Joint angle data from healthy subjects are necessary as baseline information.
ObjectiveTo analyze the problems of patients who struggle with activities of daily living (ADL) due to restricted range of motion and to provide ADL guidance based on objective data.
MethodAn electromagnetic three-dimensional tracking system (FASTRAK) was used to quantify the hip, knee, and ankle angles of the dominant leg of 26 healthy adults as they performed 22 ADLs related to dressing, using the toilet, bathing, picking up objects, and crouching. For each ADL, the maximum angle was averaged across the 26 subjects. Mean angles of adduction/abduction and internal/external rotation during maximum hip flexion were also measured.
ResultsThe largest mean maximum angle was 101° for hip flexion (trunk rotation during crouching), 17° for hip adduction (putting on shoes), and 149° for knee flexion (trunk rotation during crouching). Analysis of adduction/abduction and internal/external rotation angles during maximum hip flexion showed the largest angle of adduction when putting on shoes, and the largest angle of internal rotation with trunk rotation during crouching.
ConclusionsADLs such as crouching and putting on pants showed larger joint angles than walking, climbing stairs, and standing up. Results obtained from this study can provide important objective data for ADL guidance for total hip arthroplasty and femoroacetabular impingement patients.
The range of motion (ROM) of the lower limb joints may be restricted in musculoskeletal patients with joint disease or bone fracture and in individuals who have undergone surgery such as total joint arthroplasty.1–3 Restricted ROM of the lower limb joints hinders the performance of activities of daily living (ADL)4 such as walking, standing up, and climbing stairs.5–7 Patients may also have difficulty with activities such as dressing, using the toilet, bathing, picking up objects, crouching, tying shoelaces, and clipping toenails.5,6,8,9
To elucidate the problems of patients who struggle with ADLs due to restricted ROM, we used joint angle data from healthy subjects for comparison. Moreover, the maximum joint angles that occurred during ADLs in healthy individuals can serve as ROM targets for patients. Numerous studies have reported the lower limb joint angles involved in walking, standing up, and climbing stairs10,11 in normal subjects, but few have addressed self-care activities. In dressing, the only activity that has been studied is tying shoelaces.12 In bathing, one study reported the knee joint angles involved in getting in the bath.13 No studies have examined the lower limb joint angles required for using a toilet, dressing, or getting out of the bath. The only report with respect to picking up objects studied the hip joint,12 and although crouching has been analyzed at rest,9 no studies have analyzed the dynamic crouching motions involved in tasks such as gardening or picking up objects off the floor. Movements such as these may be difficult for patients with restricted ROM.5,6,8,9
Limited ROM not only hinders the performance of ADLs, but also restricts activities, particularly in patients after total hip arthroplasty (THA). However, no reports have measured multiple joint angles in ADLs that are speculated to be risky in terms of dislocation, and thus ADL guidance still cannot be considered to be based on objective data. Data from healthy individuals are clearly not directly applicable to patients, but their data on adduction/abduction and internal/external rotation angles for maximum hip flexion during ADLs can provide indicators for objective ADL guidance.
This study aimed to quantify hip, knee, and ankle joint angles in healthy subjects during ADLs such as dressing, using the toilet, bathing, picking up objects, and crouching. These ADLs can require larger joint angles than those encountered during walking, standing up, and climbing stairs. The joint angles that occurred in healthy individuals during ADLs were measured and compared with those of patients with restricted ROM, as described in previous reports. In addition, adduction/abduction and internal/external rotation angles during maximum hip flexion while performing these activities were also measured. The extent to which multiple joint motions occur in healthy individuals during the measured ADLs was categorized.
MethodParticipantsParticipants were 26 healthy subjects (13 men, 13 women) with no symptoms involving the lower extremities. Mean (±standard deviation) age, height, weight, and body mass index were 20±1 years, 168±7cm, 60±7kg, and 21±1kg/m2, respectively. The dominant foot was defined as the foot that could kick a ball the greatest distance, and all participants were right-foot dominant. The appropriate ethics review board approved this study. All participants received written information about the study and provided consent before enrolling.
Data collectionKinematic measurements were taken using an electromagnetic three-dimensional tracking system (3SPACE FASTRAK, Polhemus, Colchester, VT, USA). This apparatus included a system control unit, a transmitter, and four receivers. According to the manufacturer of the device, the apparatus measures the three-dimensional position and angle of each receiver within the magnetic field produced by the transmitter. The measurement range is a hemisphere with a radius of 76cm from the transmitter. Within this range, the measurement error in receiver position is 0.3–0.8mm and the measurement error in receiver angle is 0.15° (3SPACE FASTRAK User Manual; Polhemus). The position of the transmitter was adjusted as required to ensure that the receivers remained within measurement range during the performance of each task. A sampling rate of 30Hz was used.
Measurements were made only for the dominant (right) leg. Four receivers were attached to the leg on the foot, lower leg, thigh, and sacrum. These receivers were positioned away from areas with a large proportion of soft tissue to minimize errors in receiver position due to soft tissue movement.14 The foot receiver was positioned on the lateral-dorsal surface of the foot. The lower leg receiver was positioned on the lateral side of the leg, one third of the way down from the knee joint. The thigh receiver was positioned on the lateral side of the leg, one third of the way up from the knee joint. The sacrum receiver was attached to the skin overlaying the sacrum.
