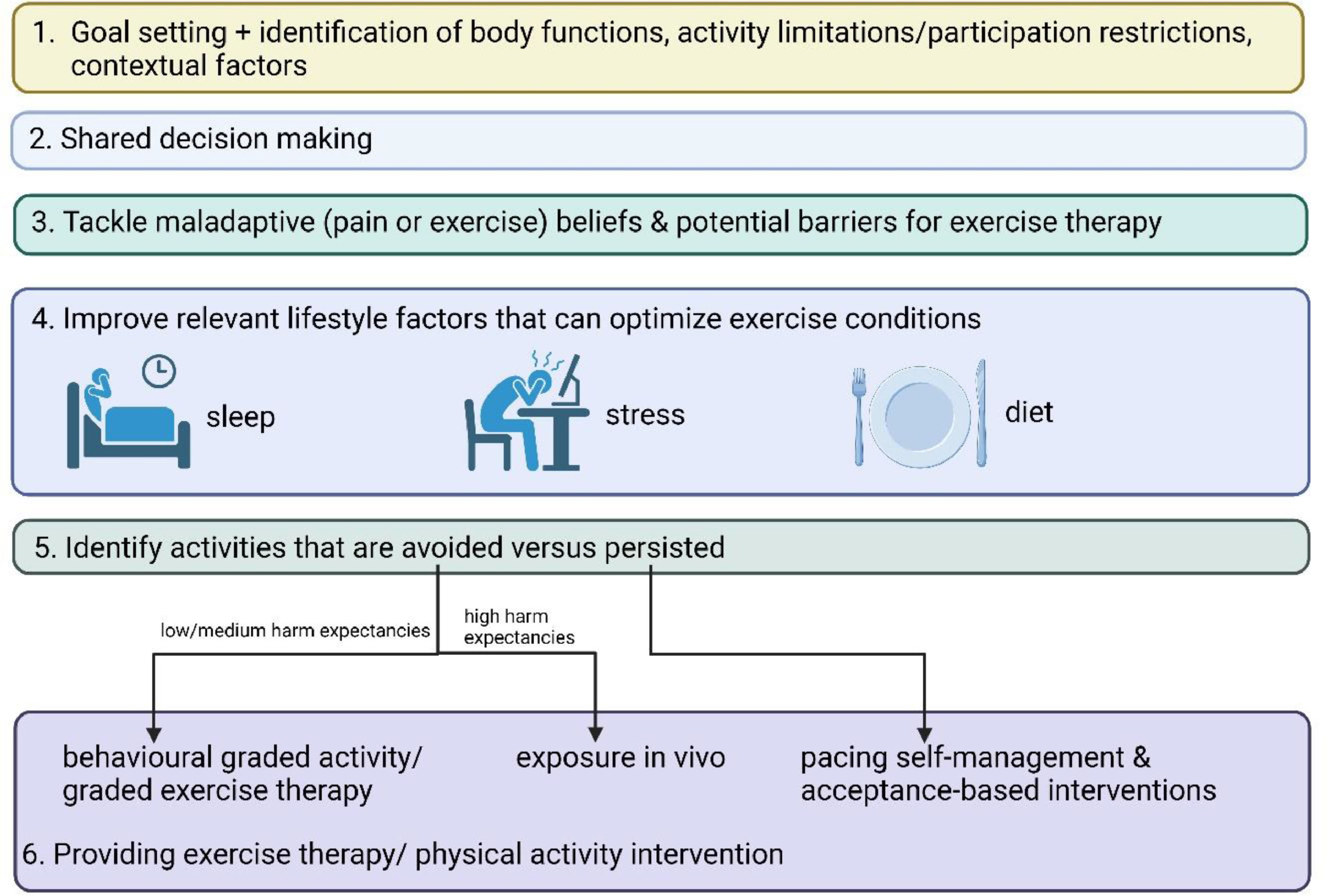
In previous contributions to the Comprehensive Pain Management Editorial Series, we emphasized the importance of improving pain beliefs,1 stress tolerance,2 and sleep,3 as part of multimodal lifestyle approach for patients with chronic pain (defined as experiencing debilitating pain for at least 3 months).4 Where do we fit-in exercise therapy and/or physical activity interventions, the core business of our profession? Here we provide a 6-step approach to integrate individually-tailored exercise therapy in a multimodal lifestyle approach for patients with chronic pain.
