Multisensory interventions, such as auditory-tactile-visual-vestibular intervention (ATVV), tactile-kinesthesic stimulation (TKS), and the kangaroo mother care (KMC), have been commonly applied in hospitalized preterm infants.
ObjectiveTo investigate the effectiveness of the ATVV, the TKS, and the KMC combined to standard care compared to standard care in the length of hospital stay and weight gain of hospitalized preterm infants.
MethodsPubMed, Scopus, Web of Science, Embase, SciELO Citation Index, CINAHL, Cochrane, and LILACS databases were searched from the inception to May 06, 2022 without language restrictions. We included randomized controlled trials. Two independent reviewers selected studies and extracted information about participants, interventions, outcomes, and the risk of bias. The body of evidence was synthesized through GRADE. Data were pooled using a random-effects model.
ResultsSixty-three randomized clinical trials included a range of 20–488 preterm infants (gestational age=25 to <37 weeks). Evidence was low to very low due to risk of bias, inconsistency, and imprecision. Most studies presented some concerns about methodological quality. The ATVV and the KMC increased weight gain. The TKS reduced the number of days at the hospital and increased the daily weight gain and the total weight gain.
ConclusionsAdding ATVV, TKS, or KMC to standard care was more effective than standard care alone to improve weight gain. Only the TKS combined with standard care was more effective than standard care alone to reduce the length of hospital stay.
Studies have shown that the neonatal intensive-care unit (NICU) environment might present abnormal sensory stimulation.1 Usually, visual and hearing systems are overstimulated, while tactile and vestibular systems are under stimulated. Preterm infants have immature sensory systems and present limited capacity to self-regulate. They are, therefore, influenced by the NICU environment.2 The deprivation of normal, or the presence of abnormal, sensory stimulation might disrupt brain development, especially during the first year of life when critical periods for the maturation of sensory systems are active.2
Systematic reviews have recommended sensory stimulation for preterm infants.3-5 This type of intervention has been applied in the NICU.3 During the multisensory intervention, therapists stimulate two or more sensory systems. Studies have shown that the multisensory intervention improved the behavioral state organization, the feeding progression, and the general development of the infants. Also, this type of intervention reduced maternal stress.6-8
One of the primary aims of multisensory stimulation is to supply sensory enrichment for infants exposed to environments with a low level of sensory stimuli, such as the NICU. The aim is to improve brain connectivity and maturation.9,10 Also, the multisensory intervention aims to reduce overload or inappropriate stimuli,11 reducing stressors. One of the physiological mechanisms that supports the application of this type of intervention is the mechanism of stress reduction.12 It has been shown that tactile stimulation and mother-infant interaction increase oxytocin levels in the brain, increasing well-being.12
The length of hospital stay and weight gain have been recognized as important variables for hospitalized preterm infants. Studies found that prolonged hospitalization has been associated with decreased mother-infant interaction, grieving parents, and failure to thrive.13,14 Studies have also shown that weight gain is associated with reduced morbidity,15 decreased hospital readmissions,16 and decreased neurodevelopmental deficits.16 The knowledge of the effects of the multisensory intervention on these variables is, therefore, relevant.
Three multisensory interventions have been commonly applied in clinical practice: auditory-tactile-visual-vestibular (ATVV) intervention,17 tactile-kinesthesic stimulation (TKS),18 and the kangaroo mother care (KMC)19 or skin to skin contact.20 This review investigated the effectiveness of ATVV, TKS, and KMC combined with standard care compared to standard care alone in the length of hospital stay and the weight gain of hospitalized preterm infants. This study will provide an update of the clinical evidence for the practice of health professionals working with early intervention and sensory stimulation of preterm infants.
MethodsProtocol and registrationThis meta-analysis followed the recommendations proposed by Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).21
Eligibility criteriaWe did not restrict the search strategy to a specific language. To be included, a publication needed to be a randomized and parallel controlled trial assessing the effects of multisensory stimulation combined to standard care compared to standard care alone on length of hospital stay or weight gain of healthy stable hospitalized infants born at less than 37 weeks of gestational age.
The multisensory interventions, which combined two or more sensory stimuli, considered in this review were the following: the ATVV, the TKS, and the KMC.
The length of hospital stay was defined as the number of days from the randomization to hospital discharge or the NICU discharge. The weight gain was divided into three measures: a) final weight, defined as the weight at discharge from hospital or at the end of the study (grams), b) daily weight gain from randomization until hospital discharge or the end of the study (days), c) total weight gain, defined as the difference between the start and final weight (grams).