At the start of the experimental session, the positions and orientations of the receivers were recorded while the participant stood still in a reference position with neutral hip flexion/extension, neutral hip adduction/abduction, neutral hip internal/external rotation, knee extension, and neutral ankle dorsiflexion/plantar flexion. Each joint angle was confirmed using a goniometer. For hip flexion/extension, adduction/abduction, internal/external rotation, knee flexion, and ankle dorsiflexion/plantar flexion in each participant, differences between the FASTRAK joint angle measurements and goniometry measurements were within 5°.
TasksJoint angles were measured during 22 tasks that mimicked dressing (tasks 1–7), using a toilet (tasks 8 and 9), bathing (tasks 10–19), picking up objects (tasks 20–21), and trunk rotation during crouching (task 22; Table 1). These tasks were performed in order. The tasks were chosen with reference to tasks performed in the Functional Independence Measure of ADLs and previous studies of ADLs involving the lower limbs.5,7,9,15,16
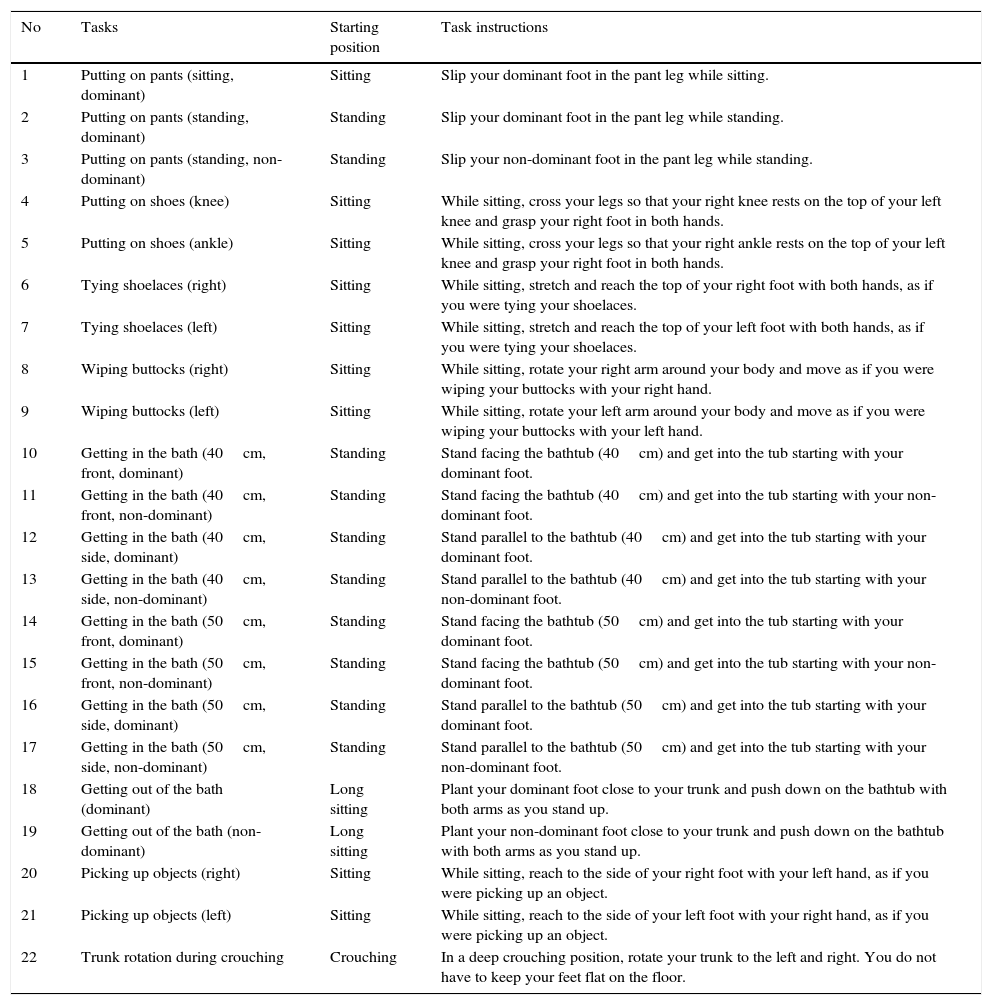
Movement tasks performed.
