The Dysfunctional Voiding Score Symptoms (DVSS) questionnaire is commonly used to evaluate dysfunctional voiding and incontinence (DVI).
ObjectivesTo translate and culturally adapt the DVSS questionnaire into Spanish (DVSS-Sp) in pediatric population and to assess its psychometric properties.
MethodsThe process of translation and cultural validation were done. To obtain evidence of validity and reliability, we evaluated the fit of different factor models and calculated internal consistency coefficients. Also, the diagnostic capacity of the DVSS-Sp scale was assessed through a logistic regression analysis and a receiver operating characteristic (ROC) curve. Accordingly, a total sample of 248 participants was recruited (204 with a diagnosis of DVIs and 44 with no medical problems).
ResultsThe cross-cultural adaptation showed an adequate correspondence with the original version. The DVSS-Sp was configured with 2 factors: Overactive Bladder (OB) symptoms (items 1, 2, 6, and 7) and Dysfunctional Elimination (DE) symptoms (items 3, 4, 8, and 9), showing excellent goodness-of-fit indices. The relationship between the factors OB and DE was low. The reliability of the OB factor was α = 0.68, ω = 0.71, and the DE factor was α = 0.56, ω = 0.57. A logistic regression analysis suggests a good diagnostic capacity of the DVSS-Sp scale. Additionally, ROC analysis showed a cut-off score of 3.5 on the DVSS-Sp scale, where the specificity was 0.907, and the sensitivity was 0.636.
ConclusionThe results of this study support the use of the DVSS-Sp for assessing DVIs in Spanish-speaking children.
Dysfunctional voiding and incontinence (DVI) symptoms are prevalent in pediatric population, representing 47% of pediatric consultations.1 They are considered one of the most significant risk factors for developing urinary tract infections and other complications in children (i.e., vesicoureteral reflux).1 The International Children's Continence Society (ICCS) defines DVIs (also known as bladder and bowel dysfunction, BBD) as combining vesical and intestinal symptoms.2 The DVIs are classified into two categories, 1) lower urinary tract dysfunctions with symptoms related to the change in the continence or voiding phase (e.g., incontinence, enuresis, urgencies, difficulty voiding, among others) and 2) bowel dysfunctions (e.g., constipation or encopresis).2
Assessing DVI is traditionally done through clinical screening and complementary examinations such as urine cultures, urodynamics, ultrasounds, magnetic resonance imaging, and uroflowmetry, among others.2 Complementing this, in the last few decades, are Patient-Reported Outcomes Measures (PROMs).3,4
There are currently different PROMs designed to detect DVI symptoms, such as the Dysfunctional Voiding Symptom Score (DVSS),5 the Dysfunctional Voiding and Incontinence Symptoms Score (DVISS),6 and the Incontinence Symptom Index-Pediatric (ISI-P, for children over 11 years) questionnaires.7,8 Since 2016, the ICCS has recommended using the DVSS to assess lower urinary tract symptoms. Consequently, the DVSS has assumed a leading role in the assessment of DVIs.2
The DVSS was designed by Farhat et al. in 2000 for its application in children and adolescents.5 It is widely used in different pediatric studies on patients with voiding dysfunctions, vesicoureteral reflux, association with constipation, nocturnal enuresis, behavioral disorders, and other pathologies.5,9 Consequently, the DVSS has been translated and validated in several languages and populations (i.e., Korean,10 Portuguese,11 Chinese,12 Japanese,13 Serbian,14 Arab,15 and Thai16). Although Spanish is the second-most spoken language in the world by number of native speakers17 the DVSS still does not have a version adapted to this language. In the pediatric population with DVIs, the evaluation of symptoms and treatment results has presented a lack of standardization. This has been partly remedied by the DVSS, because this instrument allows the quantification of clinical symptoms, being of great value both for diagnosis and for estimating the effectiveness of treatment. The non-existence of the DVSS Spanish version significantly limits the analysis of DVI in the Spanish-speaking pediatric population, both in clinical and research settings.
The DVSS has shown good psychometric properties, mainly for reliability,10,11,14,15 and secondarily in its diagnostic capacity, assuming unidimensionality of DVI.7,16 To our knowledge, only one study explicitly analyzed the factor structure of the DVSS.12 In that study, although details of the factor analysis steps are lacking (e.g., estimation method, method of determining the number of factors), at least a 3-factor structure was described. Factor 1 represented Overactive Bladder (OB) symptoms, Factor 2 represented Dysfunctional Elimination (DE) symptoms, and Factor 3 represented Stress and Pain (SP) symptoms when urinating.