Exclusion criteria were: a) quasi-experimental studies in an attempt to obtain more valid conclusion for this review, b) studies that did not report outcomes for preterm infants separately from those for full-term infants, c) studies that assessed preterm infants at risk for developmental delay, including neurological disorders or environmental exposure risks, d) studies that applied interventions that did not focus on sensory stimulation, e) studies that applied the sensory stimulation as a secondary treatment, f) studies that applied multisensory intervention only once, g) studies that applied the reduction of external stimuli, h) studies that applied breastfeeding interventions, oral-motor stimulations, and massage therapy using only tactile stimulation because these interventions are based on the stimulation of only one sensory system, and i) studies that applied therapeutic touch involving non-touch or energy-balancing techniques.
Search methodsThe following electronic databases were searched: PubMed, Scopus, Web of Science, Embase, SciELO Citation Index (Web of Science), CINAHL, Cochrane Library, and LILACS (BIREME). The search occurred from the inception date of each database until May 6, 2022. The search strategy used combined medical subject heading (MeSH) terms and text words related to population (preterm and infant), intervention (multisensory, multimodal, auditory-tactile-visual-vestibular (ATVV), massage, tactile-kinesthesic, kangaroo care, skin to skin contact), location of intervention (hospital, NICU), and type of study (clinical trial, randomized).
An example of the combination of terms used with PubMed is: ((((((Preterm*) OR (Premature)) OR (Premature Birth[MeSH Terms])) AND ((((Infant*) OR (Infant[MeSH Terms])) OR (Newborn)) OR (Infant, Newborn[MeSH Terms]))) AND (((((((((ATVV) OR (Tactile-kinesthesic)) OR (“tactile kinesthesic”)) OR (massage)) OR (massage[MeSH Terms])) OR (kangaroo)) OR (Kangaroo-Mother Care method[MeSH Terms])) OR (skin-to-skin)) OR (“skin to skin”))) AND (((((hospital) OR (hospitalized)) OR (hospitals[MeSH Terms])) OR (“Neonatal Intensive Care Units”)) OR (Intensive Care Units, Neonatal[MeSH Terms]))) AND ((((Randomized) OR ("clinical trial")) OR (Randomized Controlled Trials as Topic[MeSH Terms])) OR (clinical trial[MeSH Terms]).
We also searched for additional articles in the list of the references from 15 review studies17,18,20,22-33 found in the electronic search and the list of references from the included studies. All duplicated papers were removed, and then two reviewers (GPR, BABR) independently selected the studies according to inclusion criteria. In the case of any disagreement, a third reviewer (ANS) arbitrated. We used the State of the Art through Systematic Review (START) software34 for study selection.
Data extraction and quality assessmentTwo review authors (GPR, BABR) independently extracted and compiled the study data using a spreadsheet from the Excel program. A third reviewer (ANS) resolved disagreements. We extracted the following information from the included studies: study country, the characteristics of the participants (number of subjects, age, and sex), the outcome studied, the characteristics of treatment (technique/approach, frequency and dosage, delivery method, and duration), and results. The mean and standard deviation of data of interest were extracted, when available. When data were not available, we contacted the corresponding author to request information by e-mail.
We evaluated the risk of bias of included studies using the Cochrane Handbook for Systematic Reviews of Interventions.35 We verified the following features: randomization process, deviations from the intended interventions, missing outcome data, measurement of the outcome, and selection of the reported results. Each item and the overall bias were classified as low risk, high risk, or some concerns.7 Two review authors (GPR, ANS) independently rated the risk of bias. In the case of any disagreement, the authors discussed and reached a consensus.
Data synthesis and analysisWe used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) method to verify evidence synthesis, assessing: risk of bias, inconsistency of results, indirectness, imprecision, and publication bias.36 The level of evidence for risk of bias was downgraded by one level if 25% to 50% of the included studies were classified as high risk of bias or most studies were classified as some concerns, and downgraded by two levels if more than 50% of the included studies were classified as high risk of bias. The level of evidence for inconsistency was downgraded by one level if the I2 test was greater than 50%, or there was a high variation on the size of the effect between the included studies, or if there was high heterogeneity regarding the content of the intervention between the included studies; and downgraded by two levels if there was a combination of these factors. The level of evidence for indirectness was downgraded by one level if more than 50% of participants varied from the population of interest. The level of evidence for imprecision was downgraded by one level if the confidence intervals were too wide or the sample size was less than 400 participants.37 The level of evidence for publication bias was downgraded by one level if publication bias was identified by visual inspection of funnel plots for outcomes that included more than 10 studies. The level of evidence was classified as: high (enough evidence in the estimate of the effect), moderate (the true effect is close to the estimate of the effect), low (the confidence of the effect is limited), and very low evidence (little confidence of the effect estimate). A high or moderate level of evidence represented a strong recommendation for use of the intervention.38 A summary of findings table was produced using GRADEpro software (McMaster University, Hamilton, Canada).
Meta-analysis was conducted using RevMan 5.1 (Cochrane Collaboration, Oxford, England). Effect sizes are reported as the mean difference (MD) with 95% confidence interval (CI) for each study and outcome. Pooled treatment effects were calculated across trials by using a random-effects model.39 We verified heterogeneity among studies using the I2 statistic.39
Role of the funding sourceThe funding sources played no role in the design, conduct, or reporting of this study.
