Advanced lung disease is a chronic non-neoplastic disease that compromises activities of daily living. Treatment includes pulmonary rehabilitation and inspiratory muscle training. Studies have shown the effectiveness of inspiratory muscle training in lung disease patients, but literature is scarce on the patients’ perceptions about this topic.
ObjectiveTo explore the perceptions of patients with advanced lung disease about inspiratory muscle training.
MethodsQualitative study. Interviews were conducted using a semi-structured questionnaire regarding topics on the participation of patients in inspiratory muscle training and on daily activities performed before and after training. Interviews were transcribed and analyzed according to thematic content analysis.
ResultsTen patients (eight women and 2 men, ranging in age from 27 to 89 years) with inspiratory muscle weakness (maximal inspiratory pressure=44±13.9cmH2O) were included. Five patients were diagnosed with Chronic Obstructive Pulmonary Disease, two with bronchiectasis and three with pulmonary fibrosis. All patients completed at least 80% of the total training sessions. The reports were grouped into four thematic categories: (1) impact of inspiratory muscle training on breathlessness (e.g., “I wasn’t feeling as tired as I previously felt.”); (2) change in daily activities (e.g., “I needed to go to the supermarket, I felt less tired doing it.”); (3) improved mobility (e.g., “I could not stand for long periods […] walking, for example […] Now I stand more, I have more capability.”); and (4) increased communication (e.g., “More power, right? Even in speaking […] When I could, I felt my voice coming out better.”).
ConclusionThere were improvements in breathlessness, daily activities, mobility, and communication, which positively affected the psychological and social aspects of the patients.
Respiratory diseases are among the leading causes of death worldwide with 4 million people dying every year due to chronic respiratory conditions.1,2 Advanced lung disease (ALD) is a term used to define an extensive number of lung diseases, such as Chronic Obstructive Pulmonary Disease, bronchiectasis, idiopathic pulmonary fibrosis, pulmonary hypertension and others.3 ALD is defined as a chronic non-neoplastic lung disease that significantly compromises patients’ activities of daily living, and there are few options of treatment available.3 The diagnosis of ALD is based on the patient's clinical history, a physical examination, and the degree of functional incapacity. ALD is mostly defined using one major criterion: disabling dyspnea (Medical Research Council 2–4),4 and two or more minor criteria: forced expiratory volume at first second (FEV1)<35% of the predicted values for obstructive diseases; vital capacity (VC)<40% of the predicted values for restrictive diseases; carbon monoxide diffusing capacity (DLCO)<45% of the predicted values; hypoxemia and/or hypercapnia; cor pulmonale; weight loss>10% within 6 months; heart rate at rest of approximately 100bpm or 6-min walking distance<350m.5
Pulmonary rehabilitation (PR) is one of the possible treatments suggested for patients with ALD to improve their physical, mental, emotional and social condition and promote long-term adherence to health-enhancing behaviors.6,7 The American Thoracic Society (ATS) and the European Respiratory Society (ERS) define PR as an intervention based on the patient's evaluation followed by therapies that include physical exercise, education, and behavioral change.6,7 One of the most important aspects of PR is the evaluation of the patient before his/her enrollment in the program. An important part of the evaluation is the process of diagnosing the respiratory muscle dysfunction by assessing the peripheral and respiratory muscle strength and endurance.8 Inspiratory muscle weakness is commonly found in patients with respiratory diseases9 and could lead to dyspnea10 and a reduction in exercise capacity.11 The ATS and ERS suggest that the inspiratory muscle training (IMT) should be considered an additional intervention to the PR program, especially in patients with inspiratory muscle weakness.6,8 The IMT can improve muscular strength and endurance of inspiratory muscles, dyspnea (decrease), exercise capacity, and quality of life in patients with obstructive and restrictive lung diseases.12,13
The benefits of PR and IMT in the treatment of patients with ALD are discussed in the literature12–14; however, there is limited literature on the patients’ perceptions of the effects of therapies and how those improvements relate to lifestyle changes. William et al.15 evaluated the effects of PR from the perspective of patients with COPD, and the results showed an increased confidence in relation to dyspnea with less fear and panic in moments of breathlessness and when doing physical activities. Furthermore, there was an increase in mobility, daily contact, and social interactions with less loneliness.15 Other studies evaluated the perceptions of PR in patients with pulmonary chronic diseases and showed that PR can increase patients’ confidence on mobility, social interactions, and performance of activities as well as improve the capacity to cope with the disease with less frustration and more confidence.16,17 Considering the perceptions of the patients when providing PR has also been shown to improve patients’ self-efficacy and adherence to treatment.18
Although some studies already elucidated the effects of PR from the patients’ perspective, to the best of our knowledge, this perspective in relation to IMT has not previously been studied. Therefore, the aim of this study was to explore the perceptions of patients regarding IMT.
