Low-back pain (LBP) may be directly or indirectly related to impairments from the hip joint.
ObjectiveTo evaluate the effectiveness of hip interventions on pain and disability in patients with LBP in the short-, medium-, and long-term.
MethodsPubMed, Cochrane Library, PEDro, Web of Science, and SCOPUS databases were searched in November 2022. Randomized controlled trials involving hip-targeted interventions compared to specific low back interventions in patients with LBP were selected. The outcomes were pain intensity and disability. The quality of the studies was assessed with the risk of bias tool. GRADE was used to rate the certainty of evidence. Meta-analyses were conducted using random effects models.
ResultsA total of 2581 studies were screened. Eight were included in the meta-analysis involving 508 patients with LBP. The results provided very low certainty that both hip strengthening and hip stretching improved pain (MD = -0.66; 95% CI -0.86, -0.48; I2:0%) (MD = -0.55; 95% CI -1.02, -0.08) and disability (SMD = -0.81; 95% CI -1.53, -0.10; I2: 80%) (SMD = -1.03; 95% CI -1.82, -0.25) in the short-term, respectively. No benefits were found in the medium- or long-term. The risk of bias, heterogeneity, and imprecision of the results downgraded the level of evidence.
ConclusionsVery low certainty evidence suggest a positive effect of hip strengthening in isolation or combined with specific low back exercise and hip stretching combined with specific low back exercise for decreasing pain intensity and disability in the short-term, in patients with LBP.
Systematic review registration numberPROSPERO CRD42022303173
Low Back Pain (LBP) is one of the major causes of pain and disability in adults and a common reason for seeking medical care.1,2 LBP is experienced by 80% of the population at least once during their lifetime.3,4 The prevalence of LBP is gradually increasing and is higher among females in all age groups.5 LBP can be classified based on symptoms duration in acute, sub-acute, or chronic LBP,6 or according to diagnosis, in which approximately 90% of patients with LBP are categorized as non-specific LBP, meaning that the etiology is not known.2
The lumbar spine is interconnected to the pelvis and hips, so LBP may be directly or indirectly related to impairments from adjacent structures. Some studies found that an excessive amount of anterior pelvic tilt is used to compensate a lack of hip extension, and that limited hip extension also alters the motor activation of the lumbar spine.7–10 In addition, several authors, concluded that patients with LBP often present hip pain and morning stiffness,11 a reduction of both passive and active hip rotation range of motion,12–17 and/or hip extensor muscle weakness.18
Exercise therapy is the most recommended intervention for LBP. But, there is no clear evidence on which type of exercise is more effective,19 and the effects are small to moderate. Based on the interconnection of the lumbopelvic structures with the hip, interventions targeting the hip or the addition of hip-targeted interventions to specific low back interventions may provide better benefits for patients with LBP. Two systematic reviews and meta-analysis addressed this topic and reported conflicting results about the effectiveness of adding hip interventions to specific low back treatments.20,21 Since the publication of these reviews, new randomized controlled trials (RCTs) have been published in this field.
Therefore, the aim of this systematic review with meta-analysis was to investigate the effectiveness of hip-targeted interventions, in isolation or in combination with LBP interventions, compared to specific low back interventions to improve pain and disability in patients with LBP.
MethodsStudy designThe protocol of this systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with the registration number CRD42022303173. This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement and Cochrane recommendations.22
Search strategyThe bibliographical search was conducted in PubMed (MEDLINE), Physiotherapy Evidence Database (PEDro), Scopus; Cochrane Library, and Web of Science (WOS) from inception to 20 November 2022. The Population, Intervention, Comparison, Outcome, and Study design (PICOS) framework was used to define the search strategy. Medical Subjects Headings (MeSH) were used as the keywords in the search strategy: back pain, low back pain, sciatica, low back ache, mechanical low back pain, hip, hip joint, pain measurement, disability evaluation, and clinical trial. The strategies used for each database are shown in Supplementary material – Table S.1. Scopus database was included as a tool for searching gray literature, and a hand search of the reference list of the included studies was performed. Searches were limited to studies in English, French, and Spanish.