This phenomenon is not isolated; it is common to find tests for which adequate scientific integrity have not been published, despite widespread use in hospitals (e.g., Pain Catastrophizing Scale, PCS18). This is paradoxical because estimating reliability for a complete data test is extremely risky when its number of factors is still unknown. What matters is knowing the reliability of each of its factors (i.e., the measurement error of each factor). It should be noted that the application of tests without adequate psychometric properties is not optimal.19
Consequently, this study aimed to culturally adapt the DVSS (DVSS-Sp) questionnaire to Spanish and evaluate its psychometric properties (construct validity, diagnostic capacity, and reliability) in a sample of Chilean children.
MethodProcedureThe study was structured in two stages. The first stage, translation and adaptation of the DVSS to Spanish occurred between December 2019 and December 2020. The second stage analysed the psychometric properties of the DVSS-Sp through a cross-sectional study where the adapted questionnaire was applied to Chilean children with and without (i.e., control) DVI from December 2020 to May 2021.
The legal guardians/carers were informed of the purpose of the study and what participation entailed. Once legal guardians/carers gave their consent and the children gave their assent to participate in the study, age and sex data were collected, and the questionnaire was sent by e-mail to legal guardians/carers of the children to be completed. It should be noted that the study was conducted during the COVID-19 pandemic, so the questionnaire was completed online.
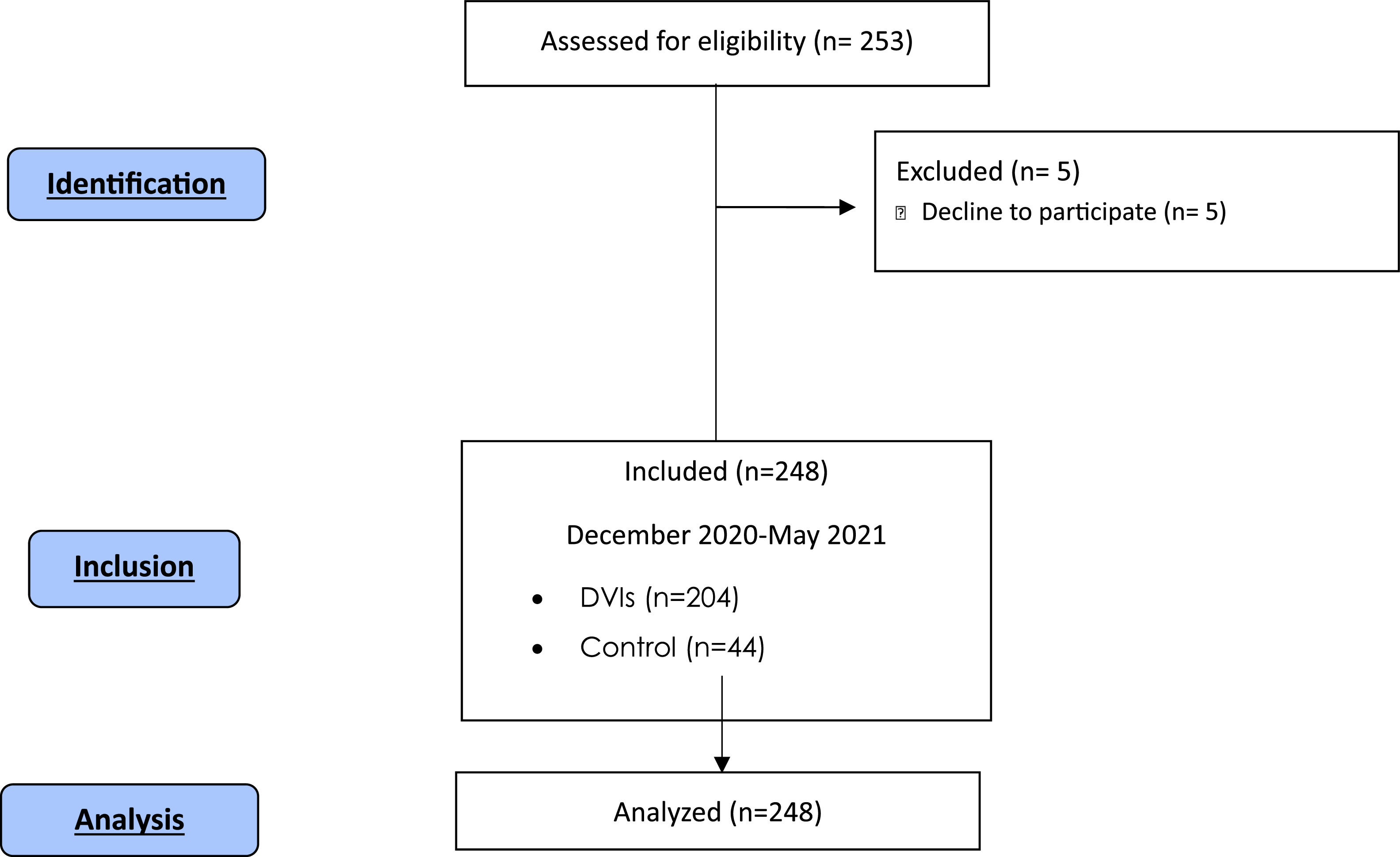
ParticipantsA total sample of 248 participants was recruited (age: 7.9 ± 2.8 years; 72% girls). Of these, 204 participants had a medical diagnosis of DVI (DVI group, age = 8.12 ± 2.87 years; 79% girls) and 44 without medical problems (Control group, age = 6.9 ± 2.2 years; 39% girls). Non-probability consecutive sampling was applied. The participants in the DVI group were recruited from the MATER Children's Renal Corporation Medical Centre located in Santiago, Chile. The participants in the Control group were recruited by online invitation (Fig. 1). The inclusion criteria of the DVI group were children aged between 4 and 17 years, resident in Chile with a medical diagnosis of voiding dysfunction and/or vesico-intestinal dysfunction and providing informed consent. The exclusion criteria were children with a urinary tract infection or pyelonephritis in the last month and neurological problems. In the Control group, the inclusion criteria were children aged between 4 and 17 years with no medical diagnosis of vesical or intestinal disease or dysfunction. This study was approved by the Scientific Ethics Committee of the Scientific Ethical Committee of the South Metropolitan Health Service (Cod. 85–04102019) and took place per the Declaration of Helsinki.19,20