MethodsThe methodological qualitative design was chosen to uncover patients’ perceptions about the IMT. The Research Ethics Committee of the Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, Minas Gerais, approved this study (CAAE – 40228314.4.0000.5149) and all patients provided their written consent before study enrollment.
SettingThis study was conducted in a research laboratory, and patients were referred from their chest physician and were included in the study if they met the eligibility criteria. All patients were followed up at the University Hospital.
ParticipantsThe patients who performed IMT from June to December 2015 were invited to participate in the interview. The patients were included if they had completed 8 weeks of training. The inclusion criteria for performing IMT were: clinical diagnosis of ALD; the presence of inspiratory muscle weakness (maximal inspiratory pressure<60cmH2O or lower than the predicted values for the Brazilian population)19; and no plans for engagement in physical activity programs or treatment therapies in the following 2 months. The patients who were in a PR maintenance program were included as long as the volume of PR remained constant toward the end of IMT.
Patients with neurological, metabolic, psychiatric or progressive neuromuscular diseases were excluded from the study. Patients with orthopedic problems that prevent them from performing activities of daily living and patients who could not understand or execute any procedure of the study were also excluded.19
Twelve patients fulfilled the inclusion criteria and were invited to participate in the study. Ten patients agreed to participate in the study and consented to follow-up in the interview and two refused to give interview.
InterventionIMT programThe IMT protocol consisted of home-based high-intensity daily training – two cycles of 30 breaths with a 1-min rest between sets, twice a day for 8 weeks using the POWERbreathe K3 (POWERbreathe K3, HaB International Ltd., UK).20 The intensity of the training was set to 50% of each patient's maximal inspiratory pressure measured every week20 and was adjusted weekly based on the Borg scale from 4 to 6 regarding respiratory effort performed during the session. If a patient scored more than 6 or less than 4 on the Borg scale after the session, the intensity of the training was adjusted to more or less than 50% of maximal inspiratory pressure respectively. The patients were instructed to perform deep and vigorous inspirations. One session per week was carried out under the supervision of the same physical therapist. Patients performed other sessions in their home without supervision.20,21
Data collection and managementThis study used semi-structured interviews with wide-ranging open questions that addressed the patients’ perception regarding IMT, their mobility, their activities of daily living, and their behavior after the intervention. The patients were asked how they felt after the 8-week training compared to how they were before being enrolled in the study. If the patients reported any changes or effects of the IMT, they were asked to elaborate on which aspects of the IMT or in which activities they noticed the changes. They were also asked how they felt after training with the device.