| No | Tasks | Starting position | Task instructions |
|---|---|---|---|
| 1 | Putting on pants (sitting, dominant) | Sitting | Slip your dominant foot in the pant leg while sitting. |
| 2 | Putting on pants (standing, dominant) | Standing | Slip your dominant foot in the pant leg while standing. |
| 3 | Putting on pants (standing, non-dominant) | Standing | Slip your non-dominant foot in the pant leg while standing. |
| 4 | Putting on shoes (knee) | Sitting | While sitting, cross your legs so that your right knee rests on the top of your left knee and grasp your right foot in both hands. |
| 5 | Putting on shoes (ankle) | Sitting | While sitting, cross your legs so that your right ankle rests on the top of your left knee and grasp your right foot in both hands. |
| 6 | Tying shoelaces (right) | Sitting | While sitting, stretch and reach the top of your right foot with both hands, as if you were tying your shoelaces. |
| 7 | Tying shoelaces (left) | Sitting | While sitting, stretch and reach the top of your left foot with both hands, as if you were tying your shoelaces. |
| 8 | Wiping buttocks (right) | Sitting | While sitting, rotate your right arm around your body and move as if you were wiping your buttocks with your right hand. |
| 9 | Wiping buttocks (left) | Sitting | While sitting, rotate your left arm around your body and move as if you were wiping your buttocks with your left hand. |
| 10 | Getting in the bath (40cm, front, dominant) | Standing | Stand facing the bathtub (40cm) and get into the tub starting with your dominant foot. |
| 11 | Getting in the bath (40cm, front, non-dominant) | Standing | Stand facing the bathtub (40cm) and get into the tub starting with your non-dominant foot. |
| 12 | Getting in the bath (40cm, side, dominant) | Standing | Stand parallel to the bathtub (40cm) and get into the tub starting with your dominant foot. |
| 13 | Getting in the bath (40cm, side, non-dominant) | Standing | Stand parallel to the bathtub (40cm) and get into the tub starting with your non-dominant foot. |
| 14 | Getting in the bath (50cm, front, dominant) | Standing | Stand facing the bathtub (50cm) and get into the tub starting with your dominant foot. |
| 15 | Getting in the bath (50cm, front, non-dominant) | Standing | Stand facing the bathtub (50cm) and get into the tub starting with your non-dominant foot. |
| 16 | Getting in the bath (50cm, side, dominant) | Standing | Stand parallel to the bathtub (50cm) and get into the tub starting with your dominant foot. |
| 17 | Getting in the bath (50cm, side, non-dominant) | Standing | Stand parallel to the bathtub (50cm) and get into the tub starting with your non-dominant foot. |
| 18 | Getting out of the bath (dominant) | Long sitting | Plant your dominant foot close to your trunk and push down on the bathtub with both arms as you stand up. |
| 19 | Getting out of the bath (non-dominant) | Long sitting | Plant your non-dominant foot close to your trunk and push down on the bathtub with both arms as you stand up. |