MeasureThe DVSS consists of 10 items (Supplementary online material). The first 9 items describe urinary and intestinal symptoms. These items have the following options on the Likert scale: almost never (0 points), less than half the time (1 point), about half the time (2 points), almost every time (3 points), and not available (0 points). Item 10 examines the domestic stress of the child in the last month and is binary. In particular, it asks about the experience of events such as the arrival of a new baby, a new house, a new school, etc. Any of these events being present scores 3 points, and if none are present, 0 point. The child answers the first 9 questions with their legal guardian or carer, and the tenth question is answered only by a legal guardian or carer. Thus, the scale presents scores that range from 0 to 30. A higher score indicates a greater presence of DVI symptoms. It has been reported that to determine the presence of DVI symptoms in girls, a score of 6 or greater (sensitivity 92%, specificity 87%), and for boys a score of 9 or greater (sensitivity 80%, specificity 91%), is required.5 Another study described the score to determine the presence of DVI symptoms as being 6.66, regardless of sex.12
The development of the Spanish version of the DVSS (DVSS-Sp) followed the adaptation principles of the International Test Commission (ITC).21,22 Two native Chilean translators with advanced knowledge of English (1 lay translator and 1 specialized in the area) translated the original version of the DVSS into Spanish. The two translators and committee agreed on the translation. Later, two lay native English translators who live and understand the language of the Chilean culture back-translated it into English, producing a second agreed-upon version. This last version, in English, was sent to one of the authors of the original questionnaire. Once an author of the DVSS had reviewed this version, it was contrasted with the Spanish version, and the modifications suggested by this author were made. This final version was analyzed by a committee of experts comprised of four specialists in urological disorders in pediatrics (i.e., a doctor and three physical therapists) and a referee with experience in validating scales. This committee considered semantic/idiomatic (i.e., correct translation), cultural (i.e., related to the context and understanding of life for the Chilean population), and conceptual equivalence (i.e., verification of the original concepts of the instrument being maintained in the translated version), creating a final version of the questionnaire in Spanish (Supplementary online material).
Later, a pretest was done with children diagnosed with DVI symptoms. Those responsible for applying this questionnaire were two physical therapists. The objective of this pretest was to test the DVSS-Sp in terms of semantic or grammatical errors, as well as the degree of understanding of the instructions and items. These participants were not included in the analysis of the final study sample. The pilot pretest had 30 children (aged 6.9 ± 2.2 years; 63% girls). Difficulty was recorded only for question 3, for the statement “(extraño defecar) I miss having a bowel movement”. Hence, this was modified to “echo de menos”, which is better understood culturally, which was incorporated into the final version of the DVSS-Sp.