Scheduling the interviews was conducted by telephone, and the interviews were performed in the research laboratory by the same researcher at a time chosen by the patients. The interviews were recorded using digital equipment and were later transcribed by the same researcher who had performed the interview. Each interview was transcribed in its entireity including the questions of the researcher and answers of the patients to allow in-depth exploration of the material. The transcripts were submitted to the participants for their confirmation of the content.18
Data analysisThe data were evaluated using thematic analysis that involves the initial collection and reading of the text, investigative interpretations for resumption of research objectives and understanding of the data. The researchers performed an exploratory reading of the material multiple times, coding and creating the categories and different themes that emerged together with treatment and interpretation of the results.22,23
ResultsTen patients (eight women and two men, ranging in age between 27 and 82 years) were included in the study. The demographic data are presented in Table 1. Four patients were married, three were widows, two were singles and one was divorced. All patients lived in their own home, along with a family member: son(s), husband, or parents. All of the patients were unemployed because they had to cease working or never had a job due to their respiratory diseases. Five patients were diagnosed with COPD, two with bronchiectasis and three with pulmonary fibrosis. Eight patients were in maintenance pulmonary rehabilitation (i.e., those patients who completed 36 sessions of PR at least one month before the study enrollment) while two had not participated in any pulmonary rehabilitation. None of the patients were enrolled in a new or first PR program during the IMT study. All patients used oxygen during exercise or activity and from these, five were 24-h oxygen users. All patients presented with inspiratory muscle weakness (i.e., maximal inspiratory pressure=44 SD=13.9cmH2O) at the beginning of the training and completed at least 80% of all training sessions, which were recorded on the IMT device and in the patients’ files completed by the same responsible physical therapist who performed the weekly IMT sessions.
The socio-demographic and clinical characteristics of the study's 10 subjects.
| Id | Age | Medications | Gender | Marital status | Employment | Habitation | Clinical diagnostic | Oxygen therapy |
|---|---|---|---|---|---|---|---|---|
| A.F. | 82 | Anticoagulant Bronchodilator Antihypertensive Corticosteroid | Female | Widow | Retired | Living with grandkids | Idiopathic fibrosis | Exercise |
| E.L. | 66 | Bronchodilator Corticosteroid | Female | Widow | Retired | Living with daughter and son | COPD | Exercise |
| M.A. | 62 | Bronchodilator Corticosteroid | Female | Widow | Retired | Living with daughter | COPD | Exercise |
| M.S | 62 | Bronchodilator Corticosteroid | Female | Married | Retired | Living with husband | COPD | Exercise |
| R.R. | 52 | Bronchodilator Corticosteroid | Female | Married | Retired | Living with husband and daughter | COPD | 24h |
| L.O. | 32 | Bronchodilator Corticosteroid | Female | Married | No job | Living with husband and son | Idiopathic fibrosis | 24h |
| M.G. | 56 | Bronchodilator Corticosteroid Antihypertensive Antidepressive Calcium | Female | Divorced | Retired | Living with daughters | COPD | 24h |
| J.M. | 34 | Bronchodilator Corticosteroid | Male | Single | No job | Living with mom | Bronchiectasis | Exercise |
| S.C. | 39 | Bronchodilator Corticosteroid Antihypertensive Antibiotic | Female | Married | Retired | Living with husband and son | Bronchiectasis | 24h |
| R.P. | 27 | Bronchodilator Corticosteroid Antacid | Male | Single | No job | Living with parents and brother | Idiopathic fibrosis | 24h |
COPD, Chronic Obstructive Pulmonary Disease.
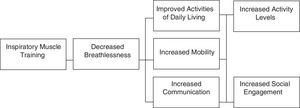
The patients’ perceptions regarding IMT are summarized in Fig. 1. The reports were grouped into four thematic categories: “impact of IMT on breathlessness”; “change in daily activities”; “improved mobility”; and “increased communication”.