Eligibility criteria and study selectionThe included studies met the PICOS criteria: 1) Population: adults diagnosed with LBP; 2) Intervention: hip-targeted conservative interventions applied in isolation or combined with specific low back interventions; 3) Comparison: specific low back interventions in isolation defined as the use of any physical intervention (manual therapy, massage therapy, exercise therapy, thermotherapy, electrotherapy, or other therapy) that targeted the low back specifically and not the hip joint; 4) Outcomes consisted of pain intensity and disability; 5) Study design: RCTs.
Studies were excluded if they: 1) were trials conducted with animals, cadavers, or simulators; 2) included participants with traumatic injuries or after surgical interventions; 3) the intervention was applied to the whole body; 4) the outcome variables reported were not the outcomes of interest or were not measured using a valid and reliable instrument.
After results of searches were retrieved, references were exported to Mendeley desktop, and duplicates were removed. Two reviewers independently (LC and SJ) assessed the title and abstract of each reference to determine potential eligibility. The same independent reviewers assessed potential full texts. A third author (EE) resolved the discrepancies between the two reviewers. Three authors of original papers were contacted by e-mail to clarify eligibility criteria. The inter-rater agreement was calculated using the Cohen's kappa coefficient.23
Data extractionThe two authors independently extracted the data from the identified studies using the standardized process adapted from the Cochrane Collaboration. Extracted information included: 1) characteristics of the study population; 2) aspects of the intervention performed; 3) outcome measures; 4) results; and 5) follow-up period. The third assessor resolved any disagreements. Data were analyzed using a qualitative synthesis and, whenever possible, using a quantitative synthesis (meta-analysis).
Risk of bias and certainty of the evidenceTwo assessors assessed the quality of the studies using the Cochrane Risk of Bias tool. The Cochrane Risk of Bias tool determines the potential bias and the internal validity of the studies and classifies them as “low”, “unclear”, or “high” risk based on 7 criteria.24 This tool has shown to be reliable for evaluating the quality of studies and assessing risk of bias. Funnel plot asymmetry to assess publication bias in the meta-analyses was not conducted in this study because the meta-analyses presented did not meet the rule of at least 10 trials.
The GRADEpro GDT was used to develop a summary of the findings. This classification categorizes the evidence as “high”, “moderate”, “low”, or “very low” and allows researchers and clinicians to discern the importance of the results. The certainty of evidence for the meta-analysis was downgraded according to the presence of the following: risk of bias (downgraded by one level or two levels if more than 25% or 50% of the participants were from studies with poor or fair methodological quality: lack of allocation concealment, random allocation and/or sample size calculation, participant, and personnel blinding, blinding of outcome assessors), inconsistency of results (downgraded by one level if there was significant heterogeneity regarding outcome measurement or intervention, or if the I2 value was ≥50%, and two levels if the I2 was ≥75%),25,26 indirectness of evidence (downgraded by one level if different populations, interventions, or comparators were included), and imprecision (downgraded by one level if fewer than 100 participants were included in the comparison, and two levels when the sample sizes were ≤30 individuals).26–28 Single randomized trials were considered inconsistent and imprecise and provided “low certainty” evidence. This could be further downgraded to “very low” certainty evidence if there was also a high risk of bias.24,29
Data synthesis and analysisThe quantitative synthesis of the results was conducted according to the outcomes considered: pain intensity and disability. When studies used different tools to assess the same outcome, the authors performed inverse variance methods.