| 20 | Picking up objects (right) | Sitting | While sitting, reach to the side of your right foot with your left hand, as if you were picking up an object. |
| 21 | Picking up objects (left) | Sitting | While sitting, reach to the side of your left foot with your right hand, as if you were picking up an object. |
| 22 | Trunk rotation during crouching | Crouching | In a deep crouching position, rotate your trunk to the left and right. You do not have to keep your feet flat on the floor. |
The same research associate explained the initial and final positions. To learn these positions, the participants practiced the motions several times before the actual measurements. Each motion was carried out in triplicate. The final position of the motion was held for approximately 5s.
Data analysisJoint angles were measured according to the recommendations of the International Society of Biomechanics.17 In this recommendation, the Euler sequence of the hip joint, for example, is in this order: flexion/extension, adduction/abduction, and internal/external rotation. Analysis was performed on the second of the three consecutive motions. The maximum hip joint angle (flexion, extension, adduction, abduction, internal rotation, and external rotation), knee joint angle (flexion and extension), and ankle joint angle (dorsiflexion and plantarflexion) were determined during each task. The magnitudes of hip adduction/abduction and internal/external rotation at the time of maximum hip flexion were also determined. Data are expressed as the mean and standard deviation for the 26 participants.
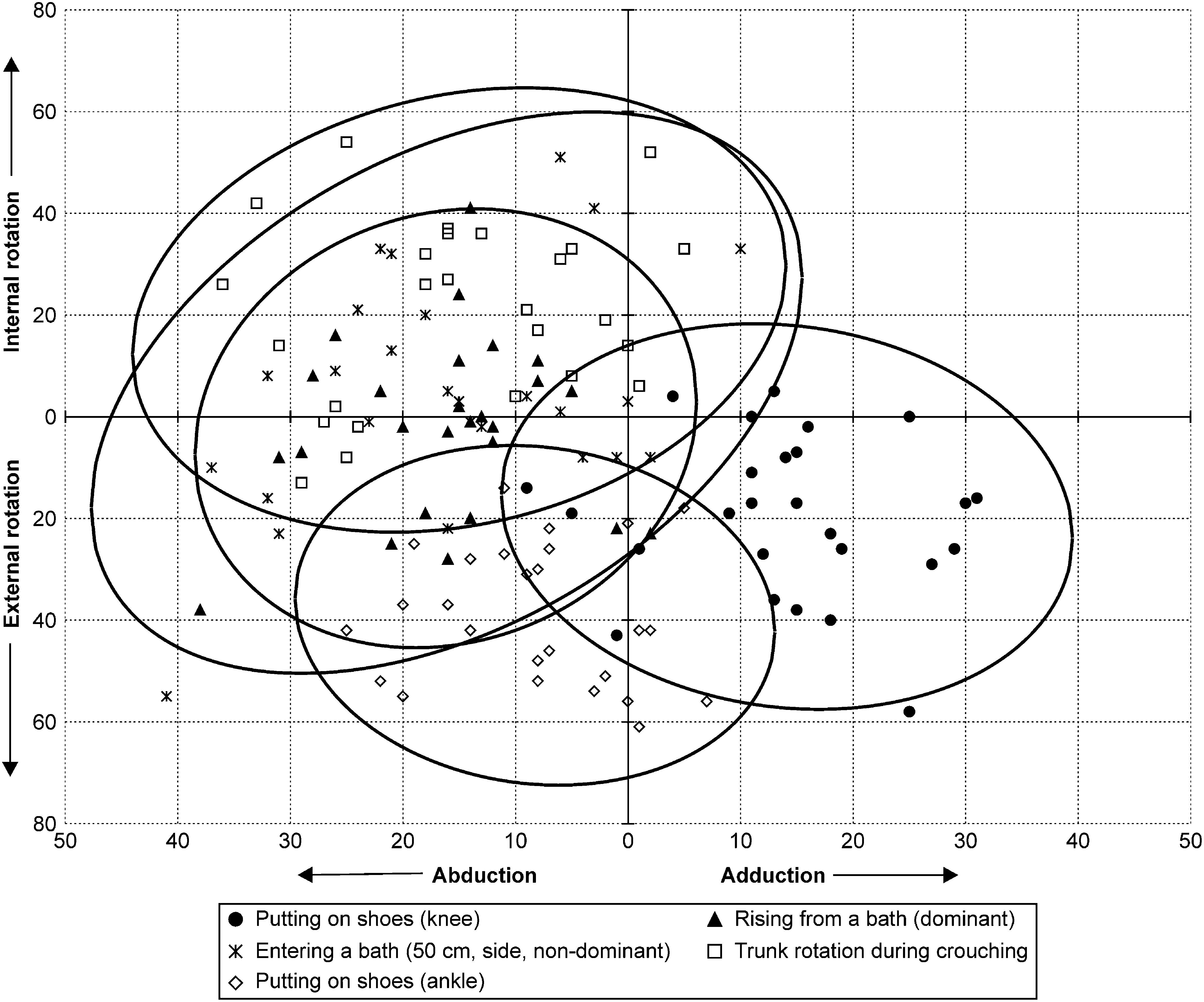
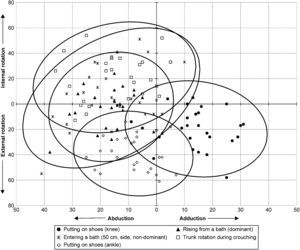
To examine the relationships between the present study results and post-THA dislocation, it is necessary to analyze the combinations of adduction/abduction and internal/external rotation for each task in each subject. The Mahalanobis distance was computed for the observed data, and then a probability ellipse of constant Mahalanobis distance indicating the 95% confidence interval for each movement was drawn.
The ethics review board of Mejiro University, Saitama, Japan approved this study (approval number: 201108).
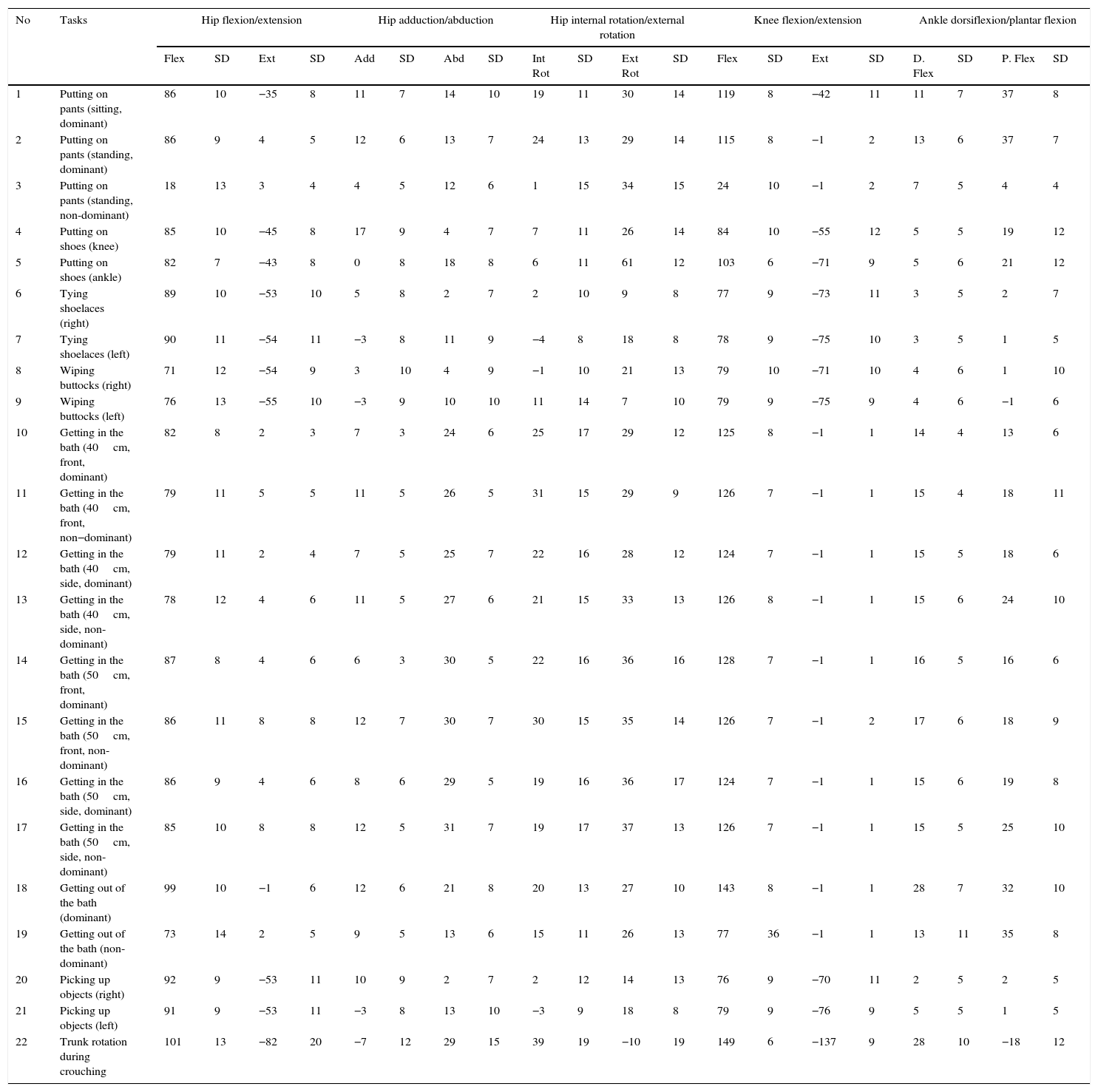
ResultsMean maximum hip, knee, and ankle joint angles during each task are shown in Table 2. The largest mean maximum angle was 101° for hip flexion (task 22: trunk rotation during crouching), 8° for hip extension [task 15: getting in the bath (50cm, front, non-dominant) and task 17: getting in the bath (50cm, side, non-dominant)], 17° for hip adduction [task 4: putting on shoes (knee)], 31° for hip abduction [task 17: getting in the bath (50cm, side, non-dominant)], 39° for hip internal rotation (task 22: trunk rotation during crouching), 61° for hip external rotation [task 5: putting on shoes (ankle)], 149° for knee flexion (task 22: trunk rotation during crouching), 28° for ankle dorsiflexion [task 18: getting out of the bath (dominant) and task 22: trunk rotation during crouching] and 37° for ankle plantar flexion [task 1: putting on pants (sitting, dominant) and task 2: putting on pants (standing, dominant); Table 2].
