The Michigan Neuropathy Screening Instrument is an easy-to-use questionnaire aimed at screening and detecting diabetic polyneuropathy.
ObjectiveTo translate and cross-culturally adapt the MNSI to Brazilian Portuguese and evaluate its measurement properties.
MethodsTwo bilingual translators translated from English into Brazilian Portuguese and made a synthetic version. The synthetic version was back translated into English. A committee of specialists and the translator checked the cultural adaptations and developed a pre-final questionnaire in Brazilian Portuguese (prefinal version). In pretesting, the prefinal version was applied to a sample of 34 subjects in which each subject was interviewed to determine whether they understood each item. For the later assessment of measurement properties, 84 subjects were assessed.
ResultsA final Brazilian Portuguese version of the instrument was produced after obtaining 80% agreement (SEM<0.01%) among diabetic patients and specialists. We obtained excellent intra-rater reliability (ICC3,1=0.90), inter-rater reliability (ICC2,1=0.90) and within-subject reliability ICC3,1=0.80, excellent internal consistency (Cronbach's alpha>0.92), reasonable construct validity for the association between the MNSI and Neuropathy Symptom Score (r=0.46, p<0.05) and excellent association between the MNSI and Neuropathy Disability Score (r=0.79, p<0.05). We did not detect floor and ceiling effects (<9.5% of patients with maximum scores).
ConclusionsThe Brazilian Portuguese version of the MNSI is suitable for application in the Brazilian diabetic population and is a reliable tool for the screening and detection of DPN. The MNSI can be used both in clinical practice and also for research purposes.
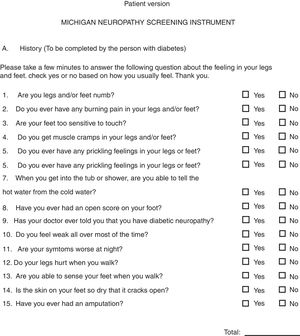
Diabetic polyneuropathy (DPN) is a common complication of diabetes mellitus. The progressive and irreversible course of the disease ultimately leads to an increase in ulceration and limb amputation rates.1,2 Different clinical scoring systems have been developed as quantitative instruments to diagnose the presence of DSN and classify its severity, including the Michigan Neuropathy Screening Instrument (MNSI)3–6; the Neuropathy Disability Score7,8 and Neuropathy Symptom Score6,7,9; the Diabetic Neuropathy Symptom Score; the Neuropathy Impairment Score10; and the Toronto Clinical Scoring System.11 These screening instruments, typically developed in English, assess the impact of these diseases on the quality of life of patients and are widely used in the literature. Specifically, the MNSI is an easy-to-use questionnaire effective at screening and identifying DPN because it addresses the major signs and symptoms that comprehensively map the disease, such as sensibility, reflexes, and orthopedic complications.3 In order to map DPN, the MNSI includes two assessments of signs and symptoms: a 15-item self-administered questionnaire and a set of physical assessments of the lower limbs. Impairment is determined by the number of positive responses or abnormal clinical findings. Compared to other instruments, MNSI is much more detailed about the reported symptoms of DPN and provides more information during the clinical assessment, which is crucial for the proper guidance of therapeutic actions.
Although the MNSI is one of the most widely used instruments in diabetes research worldwide,3–5,12–18 it is only available in English and in European Portuguese,4 and therefore, cannot be applied in Brazil. The existing studies using a translated MNSI4,15,16,18,19 worked with a simple translation, not a validated and adapted version, that was probably chosen based on its advantages over other instruments and its detailed characterization of the neuropathy. The translation, cross-cultural adaptation, and validation of instruments developed for use in a certain language and culture are important because this enables their effective application in other languages and cultural contexts, while maintaining the same measurement properties as the original version.20,21 The entire process is essential to ensure that the instrument is culturally accepted in the desired country and equivalent to the original.