Separate analyses were performed for pain intensity and disability. When studies reported pain data on a scale other than 0 to 10 (e.g., 0 to 100) we transformed the data into a 0 to 10 scale.30 Time points of assessment considered were short-term (or post intervention), medium-term (6 months), and long-term (12 months). Mean, standard deviation (SD), and sample size at each time point were extracted for each group. Outcomes were analyzed based on the post-intervention means and SDs by calculating the mean difference (MD) when studies used the same scale or standardized mean difference (SMD) when studies used different scales, with 95% CIs. Significance was set at a P value <0.05. The minimum clinically important change (MCID) on pain intensity was stated as 1.5.31 For disability, the between-group effects size was used to classify the effect estimates as small (SMD at least 0.2 but less than 0.5), medium (SMD from 0.5 to less than 0.8), or large (SMD 0.8 or greater).32
Data were combined for meta-analysis using a minimum of two trials assessed as clinically homogeneous. Trials were considered clinically homogeneous if there was a common intervention and outcome. When a three-arm study was included, the data from the control group were divided.33 Random-effect meta-analysis was performed when the combination of intervention effects could incorporate an assumption that the studies are not all estimating the same intervention effect.34
A researcher analysed data using RevMan 5.4 software.
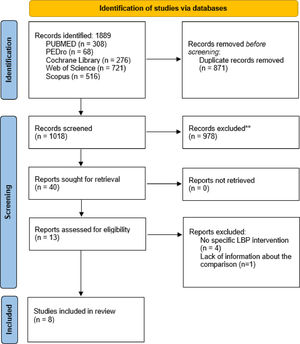
ResultsLiterature search and screeningEight studies were included in the qualitative and quantitative synthesis. One study was excluded due to lack of information about the comparison group.35 The description of the selection process is shown in the PRISMA flowchart diagram (Fig. 1). The agreement between reviewers was calculated by kappa with a value of 0.9.
Characteristics of included studiesA total of 8 RCTs were included comprising 508 patients with LBP. The sample size ranged from 24 to 80 patients.
Most studies included patients with LBP for at least 6 weeks,36 or 3 months.37–40 All the studies included patients with LBP older than 18.36–43 Concerning the LBP diagnosis, 3 studies included patients with non-specific LBP,36,38,39 one study included patients with mechanical LBP,41 and 3 studies did not specify the LBP diagnosis.40,42,43 The sociodemographic and clinical characteristics of the participants in each study are shown in Table 1.
Sociodemographic and clinical characteristics of the participants.
CG, control group; CLBP, chronic low back pain; CNSLBP, chronic non-specific low back pain; EG, experimental group; LBP, low back pain; MLBP, mechanical low back pain; NPRS, numeric pain rating score; NSLBP, non-specific low back pain; ODI, Oswestry Disability Index; RMQ, Roland Morris Questionnaire; SD, standard deviation; VAS, visual analogue scale.
The hip-targeted intervention group (hip-targeted intervention) in each trial consisted of different hip interventions. Seven studies added hip-targeted interventions to specific low back interventions,36–39,41–43 and only one applied hip treatment in isolation.40 Four studies combined hip strengthening with specific low back exercise,36–38,42 one applied hip abductor strengthening in isolation,40 one study combined hip joint stretching with specific low back exercise,38 and 3 studies applied hip joint mobilization and strengthening plus specific low back intervention.39,41,43
Specific low back intervention groups (control) were mainly based on lumbar stabilization exercises in all 8 studies.36–43Table 1 shows the treatments applied in the hip and low-back groups.
Information on the duration of the sessions, the number of sessions per week, and the total number of sessions are presented in the Supplementary material - Table S.2. The sessions duration ranged from 20 to 60 min,37–39,42,43 the most common frequency was 2–3 sessions per week,37–40,42,43 and most of the studies performed a total number of sessions between 18 and 24.37,38,40,42 Three studies did not reported the frequency, duration, and/or the total number of sessions.36,41,43
Outcome measuresThe outcomes considered in this meta-analysis were pain intensity and disability. Seven studies assessed pain intensity. Five studies used the visual analogue scale (VAS),36–40 and 2 used the numeric pain rating score (NPRS).41,43 Disability was measured for all the studies. Six studies used the Oswestry Disability Index (ODI),36–38,41–43 and 2 used the Roland Morris Questionnaire.39,40
All the studies assessed the outcome variables at baseline and after the intervention (short-term).36–43 Two studies assessed the medium- and long-term results at 6 months and at 12 months of follow-up, respectively.39,43
Study quality and risk of biasAll RCTs included in this review showed a high risk of selection bias and reporting. Most of the studies correctly performed the random sequence generation, but the concealment allocation was only performed in 3. No study blinded the participants or therapist (this item is expected in conservative non-pharmacological interventions). The Cochrane risk-of-bias tool results are shown in Fig. 2.