Statistical analysisTo obtain evidence of validity and reliability, we evaluated the fit of different factor models. The proposed models included exploratory factor analysis (EFA), confirmatory factor analysis (CFA), exploratory structural equation modeling (ESEM), and, in the event of measurement artifacts, models with orthogonal method factors. These method factors were modeled using random intercept item factor analysis (RIIFA). It is well-known that ESEM models offer more precise factor estimates, such as loadings and correlations between factors, than CFA. Parallel analysis was used to determine the number of factors to retain. The fit of the factor models was evaluated according to Schreiber's updated recommendations.23 For the reliability analyses, the internal consistency coefficients of each factor were calculated using both Cronbach's Alpha and McDonald's Omega. These reliability indices and their confidence intervals were robustly calculated (i.e., considering their lack of normality). Lastly, to continue providing evidence of the scale's validity, the diagnostic capacity of the DVSS-Sp scale was evaluated through a logistic regression analysis (of the OB and DE factors over the dysfunctional voiding diagnosis) and a ROC curve. All analyses were conducted using IBM SPSS 28, R package coefficientalpha,24 and Mplus 8.8.
Measurement modelsThe proposed models tested the structure of items and factors described in previous literature on the DVSS. Specifically, eight models (M1 to M8) were analyzed. Model M1 proposed a one-factor structure where all symptoms are attributed to a single factor. Model M2 tested the existence of two related factors: Overactive Bladder (OB) symptoms and Difficult Elimination (DE) symptoms. Model M3 expanded on M2 by adding the Stress and Dysuria (SD) symptoms factor described by Chang et al.12 Model M4 proposed an ESEM model for the OB and DE factors. Model M5 introduced an ESEM for all three factors (OB, DE, and SD). Model M6 included a method factor in addition to M1. Model M7 added a method factor to M4. Finally, Model M8 incorporated a method factor into M5. The determination of factors to be retained was evaluated using parallel analysis. All models were programmed using the weighted least squares and adjusted mean and variance (WLSMV) estimator due to the ordered categorical nature of the data.
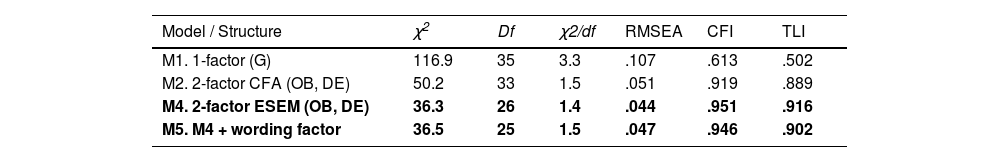
ResultsThe parallel analysis noted two factors and the fit indices for models M1, M2, M4, and M5 are shown in Table 1. The fit indices for the rest of the models are not shown in this table because their analyses did not converge, i.e., the proposed structure of items and factors does not make their calculation possible (e.g., the SD factor specifies only two main indicators, when the presence of three or more indicators are necessary to avoid such estimation problems).
Fit indices of the estimated models of the DVSS-Sp.
| Model / Structure | χ2 | Df | χ2/df | RMSEA | CFI | TLI |
|---|---|---|---|---|---|---|
| M1. 1-factor (G) | 116.9 | 35 | 3.3 | .107 | .613 | .502 |
| M2. 2-factor CFA (OB, DE) | 50.2 | 33 | 1.5 | .051 | .919 | .889 |
| M4. 2-factor ESEM (OB, DE) | 36.3 | 26 | 1.4 | .044 | .951 | .916 |
| M5. M4 + wording factor | 36.5 | 25 | 1.5 | .047 | .946 | .902 |
Note. N = 204 cases; Note. df, degrees of freedom; RMSEA, root mean square error of estimation; CFI, comparative fit index; TLI, Tucker-Lewis Index; G, global; OB, Overactive Bladder symptoms; DE, Difficult Elimination symptoms; In bold, for Chi-squared tests of model fit with p > .05.
Among the models that could be calculated, M4, the 2-factor ESEM structure, produced a good fit, and the best fit, also (e.g., RMSEA < 0.05, CFI > 0.95). M5 had almost the same fit values as M4. Adding a method factor did not substantially improve the fit.