There are currently two Portuguese versions of the MNSI: one was carried out by Barbosa et al.,4 who translated and validated the questionnaire for European Portuguese, and the other by Oliveira et al.,5 who translated and cross-culturally adapted it to Brazilian Portuguese without properly testing the all instrument measurement properties, as it is highly recommended in science. Besides, their back translation was not performed by two persons with the source language as their mother tongue, as it is recommended in Beaton.21 However, since the translation in the former study was carried out in Portugal, it exhibits semantic, idiomatic, cultural, and conceptual differences from Brazilian Portuguese and, therefore, cannot be used in Brazil.5 The second study5 failed to test the Brazilian Portuguese version of the questionnaire, making it impossible to determine whether the translation displays the same measurement properties as the original. In addition, in their cultural adaptation there is no mention to “agulhadas”, which is a very common and important symptom related to diabetic neuropathy and this is included in the English version, among some other differences to the present cross-cultural adaptation. Therefore, we proceeded with the cross-cultural adaptation and measurements properties of the MNSI in Brazilian Portuguese, applying the COSMIN20 recommendations, to ensure that all of the methodological procedures were carried out.
Therefore, the aim of the present study was to translate and cross-culturally adapt the MNSI to Brazilian Portuguese and to evaluate its measurement properties for use in research and clinical practice.
MethodsParticipants and designThe study was conducted at the Physical Therapy, Speech and Occupational Therapy department, School of Medicine, Universidade de Sao Paulo (USP), São Paulo, SP, Brazil. The study sample consisted of individuals diagnosed with type 1 or 2 diabetes, according to the criteria of the American Diabetes Association (ADA), treated at Associação Nacional de Assistência ao Diabético (ANAD) between May and December 2016. The number of participants evaluated were as follows: pretest phase – 19 patients and 15 professional healthcare specialists in diabetes care; and investigation of the measurement properties was assessed in 84 patients. Exclusion criteria were: people who did not fluently speak Brazilian-Portuguese, those suffering from blindness, cognitive disorders, liver disease, hypothyroidism, collagen diseases, vasculitis, and other causes of DPN (alcohol consumption, kidney failure). The study was approved by the Research Ethics Committee of the School of Medicine, USP.
The study was carried out in two stages: (1) translation and cross-cultural adaptation, and (2) testing of the measurement properties. The first stage followed the methods recommended by Beaton et al.’s21 guidelines and the second stage was in line with the recommendations of Terwee et al.22 All participants were advised of the procedures that would be performed and gave written, informed consent. Before the study began, we contacted the author of the original version6 of the MNSI (Dr. Eva Feldman) from the University of Michigan, who authorized the study procedures via email.
Michigan Neuropathy Screening Instrument (MNSI)The MNSI includes two assessments of signs and symptoms (Fig. 1): (1) a 15-item self-administered questionnaire and (2) a set of physical assessments of the lower limbs to be performed by a health professional in a clinical setting. The instrument contains 15 questions on sensation in the feet, the presence of DPN, and ulceration. Thirteen of the 15 questions can be scored one point each, so the maximal scoring for the questionnaire is 13. For the two remaining questions, if affirmative answers were given, they would score zero. The clinical assessment involves examining the feet and scoring each foot separately for the presence of alterations discovered upon clinical examination (deformities, dry skin, calluses, infection, or ulceration – 1 point each); a quantitative evaluation of vibration perception at the big toe (present – 1 point, decreased – 0.5 points, or absent – 0 points); and the classification of ankle reflexes (present – 1 point, reinforcement – 0.5 points, or absent – 0 points). In both sections of the MNSI, the higher the score, the greater the severity of DPN.6
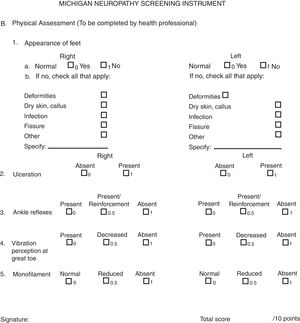
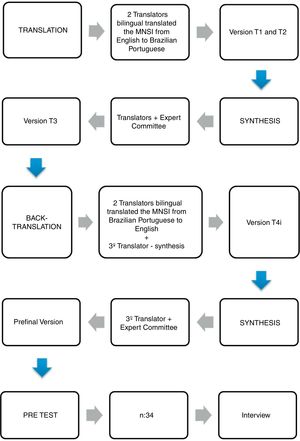
Translation and cross-cultural adaptationThe translation and cross-cultural adaptation of the MNSI was divided into 4 stages: translation, synthesis, back translation, and pretesting, as illustrated in Fig. 2 and described in detail below.