Goal setting and shared decision-making as the foundation for treatment adherenceDuring the clinical diagnostic process, the physical therapist identifies the factors that can influence the patient's body functions (e.g., mental functions, sensory functions and pain, neuromusculoskeletal and movement-related functions), activity limitations and participation restrictions, as well as the contextual (personal and environmental) factors,5 together providing key ingredients to individualize the exercise therapy and physical activity program. An important way to facilitate adherence to exercise and physical activity interventions in patients with chronic pain is value-based goal setting, defined as a target that the patient and therapist will work toward, implying patients choosing (time-)specific, attainable functional targets (e.g., being able to run 5 miles or to bring the children to school by bike). Compared to therapist-led exercise therapy, the use of value-based goal setting has been shown to enhance exercise therapy adherence in patients with low back pain.6 Once the patient defines its own valued, functional goals, the therapist can design the exercise therapy and physical activity program in a context that is specific to the patient's situation and hence allows attaining those goals. This is a motivating way to individually tailor the intervention, and an excellent way to motivate patients throughout. Value-based goal setting is also important to foster a productive relationship where the patient feels believed and cared for, which can be enhanced by behaviors such as active listening to and validating the patient's pain experience, and expressing empathy for the patient.7 This builds the therapeutic alliance, which sets the stage for productive, shared discussions about pain treatment (Fig. 1). Shared decision making implies that the therapist offers and informs the patient about (the nature and consequences of) treatment options that include the patient's preferences as well as best-evidence treatment options, in order to reach mutual agreement on the treatment.7 Hence, the therapist needs to question the patient's preferences regarding treatment content and outcome prior to initiating the shared decision making process. Cognitive dissonance between patient and therapist – the uncomfortable tension created through inconsistent (treatment) beliefs - can be resolved through shared decision making. In addition, such a shared decision-making process is not only relevant for discussing whether or not to exercise, it also applies to combining exercise therapy/physical activity with tackling other lifestyle factors, which is explained in the next section.
Pain science education, nutritional care, stress and sleep management to optimize exercise therapy in patients with chronic painFirst, it is important to emphasize that not all patients require pain science education and stress, sleep, and dietary interventions, while nearly all patients with chronic pain visiting a physical therapist are likely in need of, and will benefit from, exercise therapy and/or physical activity interventions. Second, for clinicians it can be helpful to consider interventions improving pain beliefs, stress tolerance, sleep, and diet as preparatory for exercise therapy or physical activity interventions. Indeed, maladaptive pain beliefs can prevent patients with chronic pain to engage and adhere to exercise and physical activity programs, while helpful beliefs allows them to cope appropriately with possible side effects such as pain flares.8 Any exercise bout or physical activity is a (healthy) stressor, implying that improved stress tolerance will facilitate patients to cope better with (incremental) exercise programs, including dealing with possible pain flares or any other temporary discomfort associated with exercise programs or physical activity. On the other hand, exercise and physical activity programs will improve patients’ stress tolerance, creating a synergistic effect between stress management and exercise therapy for patients with chronic pain.
Sleep is essential for many physiological functions, including the body's capacity to meet the metabolic demands of, and optimal recovery from exercise bouts and physical activity.9 Patients with sleep problems are unlikely to benefit optimally from any exercise intervention (e.g., sleep is essential for motor memory consolidation10). Dietary intake of sufficient nutrients is essential for allowing the human body to exercise, while dietary strategies are becoming increasingly recognized as potential strategies to optimize training effects and recovery from exercise interventions, at least in non-chronic pain populations.11 Finally, time-restriction to exercise and physical activity bouts (i.e., not in the hours before going to bed), stress exposure (e.g., preferentially in the morning when cortisol levels are high), and dietary intake (e.g., prioritize carbohydrate, fat, and protein intake during breakfast & lunch) are promising candidates to reprogram the disrupted circadian rhythm in patients with sleep disorders,9 illustrating the complex interplay between various lifestyle factors.
Taken together, depending on the relevant combination of lifestyle factors to address in individual patients with chronic pain, as well as the patient's activity limitations, participation restrictions, contextual factors, and value-based goal setting, a combination of pain science education, nutritional care, stress management, and/or sleep management can optimize the conditions for any exercise or physical activity program (Fig. 1). That does not imply per se that patients should complete all those interventions prior to commencing an exercise or physical activity program. On the contrary, except for pain science education, which is typically given prior to exercise therapy,8 addressing lifestyle factors such as stress, sleep, and nutrition can be combined alongside (grading) exercise and physical activity programs for patients with chronic pain. Examples on how such lifestyle interventions can be integrated in exercise interventions for patients with chronic pain are available elsewhere in published treatment manuals.12-14 The next section will focus on the content of the exercise therapy and physical activity intervention for patients with chronic pain.