Maximum flexion (Flex), extension (Ext), adduction (Add), abduction (Abd), internal rotation (Int Rot), and external rotation (Ext Rot) of the hip joint, flexion (Flex) of the knee joint, and plantar flexion (P. Flex) and dorsiflexion (D. Flex) of the ankle joint during each task.
| No | Tasks | Hip flexion/extension | Hip adduction/abduction | Hip internal rotation/external rotation | Knee flexion/extension | Ankle dorsiflexion/plantar flexion | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Flex | SD | Ext | SD | Add | SD | Abd | SD | Int Rot | SD | Ext Rot | SD | Flex | SD | Ext | SD | D. Flex | SD | P. Flex | SD | ||
| 1 | Putting on pants (sitting, dominant) | 86 | 10 | −35 | 8 | 11 | 7 | 14 | 10 | 19 | 11 | 30 | 14 | 119 | 8 | −42 | 11 | 11 | 7 | 37 | 8 |
| 2 | Putting on pants (standing, dominant) | 86 | 9 | 4 | 5 | 12 | 6 | 13 | 7 | 24 | 13 | 29 | 14 | 115 | 8 | −1 | 2 | 13 | 6 | 37 | 7 |
| 3 | Putting on pants (standing, non-dominant) | 18 | 13 | 3 | 4 | 4 | 5 | 12 | 6 | 1 | 15 | 34 | 15 | 24 | 10 | −1 | 2 | 7 | 5 | 4 | 4 |
| 4 | Putting on shoes (knee) | 85 | 10 | −45 | 8 | 17 | 9 | 4 | 7 | 7 | 11 | 26 | 14 | 84 | 10 | −55 | 12 | 5 | 5 | 19 | 12 |
| 5 | Putting on shoes (ankle) | 82 | 7 | −43 | 8 | 0 | 8 | 18 | 8 | 6 | 11 | 61 | 12 | 103 | 6 | −71 | 9 | 5 | 6 | 21 | 12 |
| 6 | Tying shoelaces (right) | 89 | 10 | −53 | 10 | 5 | 8 | 2 | 7 | 2 | 10 | 9 | 8 | 77 | 9 | −73 | 11 | 3 | 5 | 2 | 7 |
| 7 | Tying shoelaces (left) | 90 | 11 | −54 | 11 | −3 | 8 | 11 | 9 | −4 | 8 | 18 | 8 | 78 | 9 | −75 | 10 | 3 | 5 | 1 | 5 |
| 8 | Wiping buttocks (right) | 71 | 12 | −54 | 9 | 3 | 10 | 4 | 9 | −1 | 10 | 21 | 13 | 79 | 10 | −71 | 10 | 4 | 6 | 1 | 10 |
| 9 | Wiping buttocks (left) | 76 | 13 | −55 | 10 | −3 | 9 | 10 | 10 | 11 | 14 | 7 | 10 | 79 | 9 | −75 | 9 | 4 | 6 | −1 | 6 |
| 10 | Getting in the bath (40cm, front, dominant) | 82 | 8 | 2 | 3 | 7 | 3 | 24 | 6 | 25 | 17 | 29 | 12 | 125 | 8 | −1 | 1 | 14 | 4 | 13 | 6 |
| 11 | Getting in the bath (40cm, front, non−dominant) | 79 | 11 | 5 | 5 | 11 | 5 | 26 | 5 | 31 | 15 | 29 | 9 | 126 | 7 | −1 | 1 | 15 | 4 | 18 | 11 |
| 12 | Getting in the bath (40cm, side, dominant) | 79 | 11 | 2 | 4 | 7 | 5 | 25 | 7 | 22 | 16 | 28 | 12 | 124 | 7 | −1 | 1 | 15 | 5 | 18 | 6 |
| 13 | Getting in the bath (40cm, side, non-dominant) | 78 | 12 | 4 | 6 | 11 | 5 | 27 | 6 | 21 | 15 | 33 | 13 | 126 | 8 | −1 | 1 | 15 | 6 | 24 | 10 |
| 14 | Getting in the bath (50cm, front, dominant) | 87 | 8 | 4 | 6 | 6 | 3 | 30 | 5 | 22 | 16 | 36 | 16 | 128 | 7 | −1 | 1 | 16 | 5 | 16 | 6 |
| 15 | Getting in the bath (50cm, front, non-dominant) | 86 | 11 | 8 | 8 | 12 | 7 | 30 | 7 | 30 | 15 | 35 | 14 | 126 | 7 | −1 | 2 | 17 | 6 | 18 | 9 |