ResultsSearch strategyThe search resulted in 63 randomized clinical trials that met the full inclusion criteria.8,40-101 Fifty-four were included in the meta-analysis (Supplementary material Figure 1).
Description of participants and outcomesStudies included medically stable preterm infants. The sample size varied from 20 to 488. Most of the included studies evaluated preterm infants with gestational age between 28 and 35 weeks. Studies included hospitalized infants from birth to two months old (Table 1).
Description of each included study: participants, country, outcome, intervention.
| Study | Participants GA: weeks Sex: boy/girl | Country | Outcome | Control | Intervention | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Content | Frequency and Dosage | Delivery Method | Content | Frequency and Dosage | Delivery Method | Duration | ||||
| Frequency and Dosage | Delivery Method | Content | Frequency and Dosage | Delivery Method | Duration | |||||
| Auditory–Tactile–Visual-Vestibular Intervention | ||||||||||
| Brown et al.40, 1980 | GA: <37 Sex: 19/21 | USA | hospital stay | SC | Daily | Professionals | ATVV | 2X/day, 30 min, 5 days/week | Professionals | hospital discharge |
| Kanagasabai et al.41, 2013 | GA: 28–36 Total: 50 | India | hospital stay | SC: Kangaroo, breast feeding | Daily | Professionals | ATVV | 1X/day, 12 min, 5 days/week | Professionals | hospital discharge |
| Nasimi et al.42, 2016 | GA: 32–36 Total: 80 | Iran | final weight, total weight gain | SC: eat and sleep | Daily | Professionals | STMT | 1X/day, 12 min, 5 days/week | Mother | hospital discharge |
| Resnick et al.43, 1987 | GA: mean = 31.5 Sex: 96/125 | USA | hospital stay | SC | Daily | Professionals | ATVV + kinesthesic + oral | Daily | Mother | hospital discharge |
| Standley44, 1998 | GA: 27 - 34.5 Total: 40 | USA | hospital stay, daily weight gain | SC: feeding, neurologic organization, kangaroo, reduce overstimulation | Daily | Professionals | ATVV + music | 1–2X/day, 15–30 min | Professionals | hospital discharge |
| Vaivre-Douret et al.45, 2009 | GA: 31–34 Sex: 24/25 | France | hospital stay, total weight gain | SC | Daily | Healthy professionals | STMT + oils | 2X/day, 15 min | Professionals | 10 days |
| Walworth et al.46, 2012 | GA: 32–36 Sex: 108/92 | USA | hospital stay, daily weight gain | SC | Daily | Professionals | ATVV + music | At least 1X/week, 20 min | Professionals | hospital discharge |
| White-Traut et al.47, 1986 | GA: 29–35 Sex: 18/15 | USA | hospital stay, daily weight gain | SC: Feedings, handling, nonnutritive sucking, visual stimulation | Daily | Professionals | ATVV | 1X/day, 15 min | Professionals | hospital discharge or 10 days |
| White-Traut et al.8, 2002 | GA: 23–26 Sex: 18/19 | USA | hospital stay | SC: Stress reduction | Daily | Professionals | ATVV | 2X/day, 15 min, 5 days/week | Professionals | hospital discharge |
| White-Traut et al.48, 2015 | GA: 29–34 Sex: 87/95 | USA | hospital stay, total weight gain | SC: feedings, nursery care, education of parents | Daily | Professionals | ATVV | 2X/day, 15 min | Mother or nurse | hospital discharge |
| Zeraati et al.49, 2018 | GA: 32–36 Total: 80 | Iran | hospital stay | SC | Daily | Professionals | ATVV | 1X/day, 12 min, 5 days/week | Mother | hospital discharge |
| Tactile –Kinesthesic Syimulation (TKS) | ||||||||||
| Ang et al.50, 2012 | GA: 28–33 Sex: 48/72 | USA | hospital stay, final weight, daily weight gain | SC | Daily | Professionals | TKS | 3X/day, 15 min, 5X/week | Professionals | 4 weeks or hospital discharge |
| Diego et al.51, 2005 | GA: mean = 29 Sex: 14/20 | USA | hospital stay, daily weight gain | SC | Daily | Professionals | TKS | 3X/day, 15 min | Professionals | 5 days |
| Diego et al.52, 2007 | GA: mean = 29 Sex: 40/40 | USA | hospital stay, daily weight gain | SC | Daily | Professionals | TKS | 3X/day, 15 min | Professionals | 5 days |
| Dieter et al.53, 2003 | GA: 25–34 Total: 32 | USA | hospital stay, total weight gain, daily weight gain | SC | Daily | Professionals | TKS | 3X/day, 15 min | Professionals | 5 days |
| Elmoneim et al.54, 2021 | GA: <32 Sex:33/27 | Egypt | total weight gain, daily weight gain | SC | Daily | Professionals | TKS | 3X/day, 15 min | Professionals | 5 days |