Two independent bilingual translators, whose native language was Brazilian Portuguese with English as their second language, translated the MNSI into Brazilian Portuguese, producing versions T1 and T2. The first translator was a physical therapist with knowledge in the field of health and the specific content addressed, and the second was an English language teacher with a degree in Bachelor of letters and no health-related knowledge, as recommended by Beaton et al.21
SynthesisThe two translators met with a specialist committee composed of four researchers, namely a physical therapist and a physical education professional, both bilingual and specializing in diabetes, and two additional bilingual physical therapists responsible for developing the project. The two translations were compared to the original version and discussed with the specialists. A consensual translation was produced along with a report identifying the difficulties encountered and the respective solutions. This report was shared with the original author, who approved the changes.
Back translationThe consensual was back translated from Portuguese into English by two independent native English-speaking translators from a translation company (http://traduciencia.com.br/news/), whose second language was Brazilian Portuguese and who had no knowledge of or access to the original questionnaire. The translator was neither familiar with the content addressed nor had any clinical knowledge. A third translator, whose native language is English with Brazilian Portuguese as a second language, compared the two back translations (BT1 and BT2) against the original version of the questionnaire, obtaining version T3. The committee of specialists and the third translator analyzed all of the translations to eliminate discrepancies and produced a prefinal questionnaire, as well as a report justifying their choices and decisions. This questionnaire should exhibit semantic, idiomatic, experiential/cultural, and conceptual equivalence to the original, and should be easily understood.21
PretestingThe pre-final questionnaire in Brazilian Portuguese was given to a sample of 34 subjects consisting of 15 professional healthcare specialists in diabetes and 19 patients with a medical diagnosis of diabetes. The patients were recruited from the National Association for the Assistance of People with Diabetes. After application of the pre-questionnaire, each subject was interviewed to determine whether they understood each item, according to Barbosa et al.’s4 guidelines for cognitive interviewing. To that end, the subjects and the professionals were asked to (1) state whether they understood (yes or no); (2) comment what they understood about each item read; and (3) suggest possible changes in the event of an item that was not understood. At least 80% of the patients and 80% of the specialists were required to understand the questionnaire for it to be considered acceptable.
After obtaining agreement for each item among the patients with diabetes and among the specialists, a final Brazilian-Portuguese version of the MNSI was produced. A report was submitted to the developer of the instrument describing the process carried out up to that point.
Measurement propertiesIn order to test the measurement properties, the final version of the MNSI was applied to a sample of 84 people medically diagnosed with type 1 or 2 diabetes, according to the checklist of consensus-based standards for the selection of health status measurement instruments (COSMIN).20 Diabetic participants were recruited from the Free National Campaign for the Prevention of Diabetes Complications, Detection, Guidance and Education, held in ANAD in 2016. Exclusion criteria were the same as those used in the pretesting stage.
Internal consistency, inter- and intra-rater reliability, floor and ceiling effects, agreement, and construct validity were assessed. To assess construct validity, we applied the Neuropathy Symptom Score (NSS),7 which evaluates typical DPN symptoms such as muscle weakness and sensory disturbances, and the Neuropathy Disability Score (NDS),23 a physical assessment of common signs of DPN, including reflexes, tactility, and vibration sensitivity. Our hypothesis was that the MNSI translated to Brazilian Portuguese would be as reliable as the other validated instruments to assess diabetic polyneuropathy in a clinical setting.