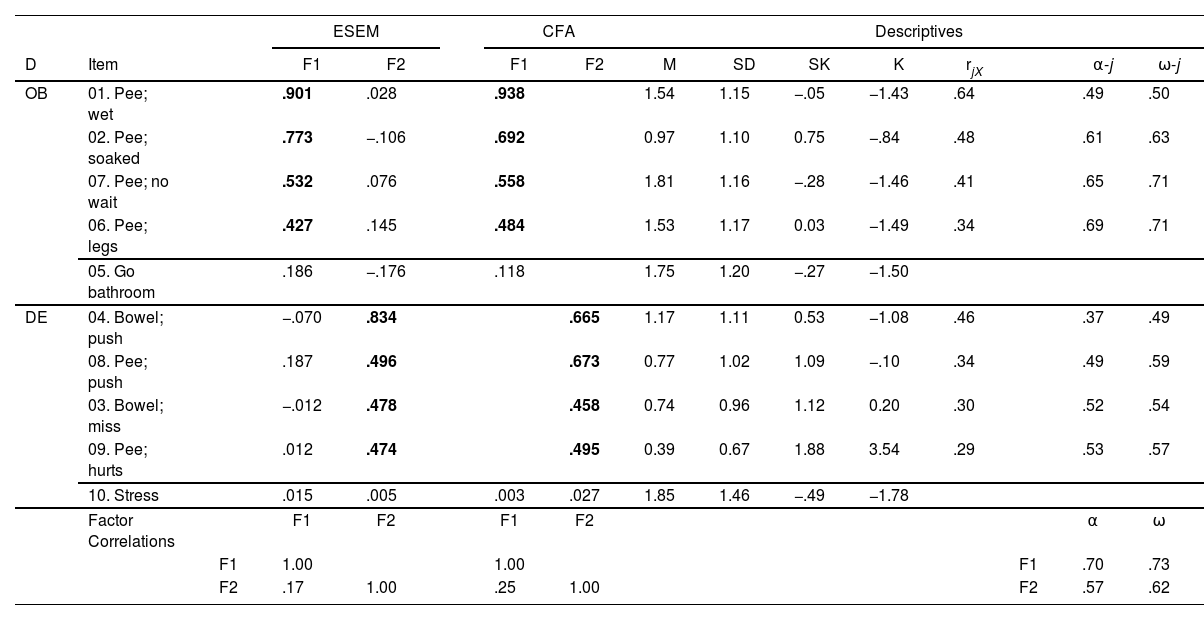
Factor loadings from M2 and M4 are shown in Table 2. Except for items 5 and 10, the rest of the primary loadings were significant (p < .05). All the cross-loadings were small (absolute value < 0.19) and non-significant (p > .05). Although the main loadings were significant, they were mostly below 0.6. Furthermore, it is important to highlight that the relationship of the factors was low (i.e., 0.17 in the ESEM model 4). This suggests the independence of OB and DE symptoms.
Solutions for the Two-Factor ESEM and CFA models of the DVSS-Sp.
Note. N = 204 cases; D, theoretical dimension; F, factor; OB, Overactive Bladder; DE, Difficult Elimination; rjX , j-rest correlation; α, Cronbach's α; ω, McDonald ω; α-j, α if j dropped; ω-j, ω if j dropped; bold factor loadings, p < .05.
The reliability of the OB factor was at the limit of what can be considered adequate: α = 0.70, 95% CI [.62, .77], and ω = 0.73, 95% CI [.67, .78]. However, the reliability of the DE factor was not adequate: α = 0.57, 95% CI [.47, .64], ω = 0.62, 95% CI [.51, .75].