| Ferber et al.55, 2002 | GA: 26–34 Total: 40 | Israel | total weight gain | SC | Daily | Professionals | TKS | 3X/day, 15 min | Mothers or Professionals | 10 days |
| Field et al.56, 1986 | GA: mean = 31 Total: 40 | USA | hospital stay, final weight, total weight gain, daily weight gain | SC: feeding | Daily | Professionals | TKS | 3X/day, 15 min | Professionals | 10 days |
| Field et al.57, 2008 | GA: mean = 34.6 Total: 42 | USA | hospital stay, daily weight gain | SC | Daily | Professionals | TKS | 3X/day, 15 min | Professionals | 5 days |
| Freitas et al.58, 2010 | GA: 26–36 Total: 32 | Brazil | hospital stay | SC | Daily | Professionals | TKS | 3X/day, 15 min | Professionals | 5 days |
| Fucile et al.59, 2010 | GA: 26–32 Sex: 27/11 | USA | daily weight gain | SC | Daily | Professionals | TKS | 2X/day, 15 min | Professionals | 14 days |
| Guzzetta et al.60, 2009 | GA: 30–33 Total: 20 | Italy | total weight gain | SC: Minimization of stress, classical music all day | Daily | Professionals | TKS + music | 3X/day, 15 min, 5X/week | Professionals | 4 weeks of age |
| Haley et al.61, 2012 | GA: average=31 Sex: 18/22 | USA | daily weight gain | SC | Daily | Professionals | TKS | 2X/day, 20 min, 6X/week | Professionals | 2 weeks |
| Hernandez-Reif et al.101, 2007 | GA: 28–32 Sex: 9/23 | USA | hospital stay | SC | Daily | Professionals | TKS | 3X/day, 15 min | Professionals | 5 days |
| Ho et al.62, 2010 | GA: 25–34 Sex: 13/7 | China | total weight gain, daily weight gain | SC and gentle touch | Daily | Professionals | TKS | 1X/day, 15 min, 5X/week | Professionals | 38 weeks PCA |
| Karamiam et al.99, 2022 | GA: < 37 Sex: 71/60 | Iran | final weight | SC | Daily | Professionals | TKS | 3X/day, 15 min | Professionals | 12 days |
| Lee63, 2005 | GA: < 36 Sex: 10/16 | South Korea | hospital stay, final weight | SC | Daily | Professionals | TKS | 2X/day, 15 min | Professionals | 10 days |
| Liao et al.98, 2021 | GA: 28–37 Sex: 17/16 | Taiwan | final weight | SC | Daily | Professionals | TKS | 3X/day, 15 min | Professionals | 7 days |
| Massaro et al.64, 2009 | GA: = 32 Total: 175 | USA | hospital stay, final weight, daily weight gain | SC | Daily | Professionals | TKS | 2X/day, 15 min | Professionals | hospital discharge |
| Mathai et al.65, 2001 | GA: mean = 34 Total: 50 | India | daily weight gain | SC | Daily | Professionals | TKS | 3X/day, 15 min | 5 days | |
| Health profesionals and mother | ||||||||||
| Matricardi et al.66, 2013 | GA: 25–31 Total: 42 | Italy | hospital stay | SC: assist care, kangaroo-care, physical therapy | Daily | Professionals | TKS + oil | 2X/day, 10 min | Health Professional or researchers | hospital discharge |
| Mendes et al.67, 2008 | GA: mean = 29 Sex: 52/52 | Brazil | hospital stay, final weight, daily weight gain | SC | Daily | Professionals | TKS | 4X/day, 15 min | Mother | hospital discharge |
| Montaseri et al.68, 2020 | GA: 30–36 Total: 30 | Iran | final weight, total weight gain | SC | Daily | Professionals | TKS | 2X/day, 10 min | Health Professional or researchers | 5 days |
| Moyer-Mileur et al.69, 2013 | GA: 28–33 Sex: 22/22 | USA | final weight, daily weight gain | SC | Daily | Professionals | TKS | 2X/day, 20 min | Health Professional or researchers | 4 weeks |
| Scafidi et al.70, 1986 | GA: mean = 31 Total: 40 | USA | hospital stay, final weight, daily weight gain | SC: feeding, parent visit with touch | Daily | Professionals | TKS | 3X/day, 15 min | Health Professional or researchers | 10 days |
| Scafidi et al.71, 1990 | GA: mean = 30 Total: 40 | USA | hospital stay, final weight, daily weight gain | SC: feeding, weaning from the isolette | Daily | Professionals | TKS | 3X/day, 15 min | Health Professional or researchers | 10 days |
| Smith et al.72, 2013 | GA: 28–32 Sex: 18/19 | USA | final weight | SC | Daily | Professionals | TKS | 2X/day, 20 min | Health Professional or researchers | 29 days |
| White et al.73, 1976 | GA: < 36 Total: 12 | USA | hospital stay | SC | Daily | Professionals | TKS | 4X/day, 15 min, | Health Professional or researchers | Day 2 to day 11 |
| Zhang et al.74, 2018 | GA: 30–34 Total: 112 | China | final weight | SC | Daily | Professionals | TKS | 2X/day, 15 min | Health Professional or researchers Mother | 2 weeks |
| Kangaroo or Skin-to-skin Contact | ||||||||||