The analysis of measurement properties was based on the guidelines proposed by Weir24 and Terwee et al.22 For inter- and intra-rater reliability, the questionnaires were applied to the subjects on two separate occasions: the first evaluator applied all of the questionnaires (MNSI, NDS, and NSS) followed by the physical examination prescribed by the instrument and, after one hour, the same process was repeated by the second evaluator. After one week, the first evaluator applied all of the questionnaires again followed by a physical assessment of the same participants (n=84).
Statistical analysisSTATISTICA v.10.0 software was used for the statistical analyses. Reliability tests and correlation analyses were performed after confirming a normal distribution for NSS, NDS, and MNSI total scores. Pearson's correlation coefficients (>0.70) were calculated to measure the construct validity between (1) MNSI and NSS and (2) MNSI and NDS. The standard error of measurement (SEM) was used to assess agreement.
Following Weir's24 recommendations, intra-rater reliability was tested using the intraclass correlation coefficients (ICC3,1) for the measurements of the first evaluator at both evaluation occasions (one week apart). Inter-rater reliability was calculated with the ICC2,1 using the first data set from the two independent evaluators. Both intra-rater (ICC2,1) and inter-rater (ICC3,1) reliability were calculated only for the total score of the MNSI physical examination, which suffers the influence of the health professionals’ reliability. Within-subject reliability was tested using ICC3,1 for the total score of MNSI, since the questionnaire is self-reported. ICC values higher than 0.70 were adopted as the approval criteria for the reliability. Floor and ceiling effects were calculated considering that 15% of all interviewees obtained the lowest or highest possible score. Factor analysis was not performed due to the theoretical structure of the MNSI as one overall scale and the fact that the factorial structure was previously determined by the original authors. As such, Cronbach's alpha (>0.70) was calculated separately for each variable as well as overall for a final score that would determine internal consistency.22
ResultsTable 1 describes the sociodemographic data, type of diabetes, time since diagnosis, weight, height, information on DPN status (knowledge of the presence or absence of DPN), and fasting blood sugar levels of the patients studied at pretesting (n=34) as well as an assessment of the measurement properties (n=84).
Sociodemographic, anthropometric and clinical characteristics (mean (SD)) of patients evaluated in the pre-test phase and in the measurement properties phase.
| Pre-test phase Patients (n=19) | Measurement properties Phase (n=84) | |
|---|---|---|
| Males | 8 (42%) | 33 (44.6%) |
| Age (years) | 73.8 (7.3) | 63.8 (15.4) |
| Bodymass (kg) | 69.0 (15.1) | 70.3 (15.5) |
| Height (cm) | 161.4 (13.3) | 161.9 (12.4) |
| Type2 diabetes | 18 (99%) | 72 (97.2%) |
| Diagnosis of diabetes (years) | 17.2 (9.2) | 12.5 (9.3) |
| Fasting glicemia (mg/dL) | 120.7 (23.1) | 121.8 (40.3) |
In the initial translation, T1 and T2 showed many similarities; the few differences found were discussed among the translators and specialist committee, and the respective solutions were defined. Those differences and the choices of the translators are pointed out in the following discussion section. The best translation was selected based on the target population. All decisions were unanimous among the translators and committee of specialists. The chosen terminology was discussed and clarified and any discrepancies were eliminated, thus producing the pre-final version of the MNSI questionnaire.
In cognitive questioning, three changes were suggested to the 15 questions put to patients. Question 3 was only understood by 61.8% (7 patients did not understand), which was below the minimum required (80%) for interviewees according to Barbosa et al.’s4 recommendations. During the interviews with diabetic individuals, words or examples had to be added to the questions to make them easier to understand (questions 6 and 8). Questions 2, 8, and 14 were understood by 97.1% of patients (1 patient did not understand), and questions 11, 12, and 13 were understood by 91.2% (3 patients did not understand), with the remaining questions understood by all of the patients.
These questions were reformulated to produce a new version of the MNSI questionnaire, which was applied once again to the same 19 diabetic patients and 15 specialists to determine whether they agreed with the changes. All of the questions obtained an agreement percentage above 80% after the second round of questioning. Question 3 was understood by 86.6%; question 6, 100%; and question 8, 93.3%. Therefore, a final version of the MNSI was obtained, translated, and cross-culturally adapted to Brazilian Portuguese (Table 2).