Impact of IMT on breathlessnessTwo of the most distinct effects noted by the patients after completion of IMT program were the decreased sensation of breathlessness or dyspnea and increased breathing resistance while performing activities. The patients had this increased responsiveness throughout the intervention process. “I felt a sense of well-being […] Less fatigue.” (M. A, 62 years old) “I felt my lungs opening more […] it was easier to breathe […] my breaths became easier” (R. R., 52 years old) “[…] I am not feeling as tired as I previously felt.” (E. L., 66 years old)
The respondents, when they identified the decrease in the perception of breathlessness, reported an improvement in the performance of activities of daily living, such as bathing and dressing, as well as in instrumental daily living activities, such as washing the dishes, cleaning the house, and shopping. “[…] First I could not stand, I could not take a shower. But now I can […]” (E. L, 66 years old) “[…] I improved a lot […] I no longer need to turn on the oxygen, I sit on the bed after shower, dry and dress my clothes unworriedly.” (L. O., 32 years old) “I started washing dishes again which I haven’t been doing before. I started doing a lot of things around the house.” (R. R., 52 years old) “[…] when I needed to go to the supermarket, I felt less tired doing it.” (A. F., 82 years old)
Another aspect related to the decrease in the sensation of breathlessness reported by the respondents was the increase in locomotor capability. The respondents stated that they experienced increased strength and agility while walking since the IMT was able to improve the sense of decreased tiredness, which used to affect the performance of this activity. There was, in this case, better performance of that task from the perspective of the interviewees. “[…] I could not stand longer […] walk, for example […] Now I stand more, I have more capability.” (A. F., 82 years old) “[…] Previously, I walked like a turtle […] I still walk like a turtle, but now I’m not as tired as I was before.” (L. O., 32 years old)
The reports pointed to an improvement in speech resulting in greater communication and more social interaction. “More power, right? Even when speaking […] When I could, I felt my voice coming out better.” (M. G., 56 years old)
One interviewee noted that the training generated more power to talk, which resulted in the reduction of her loneliness. “[…] From the moment I started talking more, then it got better, right? […] I no longer isolate myself.” (M. G., 56 years old)
Another participant highlighted the decrease in fatigue during a conversation, which previously hindered her communication and often discouraged her from talking before the training. The IMT program enabled an increase in communication and social relationships. “Before, I even felt discouraged to speak. […] I talked and was more tired, more breathless, and people noticed that I didn’t speak very much. Not now, now I talk easily and more, right?” (L. O., 32 years old).
Only one of the interviewed patients explained that there was no difference after the 8-week IMT intervention: “I did not feel that I got better, that I was less tired or that I was breathing better after the training with the device because I already noticed that in this period of the year I always become very tired”. (M. S., 62 years old).
DiscussionThe main finding of this study was the improvement in daily activities, mobility and communication after the inspiratory muscle training on patients with ALD related to a perceived decrease in breathlessness. The use of interviews explained more about how patients changed their behavior after IMT and how breathlessness was correlated with their activities in life.24
It is known that dyspnea, or breathlessness, is the major symptom for patients with advanced lung disease and is closely related to the restriction of a number of activities.25 Dyspnea can be more important for some patients than for others, having a different impact in their lives. This seems to be a natural process since different patients consider their health condition differently; therefore, they would feel the improvements in dyspnea individually.15 This also would explain why some patients recognized the effects of IMT, whereas for others, the same training did not result in any perception of improvement, as cited by only one of the patients included in the present study.
The different perceptions of the interviewees after the IMT could be explained by the complex mechanism of dyspnea. Participants pointed to improvements in different instrumental and basic daily activities after IMT. It is worth considering that there are several factors involved in the mechanism of dyspnea and its management is complex.26 One of the main mechanisms of dyspnea in ALD is the ventilatory limitation that frequently leads to the interruption of the activity. Patients with ALD usually present with ventilation values close to the maximal ventilatory capacity during physical activities combined with a diminished ventilatory reserve. These two factors would limit daily activities once the highest inspiratory demand is produced in reaction to the increased respiratory effort, overloading the inspiratory muscles and compromising their ability to generate pressure.27,28 An increase in respiratory muscle strength and better muscle power obtained after the IMT could be related to a decrease in the ventilatory demand and the perception of inspiratory effort, and consequently, a decrease in breathlessness.29 Recently, it has been shown that there was a correlation between an increase in inspiratory muscle strength and improvements in functional exercise capacity that could result in increased levels of activity.30
The IMT is also associated with structural changes in inspiratory muscles in terms of the type of fibers and distribution.31 It is possible that IMT could improve inspiratory muscles work capacity reducing the overload presented in these muscles in patients with ALD, improving their ventilatory response during physical activity.30 Furthermore, trained inspiratory muscles seemed to consume a small fraction of the cardiac output leaving a major fraction available for other muscles, such as the muscles of the lower limbs, which could ensure a better performance while walking thus impacting mobility.32 As reported by some participants, the IMT improved their mobility, which could be attributed to decreased work imposed on respiratory muscles by reducing competition for the blood supply between respiratory muscles and the peripheral muscles.32 The physical activity limitation in patients with ALD is multifactorial, and insufficient energy resources available to the respiratory muscles is known to play an important role in this process.33 It is reasonable to cogitate that IMT can increase respiratory muscle efficiency, contributing to a decrease in the ventilatory limitation during activities of daily living.