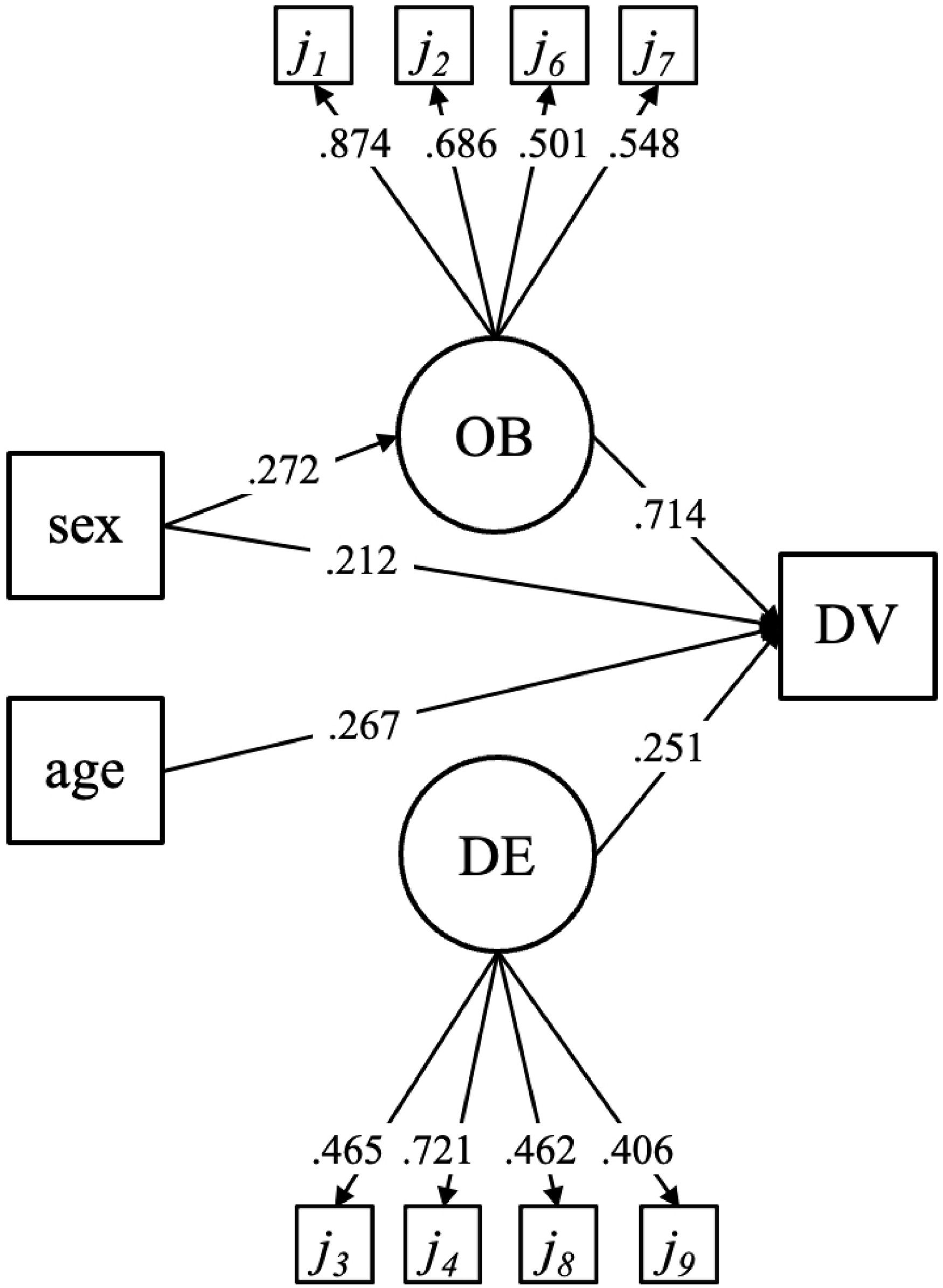
Fig. 2 depicts a logistic regression model that includes the two substantive factors of the DVSS-Sp scale (OB and DE) as independent variables, along with sex and age. The diagnosis of dysfunctional voiding (coded as 1 for yes and 0 for no) was considered the dependent variable. Items 5 and 10 were not included in the model because they showed no significance in the factor analyses, as indicated in Table 2. The factor loadings followed the pattern shown in Table 2. Both sex and age had a significant but modest effect (0.272, 0.267, and 0.212, respectively). The impact of DE and OB on age was not statistically significant. This model accounted for 79% of the variance in the diagnosis.