Final translated version to Brazilian Portuguese of the Michigan Neuropathy Screening Instrument.
| A. História (A ser preenchida pela pessoa com diabetes). Por favor, dedique alguns minutos para responder às seguintes perguntas sobre a sensação em suas pernas e pés. Marque sim ou não com base em como você geralmente se sente. Obrigado | ||
|---|---|---|
| 1. Suas pernas e/ou pés ficam dormentes? | □ Sim | □ Não |
| 2. Você costuma ter dor em queimação nas suas pernas e/ou pés? | □ Sim | □ Não |
| 3. Seus pés são hipersensíveis ao toque a ponto de incomodar? | □ Sim | □ Não |
| 4. Você tem câimbras musculares em suas pernas e/ou pés? | □ Sim | □ Não |
| 5. Você costuma ter sensação de agulhadas ou formigamento nas suas pernas e/ou pés? | □ Sim | □ Não |
| 6. Dói ou incomoda quando a roupa de cama toca a pele das suas pernas ou pés? | □ Sim | □ Não |
| 7. Quando você entra no banho (chuveiro ou banheira), você consegue dizer se a água está quente ou fria nos pés ou pernas? | □ Sim | □ Não |
| 8. Você já teve ou tem uma ferida aberta (úlcera) no seu pé? | □ Sim | □ Não |
| 9. Um médico alguma vez disse que você tem neuropatia diabética? | □ Sim | □ Não |
| 10. Você sente fraqueza geral na maior parte do tempo? | □ Sim | □ Não |
| 11. Seus sintomas são piores à noite? | □ Sim | □ Não |
| 12. Suas pernas doem quando você anda? | □ Sim | □ Não |
| 13. Você consegue sentir seus pés quando anda? | □ Sim | □ Não |
| 14. A pele dos seus pés é tão seca a ponto de abrir rachaduras? | □ Sim | □ Não |
| 15. Você já sofreu alguma amputação? | □ Sim | □ Não |
| Total: _________ | ||
| B. Avaliação física (a ser preenchida pelo profissional da saúde) |
|---|
| 1. Aparência dos pés |
| a. Normal; 0 Sim, 1 Não |
| b. Se não, assinale as opções que se aplicam: |
| Deformidades |
| Pele seca, calos |
| Infecção |
| Fissura |
| Outros |
| Especifique: |
| 2. Ulceração; 0 Ausente, 1 Presente |
| 3. Reflexo aquileu; 0 Presente, 0,5 Presente/Com Reforço; 1 Ausente |
| 4. Percepção de vibração no hálux; 0 Presente, 0,5 Reduzida, 1 Ausente |
| 5. Monofilamento; 0 Normal, 0,5 Reduzido, 1 Ausente |
| Assinatura: |
| Pontuação Total: ______/10 Pontos |
The evaluation results for the questionnaire are as follows: intra-rater reliability was ICC3,1=0.90 (95% CI: 0.82–0.95) and the inter-rater reliability was ICC2,1=0.90 (95% CI: 0.85–0.94); within-subject reliability was ICC3,1=0.80 (95% CI: 0.69–0.91). Other results are: internal consistency (Cronbach's alpha>0.92), agreement (SEM<0.01%), and floor and ceiling effects (<9.5% of patients with maximum scores).
The construct validity was calculated using the MNSI-NSS association (r=0.46, p<0.05) and MNSI-NDS association (r=0.79, p<0.05), comparing (1) the total score of the MNSI questionnaire of symptoms with the total score NSS, since they are self-reported, and (2) the MNSI physical assessment total score with the NDS score, which should be assessed by a health professional.
