Understanding the care pathway is essential to identify how to effectively treat spinal disorders. However, there is no specific data on the pathway of these individuals in the Health Care Networks (HCN) in Brazil.
ObjectiveTo investigate the pathway of individuals with non-specific spinal disorders (NSD) in the HCN in the Federal District, Brazil, and verify the interventions adopted, and to test whether sociodemographic and clinical variables predict the number of imaging tests, prescribed medication, and the first HCN access.
MethodsRetrospective study that analysed electronic records of 327 individuals with NSD between 2012 and 2018. Generalized linear models estimated the association between sociodemographic and clinical data and number of drugs prescribed and imaging tests requested. Multinomial logistic regression estimated the association between clinical and demographic variables and setting of first access.
ResultsThe median age was 57 years, and 75.5% were women. Emergency Department (ED) was the most accessed setting (43.7%), and back pain was the most prevalent condition (84.5%). Most individuals underwent imaging tests (60%) and drug prescriptions (86%). Physical exercises were prescribed to 13%, and 55% were referred to physical therapy. Women were more likely to first access the ED.
ConclusionThe ED was the most used setting by people with NSD. Few participants received exercise prescriptions and half were referred to physical therapists. Individuals who used outpatient clinics and primary care received less drug prescriptions, and women were more likely to first access the ED. Increasing age was associated with greater chance of first accessing Outpatient Clinics.
In Brazil, the public health system (SUS) provides universal and free health at all levels of care.1 The demographic and epidemiological transition in Brazil has resulted in greater longevity for the population.1 Consequently, there is an increasing prevalence of non-communicable chronic diseases such as spinal disorders, which have a considerable impact on healthcare demands.1,2 These demands resulted in new policies, particularly the implementation of Health Care Networks in 2010, aiming to provide more integrated healthcare assistance between the primary, secondary, and tertiary levels.3
Non-specific spinal disorders (i.e., an umbrella term to refer to a variety of spinal disorders, including back pain, neck pain, thoracic pain, scoliosis, sacroiliac joint pain) are considered a major public health problem and are one of the main chronic diseases resulting in years lived with disability worldwide.4 For instance, neck pain and low back pain accounted for approximately 22 and 63 million years lived with disability in 2019, respectively,5 and is one of the main causes of disability worldwide.4,5 Moreover, spinal disorders represent an economic burden for healthcare systems, as they are a frequent reason for using health services, including in Brazil.4,6-14
A previous study has shown considerable costs arising from the management of spinal disorders in Brazil.13 The study found more than 250,000 inpatient days related to approximately 36,000 hospital admissions due to spinal disorders in Brazil, in 2016, mainly dorsalgia and intervertebral disk disorders. Moreover, 18% of the total expenses were related to diagnostic imaging, and physical therapy interventions were widely adopted in outpatient units.13 Currently, there are recommendations for individuals with non-serious spinal disorders to be followed up in the primary healthcare.7,15 Such recommendations aim to reduce the costs of low value interventions (low evidence, e.g., routine use of imaging tests and medication),7,8,16-20 including frequent access by individuals with non-specific spinal disorders to emergency services.10-12 This is relevant because a recent study21 showed that the vast majority of management strategies in individuals with non-specific back pain in Emergency Departments of four public hospitals in Brazil were drug prescriptions, which are considered of low value to this condition.7,20
Due to the high disability and socioeconomic impact of spinal disorders, health professionals, managers and society should be concerned about the implementation of more effective strategies to manage these conditions.6,9,13,15,16 However, in Brazil, little attention has been given to spinal problems by health systems11,16,17 despite estimates of an increase in their prevalence in the upcoming years.2,8
Therefore, the understanding of the care pathway is essential to identify aspects for improvement and, consequently, how to effectively treat conditions affecting the spine.11,16 However, there are no specific data related to the care pathway of individuals with these conditions in the Public Health Care Networks in Brazil. Accordingly, we aimed to investigate and characterize the pathway for individuals with non-specific spinal disorders accessing the Health Care Network of the Distrito Federal, Brazil. The secondary aims were to verify the number of procedures and interventions adopted in the networks; and investigate if sociodemographic and clinical variables might predict the total number of imaging tests, the total number of prescribed medications, and the place of first access in the Health Care Network.