The participants also reported improvement in communication following IMT. To the best of our knowledge, there are no results described in relation to IMT and speech or voice rehabilitation in patients with chronic lung dysfunctions. However, some studies have presented the effects of IMT on speech in patients with vocal dysfunctions. In a literature review, Sapienza34 suggested that patients with upper airway resistance caused by static or dynamic conditions, such as bilateral abductor vocal fold paralysis, subglottic stenosis, or paradoxical vocal cord dysfunction, should be IMT candidates. In these patients, IMT could modify the larynx activity and speech dynamic, thus being able to improve communication disorders.34 Baker et al.,35 in a single subject study design, evaluated the effects of IMT in a patient with bilateral paralysis of the abductors of the vocal folds. The results of this study showed that after 5 weeks of IMT, there was a 47% increase in respiratory muscle strength, which implied a reduction in dyspnea during speech and a decrease in the number and length of pauses while reading out loud.35
Several studies have shown the effects of IMT in patients with lung diseases12,29,30; however, none of them evaluated the effects of the training from the perspective of the patient. The effects of the IMT from the patient's view can be considered the strength of the present study. However, it is important to consider that different from a quantitative research, the aim in a qualitative research is to search for a description and understand how people feel and what is their sense of their world. In this sense, the researcher should not search for objectivity and should maintain distance from the participants to avoid giving them his or her expectations and prejudices.22 Although the researcher in this interview maintained a certain distance from the participants, at the moment of coding categories, inter-rater comparison with a co-researcher was not performed.
Considering the results of this study, it would be interesting to further explore the use of this research methodology in future studies, involving inspiratory muscle training in patients with chronic lung diseases. The perception of patients about the effects of an intervention opens new possibilities for improving clinical practice. Listening to the patients after a therapeutic intervention allows the therapists to critique methods of treatment and provides an opportunity to make adjustments in therapeutic care to expand the treatment results.36 Qualitative methods have been shown to provide additional information regarding the effects of PR, such as greater confidence, improved physical well-being, and the ability to perform certain activities, as opposed to regular questionnaires or exercise tests which provide quantitative data. The interviews used in this study were able to identify unique issues, following IMT, which were specific to each individual. These issues were identified by a lower sense of breathlessness that translated into less fear of exercise, improved mobility, or improved performance of activities of daily living.17 It is possible that patients became more confident in managing the disease, which may have improved their emotional ability to perform certain activities.
ConclusionThe conclusion of this study, therefore, showed that the perception of the majority of patients who had advanced lung disease was a reduced breathlessness with a positive impact on activities of daily living, mobility and communication after completion of a high-intensity inspiratory muscle training protocol for a period of 8 weeks.
Conflicts of interestThe authors declare no conflicts of interest.
This work was supported by Pró-Reitoria de Pesquisa da Universidade Federal de Minas Gerais, Conselho Nacional de Desenvolvimento Científico e Tecnológico – CNPq, Fundação de Amaparo à Pesquisa do Estado de Minas Gerais – FAPEMIG and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – CAPES.