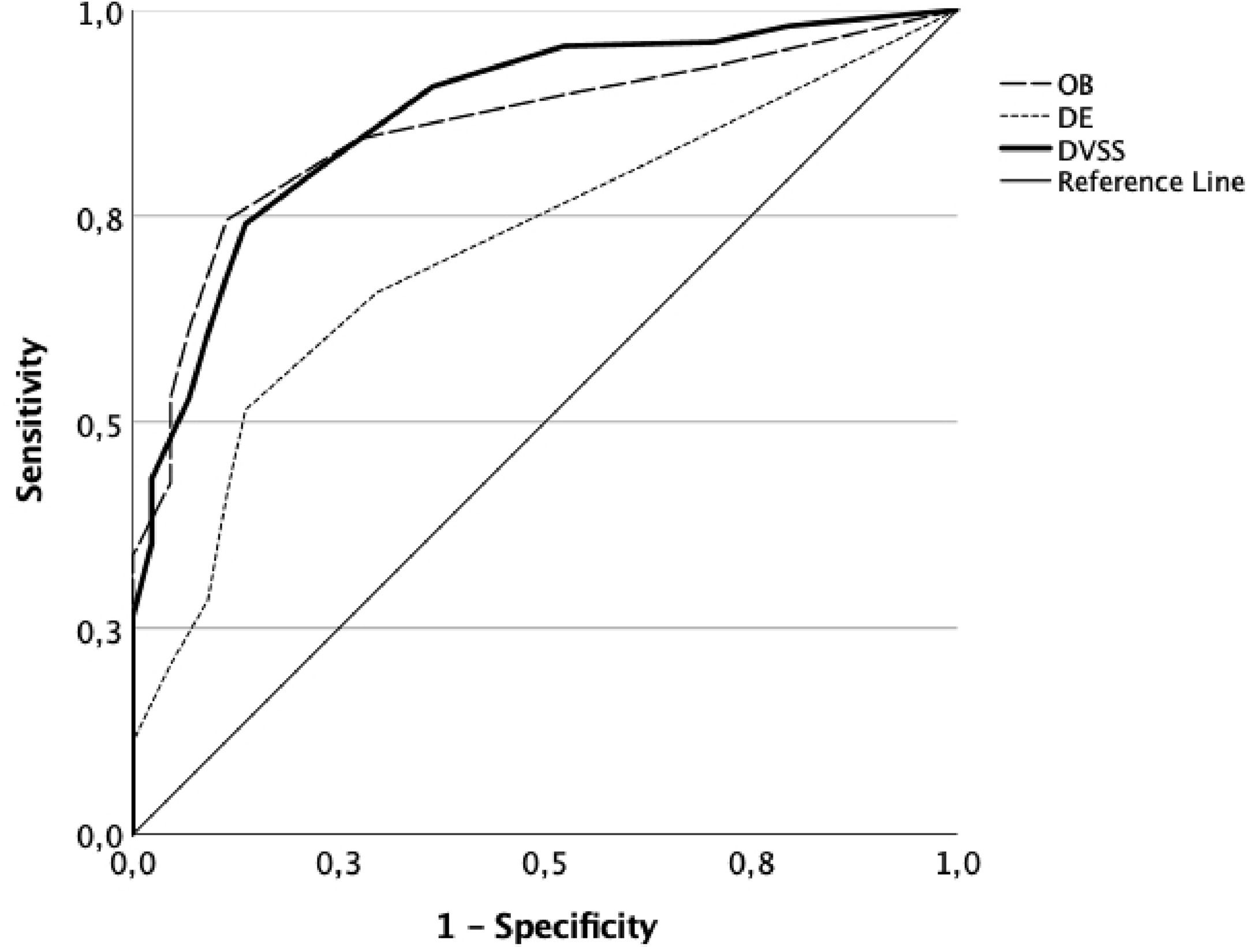
In the graph of Fig. 3, the ROC curve showed a pronounced curvature. The estimated area under the curve (AUC) of the DVSS-Sp was 0.87, 95% CI [0.82, 0.93]. The DVSS-Sp AUC was like the OB factor AUC (0.86, 95% CI [0.80, 0.91])—the good results of the previous logistic regression agreed with those of the ROC curve. Considering only items 1, 2, 3, 4, 6, 7, 8, and 9, and assuming a cut-off score of 3.5 on the DVSS-Sp scale, the specificity was 0.907, and the sensitivity was 0.636.
DiscussionThis study aimed to translate and culturally adapt the DVSS questionnaire into Spanish and to evaluate the psychometric properties of the DVSS-Sp in Chilean children with DVIs.
Our study culturally adapted the DVSS using the methodology proposed by the ITC,21 widely referred to by other authors, to demonstrate semantic, cultural, and conceptual equivalence. The translation and back-translation process from the original version and the evaluation of the committee of experts suggests an adequate correspondence between the transcultural adaptation and the original version. In addition, the pilot study demonstrated a suitable understanding of the instructions and the items.
The EFA showed two dimensions, OB and DE. This structure presented excellent goodness-of-fit indices. Chang et al.,12 analyzed the factor structure from an exploratory perspective, observing a 3-factor structure: 1) hyperactive bladder symptoms; 2) dysfunction elimination symptoms; and 3) stress and pain to pee symptoms.12 Our data did not present the configuration with Factor 3. In addition, in the present study, item 9 (i.e., pain when peeing) was associated with the dimension DE, presenting theoretical agreement with the other items in the dimension. The factors OB and DE had a low relationship, which shows that it evaluates different constructs. It would be beneficial to diagnose DVI difficulties differentially, specifically distinguishing between cases of bladder overactivity on the one hand and issues related to evacuation difficulties on the other. It is relevant to emphasize that other studies have not addressed the factor structure, which is why further investigation is required.