| 16 | Getting in the bath (50cm, side, dominant) | 86 | 9 | 4 | 6 | 8 | 6 | 29 | 5 | 19 | 16 | 36 | 17 | 124 | 7 | −1 | 1 | 15 | 6 | 19 | 8 |
| 17 | Getting in the bath (50cm, side, non-dominant) | 85 | 10 | 8 | 8 | 12 | 5 | 31 | 7 | 19 | 17 | 37 | 13 | 126 | 7 | −1 | 1 | 15 | 5 | 25 | 10 |
| 18 | Getting out of the bath (dominant) | 99 | 10 | −1 | 6 | 12 | 6 | 21 | 8 | 20 | 13 | 27 | 10 | 143 | 8 | −1 | 1 | 28 | 7 | 32 | 10 |
| 19 | Getting out of the bath (non-dominant) | 73 | 14 | 2 | 5 | 9 | 5 | 13 | 6 | 15 | 11 | 26 | 13 | 77 | 36 | −1 | 1 | 13 | 11 | 35 | 8 |
| 20 | Picking up objects (right) | 92 | 9 | −53 | 11 | 10 | 9 | 2 | 7 | 2 | 12 | 14 | 13 | 76 | 9 | −70 | 11 | 2 | 5 | 2 | 5 |
| 21 | Picking up objects (left) | 91 | 9 | −53 | 11 | −3 | 8 | 13 | 10 | −3 | 9 | 18 | 8 | 79 | 9 | −76 | 9 | 5 | 5 | 1 | 5 |
| 22 | Trunk rotation during crouching | 101 | 13 | −82 | 20 | −7 | 12 | 29 | 15 | 39 | 19 | −10 | 19 | 149 | 6 | −137 | 9 | 28 | 10 | −18 | 12 |
A value of zero indicates the neutral position, and positive values indicate more extreme than neutral in the stated direction. For example, an extension angle of −35° indicates that extension was not detected during the motion, and the most extended position was 35° of flexion.
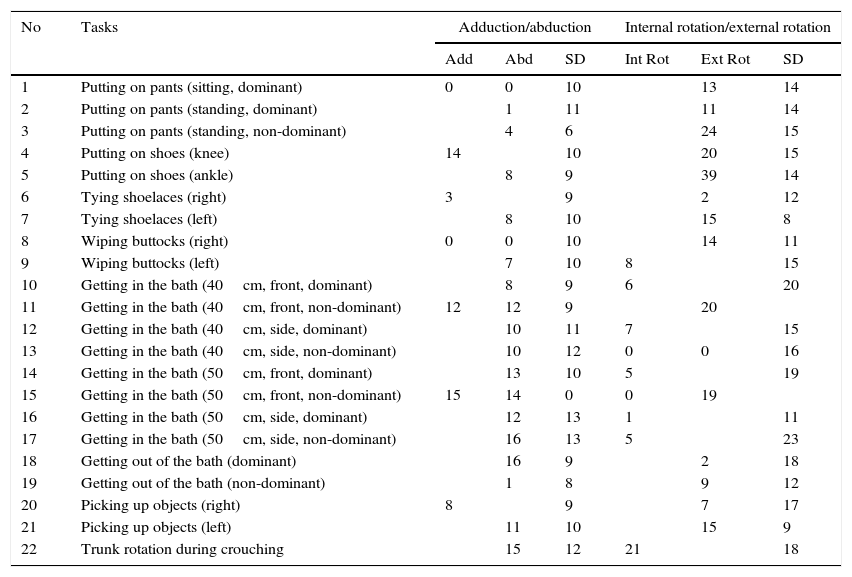
Adduction/abduction and internal/external rotation of the hip joint at the point of maximum hip flexion are shown in Table 3. Adduction was greatest for task 4 [putting on shoes (knee)]. Abduction was greatest for task 18 [getting out of the bath (dominant foot)] and task 17 [getting in the bath (50cm, side, non-dominant foot)]. Internal rotation was greatest for task 22 (trunk rotation during crouching), and external rotation was greatest for task 5 [putting on shoes (ankle)]. The probability ellipses for these five tasks are shown in Fig. 1. There was a trend for hip adduction and external rotation at the point of maximum hip flexion during task 4 [putting on shoes (knee)], abduction and external rotation at the point of maximum hip flexion during task 18 [getting out of the bath (dominant foot)] and task 5 [putting on shoes (ankle)], and abduction and internal rotation at the point of maximum hip flexion during task 17 [getting in the bath (50cm, side, non-dominant foot)] and task 22 (trunk rotation during crouching). There were no movements with simultaneous adduction and internal rotation (Fig. 1, Table 3). However, there was considerable inter-individual variability. For example, for task 17 [getting in the bath (50cm, side, non-dominant foot)], the hip was externally rotated at the point of maximum hip flexion in 11 of the 26 subjects (Fig. 1).