| Acharya et al.75, 2014 | GA: mean = 32 Sex: 86/40 | Nepal | hospital stay, daily weight gain | SC + holding | Daily | Health Professional + mother | KMC | Daily, at least 6 h | Mother | hospital discharge |
| Baton et al.100, 2021 | GA: 28–36 Sex: 12/18 | Philippines | hospital stay, final weight | SC + incubator | Daily | Health Professional | KMC | Daily, 2 to 4 h | Mother or father | until extubated |
| Bier et al.76, 1996 | GA: 24–33 Total: 50 | USA | hospital stay, daily weight gain | SC + holding | Daily | Health Professional + mother | KMC | Daily | Mother | 10 days |
| Edraki et al.77, 2015 | GA: 32–36 Total: 60 | Iran | hospital stay | SC + conventional attachment | Daily | Health Professional + mother | KMC + massage + touch | Daily, 35 min | Mother | 4 days |
| Gathwala et al.78, 2008 | GA: mean=35 Total: 100 | India | hospital stay | SC + warmer or incubator | Daily | Professionals | KMC | Daily, 6 h | Mother | hospital discharge |
| Gathwala et al.79, 2010 | GA: mean=35 Total: 100 | India | daily weight gain | SC + warmer or incubator | Daily | Professionals | KMC | Daily, 6 h at maximum | Mother | hospital discharge |
| Ghavane et al.80, 2012 | GA: mean=31 Sex: 78/62 | India | hospital stay, final weight, daily weight gain | SC + warmer or incubator | Daily | Professionals | KMC | Daily, at least 8 h | Mother | hospital discharge |
| Kadam et al.81, 2005 | GA: mean=33 Total: 89 | India | hospital stay, final weight | SC + radiant warmer | Daily | Professionals | KMC | Daily, at least 1 h | Mother | hospital discharge |
| Miltersteiner et al.82, 2005 | GA: mean=32 Total: 35 | Brazil | hospital stay | SC + incubator + prone position | Daily | Professionals | KMC | Daily, at least 1 h | Mother | 7 days |
| Mörelius et al.83, 2015 | GA: 32–35 Sex: 17/20 | Sweden | final weight | SC + incubator | Daily | Professionals | KMC | Daily | Mother | Hospital discharge |
| Mwendwa et al.84, 2012 | GA: 26–36 Sex: 86/80 | Kenya | final weight, daily weight gain | SC + warmer or incubator | Daily | Professionals | KMC | Daily, 8 h | Mother | hospital discharge |
| Neu et al.85, 2013 | GA: 32–36 Sex: 39/48 | USA | hospital stay | SC + holding | Daily | Health Professional + Mother | KMC | Daily | Mother | 8 weeks |
| Ramanathan et al.86, 2001 | GA: 28–34 Sex: 18/10 | India | daily weight gain | SC + warmer or incubator | Daily | Professionals | KMC | 4hours/day | Mother | hospital discharge |
| Roberts et al87., 2000 | GA: 30–36 Total: 30 | Australia | hospital stay, daily weight gain | SC + holding | Daily | Professionals + Mother | KMC | Daily | Mother | hospital discharge |
| Rojas et al.88, 2003 | GA: mean = 27 Sex: 35/25 | USA | hospital stay, final weight, total weight gain, daily weight gain | SC + holding | Daily | Professionals + Mother | KMC | Daily | Mother | hospital discharge |
| Samra et al.89, 2015 | GA: 34–36 Sex: 22/8 | USA | hospital stay, final weight | SC + holding | 50 min, 3X/week | Professional + Mother | KMC | 50 min, 3X/week | Mother | hospital discharge |
| Sharma et al.90, 2016a | GA: mean=29.7 Sex: 74/67 | Colombia | hospital stay, final weight, daily weight gain | SC + optional skin-to-skin holding | Daily | Professionals | KMC | Daily, at least 6 h | Mother | hospital discharge |
| Sharma et al.91, 2016b | GA: mean=29.7 Sex: 34/28 | Colombia | hospital stay, final weight, daily weight gain | SC + warmer or incubator | Daily | Professionals | KMC | Daily, at least 6 h | Mother | hospital discharge |
| Sharma et al.92, 2017 | GA: mean=29.7 Sex: 40/39 | Colombia | hospital stay, final weight, daily weight gain | SC + warmer or incubator | Daily | Professionals | KMC | Daily, at least 6 h | Mother | hospital discharge |
| Tessier et al.93, 1998 | GA: mean=36 Sex: 236/252 | Colombia | hospital stay | SC + incubator | Daily | Professionals | KMC | Daily | Mother | hospital discharge |
| Wang et al.94, 2021 | GA: 33–36 Sex: 47/32 | China | final weight | SC | Daily | Professionals | KMC | Daily, 2.5 h | Mother | hospital discharge |
| Welch et al.95, 2013 | GA: 26–35 Sex: 77/73 | USA | hospital stay, final weight | SC + optional skin-to-skin holding | Daily | Professionals | KMC | Daily, 6 h | Parents | hospital discharge |
| Weller et al.96, 2002 | GA: 26–36 Sex: 35/52 | Colombia | hospital stay | SC + incubator | Daily | Professionals | KMC | Daily, 6 h | Parents | hospital discharge |