Synthesis of resultsPain intensityPain intensity was measured in 7 studies after the intervention,36–41,43 and in 2 studies at 6 and 12 months of follow-up.39,43
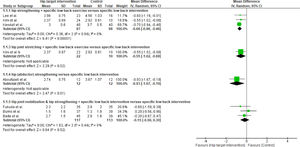
Hip strengthening + specific low back exercise versus specific low backVery low certainty evidence showed that hip strengthening plus specific low back exercise provide statistically significant but clinically unimportant improvement in pain intensity compared to specific low back intervention (MD = −0.66; 95% CI −0.86, −0.48; I2: 0%; 3 studies, 153 participants) (Fig. 3A).
Hip joint stretching + specific low back exercise versus specific low backVery low certainty evidence showed that hip joint stretching plus specific low back exercise provide statistically significant but clinically unimportant improvement in pain intensity compared to specific low back intervention (MD = −0.55; 95% CI −1.02, −0.08; 1 study, 32 participants) (Fig. 3A).
Hip abductor strengthening versus specific low back interventionVery low certainty evidence showed that hip abductor strengthening provide statistically significant but clinically unimportant improvement in pain intensity compared to specific low back intervention (MD = −0.93; 95% CI −1.67, −0.19; 1 study, 24 participants) (Fig. 3A).
Hip joint mobilization and hip strengthening + specific low back intervention versus specific low back interventionVery low certainty evidence showed that hip joint mobilization and hip strengthening plus specific low back intervention provide no better improvement in pain intensity compared to specific low back intervention (MD = −0.15; 95% CI −0.59, 0.30; I2: 0%; 3 studies, 230 participants) (Fig. 3A).
These studies measured pain intensity in the medium-term and long-term.39,43 Very low certainty evidence showed that hip joint mobilization and hip strengthening plus specific low back intervention provide no better improvement in pain intensity compared to specific low back intervention at medium-term (MD: −0.32; 95% CI: −0.96, 0.31; I2: 0%; 2 studies; 146 participants) (Fig. 3B), or long-term (MD: −0.10; 95% CI: −0.65, 0.45; I2: 0%; 2 studies; 146 participants) (Fig. 3C).
Disability was measured in all the studies after the intervention,36–43 and in 2 studies at 6 and 12 months of follow-up.39,43
Hip strengthening + specific low back exercise versus specific low backVery low certainty evidence showed that hip strengthening plus specific low back exercise provide a large improvement in disability compared to specific low back intervention (SMD = −0.81; 95% CI −1.53, −0.10; I2: 80%; 4 studies, 220 participants) (Fig. 3D).
Hip joint stretching + specific low back exercise versus specific low backVery low certainty evidence showed that hip joint stretching plus specific low back exercise provide a large improvement in disability compared to specific low back intervention (SMD = −1.03; 95% CI −1.82, −0.25; 1 study, 32 participants) (Fig. 3D).
Hip abductor strengthening versus specific low back interventionVery low certainty evidence showed that hip abductor strengthening provide no improvement in disability compared to specific low back intervention (SMD = −0.77; 95% CI −1.60, 0.07; 1 study, 24 participants) (Fig. 3D).
Hip joint mobilization and hip strengthening + specific low back intervention versus specific low back interventionVery low certainty evidence showed that hip joint mobilization and hip strengthening plus specific low back intervention provide no improvement in disability compared to specific low back intervention (SMD = 0.06; 95% CI −0.30, 0.42; I2: 46%; 3 studies, 230 participants) (Fig. 3D).