How to exercise patients with chronic pain: individual tailoring of activities that are avoided versus persistedIndividual tailoring of exercise therapy and physical activity for patients with chronic pain implies a careful selection of the appropriate type of exercise therapy or physical activity intervention, considering that patients with chronic pain often combine (context-specific) avoidance and persistence (or overactivity) behaviors to deal with their condition within their life.15,16 For instance, let's consider a patient with neck pain who stopped their running routine (i.e., avoidance behavior out of fear of causing more harm to their neck due to running), yet continued their professional and household activities (i.e., persistence behavior due to motivational or contextual factors related to their perceived roles in life, and despite experiencing frequent neck pain flares during and in response to these activities). If the patient is willing to return to their running routine (i.e., running is part of their goal setting), behavioral graded activity and exposure in vivo are valid options. The choice between behavioral graded activity and exposure in vivo is made by questioning the reasons for quitting running, and asking to rate the threatening nature of running (i.e., threatening in a way that it might cause more harm to their neck) on a scale from 0 to 100, with 0 reflecting not threat at all, and 100 an unbearable threat.17 If they score running below 70/100, behavioral graded activity is an effective approach that will allow them to return to their running routine (Fig. 1).18,19
Behavioral graded activity applies the concept of operant conditioning to increase the level of physical activity in the patient's daily life.20 It is a highly personalized approach targeting the patient's self-defined, specific, treatment goals (value-based goal setting), with individual tailoring of baseline and grading levels for performing these daily activities by addressing pain as a barrier to physical activity. Behavioral graded activity allows patients to shift from having priority in pain control to priority in valued life goals. Pain science education prepares patients for the time-contingent (“Go running for five minutes, regardless of the pain”), cognition-targeted approach to daily (physical) activity and exercise therapy employed in behavioral graded activity, replacing the classical disease-based symptom-contingent (“Stop running when it hurts”) approach. ‘Cognition-targeted’ implies regularly discussing the patient's perceptions about each activity or exercise, including anticipated consequences such as pain flares and more tissue damage, in a way that the patient develops a more positive attitude towards the physical activity and exercises. These time-contingent and cognition-targeted treatment principles are also applied in cognition-targeted exercise therapy,8 where new exercises are graded from low-threatening (i.e., motor imagery) to gradually more threatening and with increasing complexity in different environments and contexts in order to maximize the transfer to daily situations.21
In case the patient with neck pain scores the threatening nature of running higher than 70/100, designing specific behavioral experiments within an exposure in vivo approach22 is indicated, as such high-threatening activities are difficult to address using a behavioral graded activity approach. The aim of the behavioral experiments within an exposure in vivo approach is to challenge the patient's harm expectancies related to the specific activities or body movements in preparation of performing the feared activity or movement function, including discussing the anticipated consequences (e.g., the jerking while running might further damage my neck). By challenging the patient's anticipated consequences and reassuring the safety of the activity/exercise, the patient is prepared to execute the feared activity or body movement function. Performance of the feared activity or body movement typically violates the patient's expectancies, which are discussed with the therapist to reinforce learning new associations (e.g., running does not damage my neck, and even though it might trigger a bit more pain, it's a safe and healthy activity, making my neck stronger).
Contrary to avoided activities, activities that persist should not be included in any type of graded exercise and activity interventions. This is also in line with step 1 of value-based goal setting, as persistence behavior implies that the patient is currently able to perform the activity. Instead, activities that are avoided require pacing activity self-management and acceptance-based interventions.17 Pacing activity self-management implies teaching the patient to spread the activity over multiple shorter bouts and insert breaks (‘recovery periods’) where they can practice the proposed relaxation skills or any other stress-coping strategy that can facilitate acceptance (e.g., acceptance of pain during and in response to activity).23 This way, step 4 (‘improving relevant lifestyle factors to optimize exercise conditions’) is followed-up in step 6 (‘providing exercise therapy and physical activity intervention’).
Can patients become & stay pain-free following exercise therapy?Treatment expectations impact treatment outcomes, implying that patient should be informed upfront what they can expect from exercise therapy/physical activity programs. Is it realistic to aim for full pain relief following exercise therapy? That is likely to depend on many factors, including the pain condition. While patients with fibromyalgia rarely experience complete pain relief in response to exercise therapy, patients with chronic neck or low back pain can expect it. In a multicenter trial, 38% of patients with chronic spinal pain receiving pain science education combined with cognition-targeted exercise therapy experienced complete pain relief (i.e., 0 or 1 out of 10 on a pain severity scale) at the end of the treatment, and the mean percentage pain improvement was 50%.8
ConclusionThe individually tailored exercise therapy and physical activity interventions as explained here are applicable in many, if not all, chronic pain conditions, including neck pain, low back pain, osteoarthritis, fibromyalgia, headache, shoulder pain, neuropathic pain, and post-cancer pain. This way, exercise therapy and physical activity interventions facilitate the paradigm shift from a tissue- and disease-based pain management approach towards multimodal lifestyle interventions for patients with chronic pain.24 The paradigm shift aligns with a modern way to teach and practice our profession, including focusing on active, person-empowering interventions delivered in a contextualized healing environment with a well-developed patient-practitioner allience.25 Still, more research is needed, including studies using real world data, big data analysis based on artificial intelligence, practice-based evidence, and pragmatic trials. Although many of the ingredients of the proposed exercise therapy and physical activity interventions for patients with chronic pain are supported by clinical trial evidence (e.g., behavioural graded activity,18,19 cognition-targeted exercise therapy,8 exposure in vivo18), multicenter clinical trials examining the comprehensive multimodal lifestyle approach for chronic pain as proposed here are needed. This notion is supported by the recently established evidence and gap map stressing the need for increased focus on interventions encompassing the entire biopsychosocial perspective in patients with chronic pain.26