| Whitelaw et al.97, 1988 | GA: 25–36 Sex: 35/36 | England | hospital stay | SC + holding | Daily | Health Professional + Mother | KMC | Daily, as long as possible | Mother | hospital discharge |
ATVV, Auditory–Tactile–Visual-Vestibular Intervention; GA, gestational age; KMC, kangaroo mother care; SC, standard care; TKS, tactile-kinesthesic stimulation.
Forty-three (68%) studies assessed length of hospital stay. Twenty-three (37%), 30 (48%), and 11 (17%) studies assessed, respectively, the final weight, the daily weight gain, and the total weight gain (Table 1).
Description of interventionsEleven (17%) studies applied multimodal stimulation.8,40-49 Nine studies applied the ATVV, which included sensory stimuli such as female voice or soft lullaby song, light stroking all over the body, eye-to-eye contact or black and white cards, and rocking. One study applied the auditory-vestibular stimulation, using rocking waterbeds, taped simulated heartbeat, and a woman's voice. Two studies applied the STMT intervention that includes the use of a water mattress (vestibular), massage (tactile), active changes of position (kinaesthetic), soft music and verbal contact (auditory), and eye-to-eye contact (visual). The control group received the standard care of each hospital. Three studies specified the application of kangaroo care as part of their standard care, and two studies the application of visual stimulation. All the infants in the multimodal stimulation group also received standard care (Table 1).
Twenty-eight (44%) studies applied TKS50-74,98,99,101 which is a form of infant massage that includes kinesthetic movement. The tactile portion consisted of the application of moderate strokes to the infant. The kinesthesic part consisted of extension and flexion movements of the upper and lower limbs. One study combined TKS with classical music, and one study applied oil during massage. The control group received the standard care of each hospital. Two studies specified the application of kangaroo care as part of their standard care, two studies the application of gentle touch, and one the application of classical music. All the infants in the TKS group also received standard care (Table 1).
Twenty-four (38%) studies applied the KMC or skin-to-skin contact.77-97,100 The main component of KMC is skin-to-skin contact. During the skin-to-skin contact, the parent holds the infant in an upright position, closer to their chest. The KMC also includes breastfeeding. One study associated KMC with massage and touch. One study combined KMC with music, and one study with a calming touch. Both kangaroo and control groups received the standard care of each hospital. The infants from the control groups were kept inside an incubator or a warmer room in 11 studies. The parents applied the traditional holding to the infants of the control group in five studies. In two studies, the parents from the control group were educated about the kangaroo method and had the option to apply or not (Table 1). All the infants in both groups also received standard care.
Risk of bias of individual studiesThe risk of bias of the 63 eligible trials are described in supplementary material Figure 2. We found that 12 studies (19%) were classified as low risk, 30 (48%) as some concerns, and 21 (33%) as high risk.
The main methods limitations across studies were that 45 studies (71%) did not report the randomization process or did not use or inform about concealed allocation, and 22 (35%) did not inform about missing outcome. Because of the type of interventions, it was not possible to blind therapists and participants. Most studies did not blind assessors or provide information about blinding. Because the outcome length of hospital stay reflects decisions made by the intervention provider, we classified the studies as presenting some concerns regarding the influence of the non-blinding of the assessor. Because weight gain is an observer-reported outcome not involving judgment, we classified the studies as presenting low risk regarding the influence of the non-blinding of the assessor. Studies had different designs, convenience samples, and included small sample sizes (supplementary material Figure 2).