These studies measured disability in the medium-term and long-term.39,43 Very low certainty evidence showed that hip joint mobilization and hip strengthening plus specific low back intervention provide no improvement in disability compared to specific low back intervention in the medium term (SMD = −0.01; 95% CI; −0.33, 0.31; I2: 0%; 2 studies; 146 participants) (Fig. 3E), or long-term (SMD = 0.05; 95% CI; −0.27, 0.38; I2: 0%; 2 studies; 146 participants) (Fig. 3F).
According to GRADE, the overall certainty of evidence for all comparisons were rated as very low for pain intensity and disability (Table 2).
Summary of evidence of the results according to their certainty and their importance using the GRADE tool.
CI, confidence interval; MD, mean difference; RCTs, randomized controlled trial; SMD, standardized mean difference.
Explanations:.
a. More than 25% of the participants were from studies with poor or fair methodological quality, considering these aspects: Lack of allocation concealment, random allocation and/or sample size calculation, participant and personnel blinding, blinding of outcome assessors.
b. Significant heterogeneity regarding outcome measurement or intervention, or if the I2 value was ≥50%.
c. Significant heterogeneity regarding outcome measurement or intervention, or if the I2 value was ≥75%.
d. Fewer than 100 participants were included in the comparison or single randomized controlled trials included.
High: We are very confident that the true effect is close to the estimate of the effect.
Moderate: We are moderately confidence in the effect estimate. The true effect is close to the estimate of the effect, but the result can be different.
Low: Confidence in the effect estimate is limited, the true effect can be substantially different from the estimate of the effect.
Very Low: There is little confidence in the effect estimate, the true effect is likely to be substantially different from the estimate effect.
The present systematic review and meta-analysis found very low certainty evidence suggesting that hip strengthening in isolation or combined with specific low back exercise and hip stretching combined with specific low back exercise are more effective for reducing pain intensity and disability than specific low back interventions in isolation in patients with LBP in the short-term. The risk of bias, inconsistency, and imprecision of the results downgraded the level of evidence to very low (GRADE).
Concerning the methodological quality of the included RCTs, common methodological flaws were lack of concealed allocation, blinding of participants, therapists, and assessors, and sample size calculation. But it is important to consider that therapist blinding is not possible in conservative non-pharmacological interventions.
This meta-analysis included 8 RCTs and indicated that the application of hip strengthening in isolation or combined with specific low back exercise and hip stretching combined with specific low back exercise in patients with LBP showed an immediate decrease in pain intensity and disability. The changes achieved were statistically significant but clinically unimportant for pain intensity (MD= −0.55; −0.93), and the effect estimated for disability was moderate to large (SMD= −0.77; −1.03). Our results were similar to those obtained by De Jesus et al., but the MDs and SMDs achieved in this study were higher for pain intensity and disability.21 These differences could be because, in the study of De Jesus et al., only 4 and 5 studies measured pain intensity and disability, respectively.21 In addition, the interventions were based on hip flexor, extensor, abductor, and adductor muscles strengthening in all the studies included, so the experimental groups were more homogeneous, but the comparison did not only include specific low-back interventions. In contrast, Bernet et al.,20 concluded that adding hip-targeted interventions in patients with LBP produced no benefits.20 However, this meta-analysis included only 5 studies in which the interventions were based on hip strengthening, manual therapy, strengthening plus manual therapy, and aquatic therapy.20 Therefore, each included study performed a different intervention showing a high heterogeneity, which could affect the results.
This is the first systematic review and meta-analysis investigating the medium- and long-term effects of hip interventions in patients with LBP. Only 2 studies assessed the medium- and long-term effects, and the changes were not statistically significant. The results showed that the treatment of the hip seems to produce no benefits in the medium- or long-term follow-up. These results must be interpreted with caution due to the small number of studies that assessed the follow-up. Also, the guidelines followed by these patients during the follow-up period was not described, nor the forms of control by the study authors.