Adduction/abduction and internal/external rotation angles at the time of maximum hip joint flexion.
| No | Tasks | Adduction/abduction | Internal rotation/external rotation | ||||
|---|---|---|---|---|---|---|---|
| Add | Abd | SD | Int Rot | Ext Rot | SD | ||
| 1 | Putting on pants (sitting, dominant) | 0 | 0 | 10 | 13 | 14 | |
| 2 | Putting on pants (standing, dominant) | 1 | 11 | 11 | 14 | ||
| 3 | Putting on pants (standing, non-dominant) | 4 | 6 | 24 | 15 | ||
| 4 | Putting on shoes (knee) | 14 | 10 | 20 | 15 | ||
| 5 | Putting on shoes (ankle) | 8 | 9 | 39 | 14 | ||
| 6 | Tying shoelaces (right) | 3 | 9 | 2 | 12 | ||
| 7 | Tying shoelaces (left) | 8 | 10 | 15 | 8 | ||
| 8 | Wiping buttocks (right) | 0 | 0 | 10 | 14 | 11 | |
| 9 | Wiping buttocks (left) | 7 | 10 | 8 | 15 | ||
| 10 | Getting in the bath (40cm, front, dominant) | 8 | 9 | 6 | 20 | ||
| 11 | Getting in the bath (40cm, front, non-dominant) | 12 | 12 | 9 | 20 | ||
| 12 | Getting in the bath (40cm, side, dominant) | 10 | 11 | 7 | 15 | ||
| 13 | Getting in the bath (40cm, side, non-dominant) | 10 | 12 | 0 | 0 | 16 | |
| 14 | Getting in the bath (50cm, front, dominant) | 13 | 10 | 5 | 19 | ||
| 15 | Getting in the bath (50cm, front, non-dominant) | 15 | 14 | 0 | 0 | 19 | |
| 16 | Getting in the bath (50cm, side, dominant) | 12 | 13 | 1 | 11 | ||
| 17 | Getting in the bath (50cm, side, non-dominant) | 16 | 13 | 5 | 23 | ||
| 18 | Getting out of the bath (dominant) | 16 | 9 | 2 | 18 | ||
| 19 | Getting out of the bath (non-dominant) | 1 | 8 | 9 | 12 | ||
| 20 | Picking up objects (right) | 8 | 9 | 7 | 17 | ||
| 21 | Picking up objects (left) | 11 | 10 | 15 | 9 | ||
| 22 | Trunk rotation during crouching | 15 | 12 | 21 | 18 | ||
The solid line represents the probability ellipse for each of the five tasks of interest. The tasks of interest were the tasks with the greatest hip adduction, abduction, internal rotation, and external rotation angles at the time of maximum hip joint flexion. The relationship between abduction/adduction angle at the time of maximum hip flexion and the internal/external rotation angle at the time of maximum hip flexion for each of the five tasks of interest is shown.
The present study provides detailed data on the maximum lower limb joint angles during dressing, using a toilet, bathing, picking up objects, and crouching. The findings from healthy individuals can serve as reference data for comparison with patients who struggle with ADLs due to restricted ROM.
Many previous studies have addressed restricted ROM, particularly following joint arthroplasty in the legs.18–20 For example, in patients with total hip replacement, the hip joint is reported to have a maximum flexion of 91°, maximum adduction of 25°, and maximum internal rotation of 6°,21 making the ROM of these patients smaller than that of healthy individuals.22 The same applies to patients with total knee replacement.23 Mobility following joint arthroplasty is generally discussed with reference to actions such as walking, climbing stairs, and standing up.13,20 After total knee arthroplasty, flexion of 100–110° has been suggested as necessary for ADLs.24 However, this reference value is for walking, climbing stairs, and standing up, and cannot be applied to other ADLs.
Studies measuring the joint angles involved in walking, climbing stairs, and standing up have reported that hip flexion of 80°, knee flexion of 110°, ankle dorsiflexion of 26° are required.10,25,26 The present results indicate that other ADLs require more extreme joint angles than walking, climbing stairs, or standing up. There were 12 movements for which the average maximum knee flexion angle exceeded 110°. Average maximum knee flexion exceeded 140° during trunk rotation during crouching and getting out of the bath with the dominant foot. Therefore, these movements require more knee flexion than needed for walking, climbing stairs, or standing up. In addition, there were 15 movements in which the average maximum hip flexion angle exceeded 80°. Average maximum hip flexion was around 100° while getting out of the bath with the dominant foot and rotating the trunk during crouching. For the ankle, dorsiflexion exceeded 26° (the amount of dorsiflexion required for climbing stairs) while getting out of the bath with the dominant foot and rotating the trunk during crouching.
Since the study participants were young adults in their early twenties, the present results are not directly applicable to postoperative patients. Moreover, movements made by postoperative patients who have limited joint angles may differ from those of healthy individuals. To use the results from the present study as reference values, it is necessary to compare the present results to previous studies that have assessed ADLs and body movement methods of postoperative patients. Although there are no studies that have comprehensively analyzed the body movement methods of postoperative patients, several studies investigated the association between ADLs and ROM in postoperative patients. In a study that assessed the association between ROM and ADLs in patients who had undergone THA, it was reported that the ROMs of hip flexion, abduction, adduction, and internal rotation affected activities of putting on socks, tying shoelaces, and clipping toenails on the operated leg.7 A report that surveyed ADLs in patients who had undergone total knee arthroplasty showed that the majority of ADLs improved, but kneeling and crouching were often difficult when sufficient knee flexion could not be attained.27 Large hip and knee joint angles were evident in the present study when participants performed tasks of tying shoelaces and crouching, which were also classified as difficult in postoperative patients in the previous studies. This finding suggests that movements requiring large hip and knee mobility (i.e., putting on pants/shoes, getting in/out of the bath, and picking up objects) are also difficult for postoperative patients because the movements that require large hip and knee joint angles in healthy individuals matched the movements that were difficult for postoperative patients.