Synthesis of resultsFifty-three (84%) studies provided means and standard deviations to input in the meta-analysis. We estimated the standard deviation based on means and p values for the length of hospital stay in three studies,47,71,74 and for the daily weight gain in three studies.47,72,74
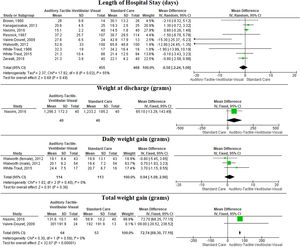
Auditory–tactile–visual-vestibular interventionWe included 10 studies8,40-43,45-49 that compared the effects of ATVV combined to standard care to only standard care. There is low-quality evidence (downgraded due to risk of bias and inconsistency) that adding ATVV to standard care may increase total weight gain (MD = 72.7 g, 95% CI: 68.3, 77.2; n = 114, 2 trials, I2 = 0%) at post intervention when compared to standard care alone (Fig. 1, Table 2). In addition, there is low-quality evidence (downgraded due to risk of bias and imprecision) that ATVV combined with standard care may not reduce length of hospital stay (MD = −0.6 days, 95% CI: −2.2, 1.1; n = 923, 9 trials, I2 = 55%) compared to standard care alone and there is very low-quality evidence (downgraded due to risk of bias, inconsistency, and imprecision) that ATVV combined with standard care may have little to no effect on daily weight gain (MD = 0.9 g, 95% CI: −1.1, 3.0; n = 227, 2 trials, I2 = 0%) (Fig. 1, Table 2) compared to standard care alone. Only one study assessed the final weight.
Summary of the evidence: certainty assessment, summary of findings, and level of evidence for each outcome and intervention.
| Outcome | Certainty assessment | Number of patients | Anticipated absolute effects | Level of evidence | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Infants (studies) | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Multisensory | Standard care | Risk with standard care | Risk difference with multisensorial | |||
| ATVV | Length of hospital stay (days) | 923 (9 RCTs) | seriousa | seriousb | not serious | not serious | None | 455 | 468 | 0 | MD 0.6 lower (2.2 lower to 1.1 higher) | ⨁⨁○○ |
| LOW | ||||||||||||
| Daily weight gain (grams) | 227 (2 RCTs) | very seriousc | seriousb | not serious | seriousd | None | 114 | 113 | 0 | MD 0.9 higher (1.1 lower to 3.0 higher) | ⨁○○○ | |
| VERY LOW | ||||||||||||
| Total weigth gain (grams) | 114 (2 RCTs) | seriousa | not serious | not serious | Serious | None | 64 | 53 | 0 | MD 72.7 higher (68.3 higher to 77.2 higher) | ⨁⨁○○ | |
| LOW | ||||||||||||
| TKS | Length of hospital stay (days) | 570 (13 RCTs) | very seriousc | seriousb | not serious | not serious | none | 283 | 287 | 0 | MD 1.7 lower (3.2 lower to 0.2 lower) | ⨁○○○ |
| VERY LOW | ||||||||||||
| Final weight (grams) | 633 (11 RCTs) | seriousa | not serious | not serious | seriousd | none | 390 | 393 | 0 | MD 69.31 higher (4.65 lower to 143.28 higher) | ⨁⨁○○ | |
| LOW | ||||||||||||
| Daily weight gain (grams) | 682 (14 RCTs) | seriousa | seriousb | not serious | not serious | None | 338 | 344 | 0 | MD 3.3 higher (1.7 higher to 4.9 higher) | ⨁⨁○○ | |
| LOW | ||||||||||||
| Total Weigth gain (grams) | 182 (5 RCTs) | very seriousc | not serious | not serious | seriousd | None | 93 | 89 | 0 | MD 85.6 higher (35.5 higher to 135.6 higher) | ⨁○○○VERY LOW | |
| KMC | Length of hospital stay (days) | 1830 (17 RCTs) | seriousa | seriousb | not serious | not serious | None | 929 | 901 | 0 | MD 0.6 lower (2.1 lower to 0.8 higher) | ⨁⨁○○LOW |
| Final weight (grams) | 798 (10 RCTs) | not serious | not serious | not serious | not serious | None | 406 | 392 | 0 | MD 8.5 lower (25.8 lower to 42.9 higher) | ⨁⨁⨁⨁HIGH | |
| Daily weight gain (grams) | 841 (10 RCTs) | seriousa | seriousb | not serious | not serious | none | 428 | 413 | 0 | MD 3.2 higher (2.2 higher to 4.3 higher) | ⨁⨁○○LOW | |
ATVV, Auditory–Tactile–Visual-Vestibular Intervention; KMC, kangaroo mother care; MD, mean difference; RCTs, randomized controlled trials; TKS, tactile-kinesthesic stimulation.