Items 5 and 10 were not related to any factor. Item 5 considers the number of trips to the bathroom during the day. Not specifying if this refers to urinating or defecating can lead to confusion. In the case of defecating, going to the bathroom once or twice a day is expected and does not constitute a sign of pathology.25 However, urinating once or twice a day is a sign of alteration. It is considered normal to urinate 4–7 times a day.26 Thus, because the item seeks to determine whether the child has retention behavior or not, we believe this can be improved by explicitly adding if it is to urinate or defecate, as Chang et al.12 and Cirovic et al.14 specified, and the normal range of bathroom visits. The Korean version of the DVSS suggests that the question could contain whether it is in the day or at night.10 It is suggested that cultural beliefs could influence the response, arguing that frequent voiding activities in one day would be embarrassing.27 Future studies must analyze this last point. On the other hand, item 10 was not related to either OB or DE. This item evaluates the presence of psychological stressors in the last month. The presence of the stressful events asked about can impact a child in a variety of ways. In this vein, including items that assess stress on pediatric DVI questionnaires is controversial.12 Particularly, if it is considered that the DVSS assesses the symptoms of DVI and is used to monitor the evolution and response to treatment of children who suffer from DVI symptoms. Stress could be linked to the etiology of DVI symptoms, more than being a symptom of it. Although item 10 has significantly predicted DVI symptoms,13 we think that incorporating a specific questionnaire into clinical practice that evaluates stress or the psychoemotional impact of DVI symptoms could improve the understanding of the clinical picture of the boy or girl. Consequently, these two items that have shown inadequate functioning in the factor models (i.e., items 5 and 10) should be removed or modified, and better content put in their place.
With respect to reliability, the DVSS-Sp showed acceptable results for OB (α 0.70 and ω 0.73), but not adequate for DE (α 0.57 and ω 0.62). The scale needs to improve its internal reliability indicators in both factors. Chang et al.12 evaluated the Chinese version of DVSS and found α = 0.45, calculating the reliability with all the items and not for the factors. This affects the value of the reliability.
A logistic regression analysis indicates a good diagnostic capacity of the DVSS-Sp scale. For any diagnostic tool, the AUC should exceed 0.5, and generally, it should be greater than 0.8 to be considered acceptable. In our study, the obtained value surpasses the latter threshold (0.87). Additionally, the ROC analysis revealed a cut-off value of 3.5 on the DVSS scale, with a specificity of 0.907 and a sensitivity of 0.636. It would be advisable to reanalyze the data from the remaining adaptations of this scale to other languages using appropriate factor models. The same pattern of results would likely be replicated, as observed in this study.
Our study contributes evidence of the validity of the DVSS-Sp, a valuable tool for both the clinical and research areas in Spanish-speaking communities, because there are no other instruments with these characteristics in this language. To the best of our knowledge, this is the first study to perform a transcultural adaptation of the DVSS into Spanish while evaluating its psychometric properties. This instrument could be used to evaluate the effectiveness of treatments, follow-up, and compare the results obtained by children with DVI symptoms. It is important to note that the validation of DVSS-Sp was done following rigorous methodological and statistical criteria. Finally, there is a need for instruments that are brief and easy to apply in clinical contexts, with suitable psychometric properties.
Nevertheless, it would be convenient to analyze again, with the appropriate factorial models, the data from the rest of the adaptations of this scale to other languages. It is almost certain that the same pattern of results would be reproduced as in this study.
Our study is not without limitations. It is important to consider that the COVID-19 pandemic demanded a modification of the protocol for online application, which did not make it possible to clarify questions immediately. The differences between the control group and the DVI symptoms group in relation to the distribution by sex (79% girls) and controls (39% girls) could also pose an obstacle to the analysis. Nevertheless, the group's composition with DVI symptoms was mainly girls, which is consistent with the nature of this condition. The sample was recruited in only one center, so the results cannot be extrapolated to other populations.
ConclusionThe results of this study support the use of the DVSS-Sp as a suitable tool to assess DVI symptoms in Chilean boys and girls, with potential for its use in other Spanish-speaking countries.
We thank Darius Bagli, author of the DVSS questionnaire, for authorizing this research. To the Corporación Renal Infantil MATER, for supporting and contributing to the recruitment of the sample without any financial interest. To the Research Department of the Universidad de La Frontera for funding the translation of this paper. And we also want to mention and thank Gabriela Retamal, Matilde Osses, Alejandra Pastene and Bernardita Fuentes for selflessly participating in the process.
This study was approved by the Scientific Ethics Committee of the South Metropolitan Health Service (Cod. 85-04102019).