The short-, medium-, and long-term results found in this systematic review and meta-analysis may be related to several factors, such as the eligibility criteria, the type of intervention, and the intervention duration.
The eligibility criteria for all the included studies36–43 and for recent meta-analysis20,21 was the application of a hip-targeted intervention in patients with LBP. But only 2 studies described the presence of a hip impairment, such as hip range of motion limitation or hip muscle strength weakness39,43 as inclusion criteria. The application of a specific intervention in the hip joint or related tissues when there is no hip impairment could be related to the lack of improvements in pain intensity or disability.36,37,41
Seven of the included studies applied lumbar stabilization exercises or guideline-oriented low back treatment in the hip-targeted group.36–39,41–43 These therapies have shown to be effective in reducing pain and disability in patients with LBP.44 However, the interventions applied to the hip region varied widely. Five studies applied hip strengthening,36–38,40,42 3 studies combined hip strengthening with manual therapy,39,41,43 and one study applied hip stretching.38 The heterogeneity of the interventions used in the hip-targeted group of each study and the application of a specific treatment in the hip region in patients with LBP but without any coexisting hip impairment may explain the lower values found in the short-term and the lack of benefits in the medium- and long-terms. Future studies should consider the assessment of the hip region in patients with LBP and verify the most appropriate type of therapy for each situation.
Concerning the duration, the frequency, and the total number of sessions, most of the included studies applied 10 to 24 sessions in a period of 4 to 8 weeks.37–40,42 However, 3 studies did not present all the necessary information to replicate the study.36,41,43 These studies did not describe the duration of the intervention and the total number of sessions, and 2 presented no statistically significant differences between groups.36,43 The results achieved in this study in the short-, medium- and long-term may also be related to the frequency or the duration of the intervention.
From a clinical point of view, this study found very low certainty evidence suggesting that hip strengthening in isolation or combined with specific low back exercise and hip stretching combined with specific low back exercise is effective for reducing pain intensity and disability in patients with LBP in the short-term. In addition, very low certainty evidence suggested that hip joint mobilization and hip strengthening combined with specific low back intervention versus specific low back intervention produce no improvements in the short-, medium-, and long-terms. These results should be considered according to its strengths and limitations. The main strengths are the comprehensive literature search, methodological consistency, data extraction, rigorous statistical analysis, and the inclusion of RCTs. Some important limitations were the different types of treatments applied, the inadequate description of the therapies, the heterogeneous durations of the interventions, and the lack of hip impairments as an eligibility criterion. Additionally, the small number of studies included in the medium- and long-term follow-up analysis should be considered.
This systematic review and meta-analysis has some limitations. Our search strategy may have been limited by the omission of other databases, such as SportDiscus, and we may have missed relevant articles. The heterogeneity found in the treatments applied in the studies, such as the type and duration of the therapies, complicates the interpretation of our results. Methodological limitations include the insufficient sample size that could overestimate the results and the lack of follow-up measurements of the studies. Future studies should consider hip impairment as an eligibility criterion, such as hip range of motion limitation or hip muscle weakness, to analyze the effects of hip-targeted intervention in patients with LBP. Thus, the management of a patient with LBP should include a hip-targeted intervention only when a hip impairment is detected during the assessment. The quality of the studies should be improved. Future studies should consider the allocation concealment and blinding of participants and researchers to reduce the risk of bias. The total number of sessions and the duration of the intervention should be described to allow the replication and comparison of the study. Finally, the combination of therapies that produces the best effects should be investigated, as well as their dose.
ConclusionThis systematic review and meta-analysis found very low certainty evidence suggesting a positive effect of hip strengthening in isolation or combined with specific low back exercise and hip stretching combined with specific low back exercise for decreasing pain intensity and disability compared to specific low back interventions in isolation, in the short-term, in patients with LBP. Further investigation is needed to determine the medium- and long-term effects of hip-targeted interventions in patients with LBP and to determine the best multimodal intervention.