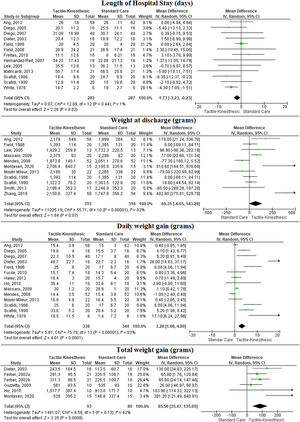
We included 32 studies50-64,66-74 that compared the effects of TKS combined to standard care to only standard care. There is very low-quality evidence (downgraded due to risk of bias and inconsistency) that adding TKS to standard care may reduce days at the hospital (MD = −1.7 days, 95% CI: −3.2, −0.2; n = 570, 13 trials, I2 = 1%), low-quality evidence (downgraded due to risk of bias and inconsistency) that it may increase daily weight gain (MD = 3.3 g, 95% CI: 1.7, 4.9; n = 682, 14 trials, I2 = 83%), and very low-quality evidence (downgraded due to risk of bias and imprecision) that it may increase total weight gain (MD = 85.6 g, 95% CI: 35.8, 135.6; n = 182, 6 trials, I2 = 42%) at post intervention when compared to standard care alone (Fig. 2, Table 2). In addition, there is a low-quality evidence (downgraded due to risk of bias and imprecision) that the TKS combined with standard care may have no effect on final weight when compared to standard care alone (MD = 57.3 g, 95% CI: −6.9, 121.5; n = 783, 12 trials, I2 = 82%) (Fig. 2, Table 2).
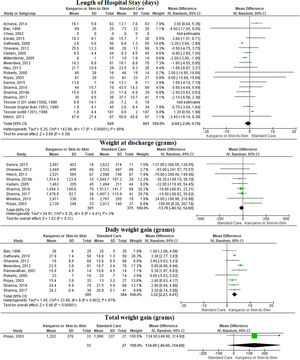
Kangaroo method care or skin-to-skin contactWe included 20 studies75-93,95 that compared the effects of KMC combined to standard care to standard care alone. There is low-quality evidence (downgraded due to risk of bias and inconsistency) that adding KMC to standard care may increase daily weight gain (MD = 3.2 g, 95% CI: 2.2, 4.3; n = 841, 10 trials, I2 = 64%), at post intervention when compared to standard care alone (Fig. 3, Table 2). We found there was low-quality evidence (downgraded due to risk of bias and inconsistency) that KMC combined with standard care may have no effect on length of hospital stay (MD = −0.6 days, 95% CI: −2.7, 0.8; n = 1830, 18 trials, I2 = 88%) compared to standard care alone and there is high-quality evidence that KMC combined with standard care does not increase final weight (MD = 8.5 g, 95% CI: −25.8, 42.9; n = 798, 10 trials, I2 = 28%) compared to standard care alone (Fig. 3, Table 2). Only one study assessed the total weight gain.
The summary of findings and the overall quality of evidence for the primary outcomes are described in Table 2.
DiscussionAccording to our findings, only TKS combined with standard care may reduce the length of hospital stay. One integrative systematic review did not find any clear result that sensory stimulation techniques improve outcomes in preterm infants in the NICU.5 Some studies have found that home health services are essential to facilitate pre- and post-discharge transition care from NICU to home. The availability of health professionals to provide home care and the contribution between health professionals and parents are facilitators of earlier discharge.102,103 Most of the included studies did not focus on parent education programmes and home health services, which might be a strong reason for no difference between multisensory intervention and standard care regarding length of hospital stay.
In general, our results suggest that the included interventions may increase weight gain. Systematic reviews reported similar results for massage,104 TKS,18 and KMC.105 The outcome lack of weight gain is one of the signs of poor growth that is easy to assess in clinical practice. Poor growth in preterm infants is related to subsequent deficits or delay in neurocognitive development.106,107 The types of multisensory stimulation included in this review, therefore, are recommended for hospitalized preterm infants.
Some limitations exist for the included studies. We classified the included studies as presenting some concerns or a high risk of bias, especially for the outcome length of hospital stay. Most of the studies did not blind assessors, which might lead to a biased ascertainment of outcomes.108 In addition, most of the included studies did not provide information regarding concealed allocation or reported if there were missing outcomes data. These could lead to bias in selection of the participants and result in prognostic differences between treatment groups.109,110 All of these methodological issues might have generated a biased estimate of the treatment effect.
We can cite several potential limitations of this review. First, we included studies with potential risk of bias. Second, we included only randomized clinical trials, and we did not search for gray literature potential, which could introduce publication bias. The inclusion of only randomized controlled trials, however, was an attempt to avoid the inclusion of lower-quality studies. Interventions were diverse, as were comparator usual care conditions. The results of this systematic review, therefore, should be considered with caution.
ConclusionThe addition of ATVV, TKS, and KMC interventions to standard care may be more effective than standard care alone to improve weight gain of hospitalized preterm infants. The TKS combined to standard care may also be more effective than standard care alone to decrease the length of hospital stay. The ATVV and the KMC combined to standard care were no more effective than standard care alone to decrease length of hospital stay. Future studies with larger sample sizes, low risk of bias, and detailed descriptions of interventions for the standard care group are necessary.
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance code 001.