first recommendation investigated the superiority of adding resistance training to aerobic modality. The meta-analysis found that this association significantly improved lower limb strength and symptoms more than aerobic training alone, but it did not provide additional benefits for exercise capacity and health-related quality of life. This aligns with previous guidelines recommending a combination of aerobic and resistance training.2,10,28 The task force emphasizes that both aerobic exercises alone and combined with resistance training are effective, yielding similar improvements in most outcomes. The combined approach is particularly beneficial for patients with peripheral muscle weakness and a high burden of symptoms.
Although widely used in clinical practice, there is no strong evidence that additional interventions (i.e., add-ons) enhance the effects of exercise training for the general population of people with COPD.7 In this guideline, only a few studies investigated the addition of IMT, NIV, and oxygen supplementation to exercise training. This was primarily due to strict inclusion criteria, requiring studies to have at least eight weeks of intervention and to include the investigated modality in a combined exercise regimen (aerobic + resistance training). A meta-analysis was only possible for IMT, revealing that even in patients with inspiratory muscle weakness, no additional gains were observed in key rehabilitation outcomes such as exercise capacity or quality of life, confirming the results of a recent systematic review.22 Oxygen supplementation and NIV did not show additional benefits, but the limited evidence prevents any conclusive statements for or against the use of these modalities. The task force believes that a specific group of patients may benefit from these modalities, such as those who cannot reach the intensities of desired physical training caused by dynamic hyperinflation, intense dyspnea, and fatigue of the lower limbs and those experiencing severe oxygen desaturation (<85 %).
Different modalities of exercise were investigated in the present guideline. The task force concluded that interval aerobic training offers similar responses to continuous aerobic training. The ERS/ATS guideline on pulmonary rehabilitation suggests that interval training can be an alternative to standard aerobic training for people with chronic respiratory disease who struggle to reach their target intensity or duration of continuous exercise due to dyspnea, fatigue, or other symptoms.2 Likewise, training partitioning reduces ventilatory demands and, thus, may reduce symptoms during exercise.29 Non-linear training imposes different exercise workloads across the training sessions with varying objectives in each session. Although the latter has the potential to increase exercise performance significantly more than the other two former modalities, the limited evidence precluded the task force from conveying a strong recommendation for or against its use.
There has been an increased interest in studies that investigate ways to maintain the benefits of exercise training. The latest ATS clinical practice guideline in PR suggests that either maintenance programs or usual care after PR can be offered since benefits are small and evidence is limited.10 This cautious recommendation reflects the low certainty of evidence and the absence of consistent effects on health-related quality of life. In contrast, the data from the present guideline encourage the adoption of maintenance programs after PR, as small but significant benefits in exercise tolerance were observed for up to 12 months. Although the certainty of evidence remains low, the panel prioritized the potential for maintaining functional gains, consistent with findings from previous systematic reviews. It is recommended, however, that future studies focus on the ideal frequency and type of supervised maintenance programs, as this remains not well-established in the literature.10,25
Exercise training using minimal equipment may be a suitable alternative where limited availability of expensive equipment exists. In line with the present guideline, a recent systematic review suggests that minimal equipment may improve access to pulmonary rehabilitation worldwide, particularly in rural and remote areas and developing countries.23 This particularly interests the Brazilian population, as rehabilitation centers are scarce and unevenly distributed.12 The task force endorses the use of minimal equipment as it provides similar effects on muscle strength and exercise capacity to center-based programs as an alternative, primarily by reducing the costs of the modality.
Previous evidence from the ATS/ERS already pointed to potential barriers that need to be addressed to ensure equitable access and effective application of the present guideline.8 First, physical therapists must have formal training in the science, process, and benefits of PR. Second, more centers are needed, with a more even distribution nationwide. Finally, it is crucial to raise payer awareness of the benefits of exercise training for people with COPD to increase referrals.
In this guideline, the certainty of evidence for the PICO questions ranged from moderate to very low. This was primarily due to imprecision and risk of bias, and to a lesser extent, inconsistency. The limited number, small sample sizes, and methodological limitations of the available randomized controlled trials are likely the main contributors to these issues. To address these limitations, future studies should ensure adequate sample sizes to reduce imprecision and implement rigorous methodologies to minimize risks of bias, such as deviations from intended interventions, missing outcome data, and measurement errors.
To strengthen the evidence base for future guideline updates, several key research gaps must be addressed. The current findings raise the question of whether a more individualized approach may offer greater benefits to patients. For example, future studies should investigate the effects of combined endurance and strength training compared to endurance training alone, particularly in patients with COPD with peripheral muscle dysfunction, to determine whether the combined approach yields superior outcomes. Additionally, the adjunctive use of supplemental oxygen and noninvasive ventilation during exercise training is currently supported by very limited evidence. Addressing specific limitations such as the lack of clarity on ventilator pressure settings in noninvasive ventilation trials and the absence of cardiovascular overload assessments in oxygen supplementation studies would contribute to a better understanding of appropriate patient selection for these modalities. While exercise training is well established in improving exercise tolerance, future trials should broaden their scope to include outcomes such as physical activity levels, balance, muscle strength, and functional performance. Finally, to support the broader implementation of minimal-resource rehabilitation programs, future research should also evaluate clinical effectiveness, safety, long-term adherence, sustainability, and the impact on health equity, particularly in remote or underserved populations.
Despite following internationally recognized frameworks for guideline development, this guideline has some limitations. Notably, patients were not formally involved in the panel nor systematically consulted during the development process. While panelists occasionally sought input from patients they were acquainted with, this feedback was informal and not standardized. The absence of structured patient engagement may limit the extent to which the recommendations fully reflect patient perspectives and values. Future updates of the guideline should prioritize formal patient inclusion to enhance transparency, relevance, and shared decision-making. Additionally, due to journal formatting constraints, comprehensive methodological details, including search strategies and outcome prioritization, were placed in the Supplementary Material, which may limit immediate accessibility for some readers. Lastly, the level of detail reported in the included studies regarding exercise training progression protocols was inconsistent. While this was considered during the formulation of recommendations, it may influence the interpretability and applicability of the findings. Future trials should aim to provide clear and standardized reporting of progression protocols to support more robust guideline development.
ConclusionThese clinical practice recommendations help clinicians structure exercise training and implement additional therapeutic interventions to help people with COPD. Furthermore, they show that the use of minimal equipment presents results similar to a conventional program, and maintenance programs after completion of a pulmonary rehabilitation program can benefit gains and maintain benefits. Clinicians are encouraged to adopt these recommendations to improve patient outcomes, while researchers are urged to address the evidence gaps to strengthen future guidelines.
The authors declare no competing interests. No external funding influenced the content or recommendations of this guideline, which were developed independently based on current evidence.
The authors thank the Brazilian Association of Respiratory Physiotherapy, Cardiovascular Physiotherapy, and Physiotherapy in Intensive Care (ASSOBRAFIR) for its support in developing this guideline. We also acknowledge the contributions of the guideline committee, external reviewers, and collaborating healthcare professionals.