DiscussionThe MNSI questionnaire is a valuable tool for healthcare professionals who need to screen or investigate possible clinical signs and symptoms of DPN. Although there are other instruments validated for Brazilian Portuguese,3 the MNSI has unique characteristics not found in other questionnaires, justifying the need for its use in that language. Specifically, the MNSI differs from other instruments in that it investigates the disease in greater detail, since it contains 15 questions, while others, such as the NDS, consist of only 6 items. Thus, its use in screening for the presence of DPN means that there is a greater chance of correctly characterizing the disease. Given that a DPN diagnosis has clinical implications, this aspect of the assessment is a decisive factor in securing an accurate diagnosis; as such, a questionnaire that covers a larger number of aspects in a more specific manner is desirable. Since this tool is widely used in the literature to investigate diabetes, including in Brazil, our aim was to translate and validate it for Brazilian Portuguese.
Differences were identified in the translation and cross-cultural adaptation phase, which were discussed among the translators and committee of specialists to establish solutions. For example, in question 5, the translation of the word “prickling” into Brazilian Portuguese required the use of two words, ‘agulhada’ (tingling) and ‘formigamento’ (numbness), both of which are symptoms of DPN. In question 7, the original item referred to the sensation of hot and cold water when getting into the tub or shower; for Brazilian Portuguese, we used ‘banho (chuveiro ou banheira)’, since the word banho refers to both showering and bathing in a tub. Question 9 was also adjusted, whereby the idea of a specific doctor (‘your doctor’) used in the original version was changed to ‘algum médico’ (any doctor), since it is common practice in the Brazilian National Health System (SUS) for patients to be treated and monitored by different physicians. We opted to use the word ‘andar’ (to walk) in questions 12 and 13, since ‘caminhada’ (a walk) in Brazil conveys the idea of physical exercise, while the former portrays the ability to move. In cognitive questioning, three changes were suggested to the 15 questions put to patients. These questions were reformulated to produce a new version of the MNSI, which was applied to the same subjects, obtaining the final version of the questionnaire that achieved over 80% understanding by both the patients and healthcare professionals.
Our results showed that the Brazilian Portuguese version of the MNSI obtained excellent inter- and intra-rater reliability, excellent internal consistency, good agreement, and no floor or ceiling effects, as well as an excellent degree of association between the MNSI and NDS and reasonable association between the MNSI and NSS. The last finding can be explained by the fact that the NSS contains only 6 questions, while the MNSI consists of 15, meaning the latter enables more detailed screening of DPN symptoms.
A limitation of the present study was the fact that this instrument was applied to a sample of patients from only one institution. Nevertheless, we believe that the sample shows significant variability in terms of the severity of diabetes mellitus, since the institution in question is a nationally recognized facility aimed at the target population. Although this study did not compare MNSI results against electroneuromyography findings, considered the gold standard for the diagnosis of neuropathies, a previously validated tool (NDS) based on the gold standard was used to test construct validity.23
In comparison to the original version of the MNSI instrument,6 our results were very good according to the Beaton et al.21 and COSMIN20 criteria. The original version of the MNSI does not present measurement properties, so the direct comparison between our version and the original could not be made. It is also interesting to note that the NDS and NSS, widely used surveys that were employed to calculate the construct validity, do not present any results for their measurement properties, including for the classification of ulceration risk. Therefore, we also could not compare our reliability results with theirs.
This new version of the Brazilian Portuguese MNSI can be used in a clinical setting as well as for research purposes, provides reliable results, and is more adapted to the Brazilian culture. As a screening tool for DPN, it can be applied in large-scale population assessments as well as for monitoring disease status.
ConclusionThe Brazilian Portuguese version of the MNSI is suitable for application in the Brazilian diabetic population and is a reliable tool for the screening and detection of DPN. It can be used both in clinical practice and for research purposes.
Conflicts of interestThe authors declare no conflicts of interest.
We are grateful to the National Council for Scientific and Technological Development (CNPq) for funding I.C.N. Sacco, C.D. Sartor and M. Dantas (Processes 305606/2014-0, 151531/2013-7, and 165062/2015-0, respectively). J.S.P. Ferreira received a Master's scholarship from the Coordination for the Improvement of Higher Education Personnel (CAPES). The authors also thank the ANAD (National Association for the Assistance of People with Diabetes) for kindly allowing us to acquire data at its facilities.