Limited ROM occurs not only in patients who have undergone total joint arthroplasty, but also in patients with various conditions including rheumatoid arthritis28 and spinal cord injury.29 Rheumatoid arthritis patients often have limited ROM of the hip and knee joints, which can affect their ability to walk, use the toilet, go up/down stairs, get in/out of a bathtub, put on and take off shoes, and clip their toenails.28 Spinal cord injury patients usually have contractures of at least one joint at 1 year after injury. The contracture rate is 32% for the hip, 11% for the knee, and 40% for the ankle.29 Limited ROM occurs in many conditions, and the joints and motions affected vary among these conditions. Studies investigating the influence of limited ROM on various activities require a large amount of ROM data during these activities.
The joint angle data obtained in the present study during self-care tasks, which have not been previously reported by other studies, provide useful information for investigating the relationship between ROM and ADLs. The information from healthy individuals obtained in this study can serve as reference data to analyze problems of patients with various diseases that result in restricted ROM.
In addition to measuring maximum joint angles during activities, the present study also measured adduction/abduction and internal/external rotation angles during maximum hip flexion. These data can be beneficial in providing objective ADL guidance to THA patients at risk of dislocation. Hip dislocation following THA occurs in 2%–11% of patients.30 Positional dislocation is one of the causes of dislocations after THA, and movements that simultaneously require excessive flexion and internal rotation and adduction of the hip are contraindicated because they increase the risk of dislocation.31 To prevent dislocation, certain motions are restricted, and patients are instructed on how to perform ADLs within these restrictions.32 Data on multiple joint angles of the hip during these movements would be necessary during rehabilitation to provide guidance on movements that have a risk of inducing dislocation. In actual movement guidance, it is necessary to verify the absence of excessive hip flexion and internal rotation/adduction movements. In order to accomplish these, data on the internal rotation and adduction angles at the time of maximum hip flexion during particular body movements are crucial.
The results for internal rotation and adduction showed that the largest angle of internal rotation occurred with trunk rotation during crouching, and the largest angle of adduction occurred while putting on shoes (knee). Although detailed analysis in the present study was difficult because video motion analysis was not performed simultaneously with the joint angle measurements, a graph of the measured joint angles showed that maximum hip flexion occurred with trunk rotation during crouching when the trunk was rotated to the right and while putting on shoes (knee) when the motion of crossing the legs was completed. The mean values showed that, compared to trunk rotation during crouching and putting on shoes (knee), the internal rotation/adduction angles were smaller for the other tasks. However, as shown in Fig. 1, these results varied among the participants. Therefore, internal rotation/adduction angles may be greater than these mean values in some cases. In actual activity guidance, the adduction/abduction and internal/external rotation angles at the point of maximum flexion during activities are measured using a goniometer, and the presence of excessive adduction/abduction and internal/external rotation can be confirmed by comparing the measured results with the mean values obtained in the present study.
The results in Table 3 show no tasks in which internal rotation/adduction occurred simultaneously. These are mean values, so although simultaneous internal rotation/adduction may have occurred in some participants, the number of participants with simultaneous internal rotation/adduction was small (Fig. 1). The results were similar for 17 other tasks not shown in Fig. 1. Measurement of adduction/abduction and internal/external rotation angles other than during maximum hip flexion was not performed in this study. Therefore, although assessing the risk for dislocation based on the present results alone may be difficult, few participants had internal rotation/adduction during maximum hip flexion angles with these activities. This is important information to consider when instructing patients about these activities.
Restriction of movement after THA has been recently suggested to be unnecessary.33 To eliminate postoperative restrictions, using joint angle references as targets for surgical outcomes is necessary. Although previous studies have identified motions that have a high risk of causing dislocation following THA, these studies have only examined a few ADLs (standing up, sitting, extending the arms to the floor from standing, turning to face the rear while standing, rolling over), and many ADLs remain uninvestigated.34 None of the previous reports has quantified adduction/abduction or internal/external rotation at the point of maximum hip joint flexion, and the relevance of ADLs to dislocation is unclear. Data on the integrated motion of joint angles around three axes enable further investigation of the ADLs that pose a risk of dislocation.
To perform ADLs, it is necessary to integrate the motion of the joints of the lower limbs. The data acquired in the present study can help us understand what kinds of integrated motion are necessary for different ADLs and provide targets for ROM in rehabilitation. In addition to total joint arthroplasty, this may be useful for femoroacetabular impingement, which can cause osteoarthritis of the hip joint.35 In these conditions, it is important to investigate the etiology and assess ROM for ADL guidance. Spinal cord injury and brain injury can also limit ROM in many patients, thus affecting the ability to perform ADLs. The present results provide useful data for these conditions as well.
Conflicts of interestThe authors declare no conflicts of interest.
The authors are grateful to the members of the laboratory who provided carefully considered feedback and valuable comments.