MethodStudy designRetrospective study with secondary data obtained from the electronic medical records of individuals with non-specific spinal disorders. This study was reported following STROBE22 recommendations, and was approved by the Ethics Committee (Campus Universidade de Brasília-UnB Ceilândia Ethics Committee, CAAE protocol n. 26011419.7.0000.8093).
ParticipantsWe considered data from individuals treated at the outpatient clinic of a large public hospital in the Federal District, Brazil. Adults of both sexes with non-specific spinal disorders were included. Participants were excluded if they entered the Network due to a specific spinal condition with a well-defined cause, such as trauma, inflammation, infection, or tumor. Participants were recruited by selection from electronic records of patients registered with a non-specific spinal disorder in 2018. Patients who met the eligibility criteria were included, and their medical records were analysed; retrospective follow-up covered the years 2012–2018. The information whether these patients were registered in 2012 was checked, to ensure the 7-years of follow-up.
SettingThe participating hospital is a reference hospital for two different administrative regions, including a total population of approximately 600,000 people.23 The hospital has emergency care and has 275 inpatient beds for several specialties, in addition to a specialized outpatient service. Data were used from the period between January 1st, 2012 and December 31st, 2018. The year 2012 was set as the start due to the greater stability and consolidation of the electronic medical record used in the Health Units from this date onwards. The year 2018 was set as the final year due to the implementation of a new electronic recording system for clinical and production data in Primary Care in 2019.24
Context for the studyThe Health Care Networks include services at the three levels of care, such as Family Health Support Centres (Primary Care), specialized outpatient clinics and surgical units. The purpose is to provide universal and free care for the population, including health promotion, prevention, and rehabilitation.3 Primary Health Care is the point of entry and coordinator of the pathway,1-3,25 and is responsible for a wide range of activities, such as multidisciplinary teams, and is responsible for the referral to other levels (i.e., secondary and tertiary).3 The emergency services assist individuals who need urgent care, and diagnostic support, which are responsible for providing services shared at all levels.1,3
In 2003, the SES/DF Program for Technological Upgrade of Health Care Units proposed the electronic registration of SUS users in the Federal District.26 The implementation of the electronic medical record system (TrakCare) began in 2004, and was the only electronic record shared among the Health Care Networks in the Federal District until 2018. TrakCare is a system that stores the personal and clinical information of users receiving care at the Health Care Networks and it communicates with other government systems (e.g., DATASUS), facilitating interdepartmental communication and management by providing information such as statistics and billing. Patients are identified by a single record (SES-number) generated in the first access to the health network and referenced throughout their progress.
Data extractionDue to technical difficulties in locating patients using the SUS electronic record system, the recruitment was carried out using the appointment records available at the investigated hospital. After selecting the eligible participants, we extracted information from the electronic medical records of patients that were diagnosed with an ICD code from the International Classification of Diseases (ICD-10) related to spinal disorders that were considered non-specific (multifactorial etiology).9
For the purpose of data analysis, the ICD-10 codes recorded as the primary diagnosis were grouped to characterize the following health conditions: 1) neck pain: M50 (cervical disk disorders) and M53 (other dorsopathies); 2) low back pain: M40 (kyphosis and lordosis), M51 (other intervertebral disk disorders), M54 (back pain); 3) scoliosis: M41 (scoliosis) and 4) other spinal conditions: M42 (spinal osteochondrosis), M43 (other deforming dorsopathies), M46 (other inflammatory spondylopathies), M47 (spondylosis), M48 (other spondylopathies), M49 (spondylopathies in diseases classified elsewhere), M99 (biomechanical injuries, not classified elsewhere) (Supplementary Material S1).
Variables and data sourcesThe following sociodemographic variables were extracted to characterize participants: sex (female or male), age (years), marital status (married, single, divorced, or widowed), occupation (according to the 2002 Brazilian Occupational Classification), place of residence (Federal District or surrounding areas) and level of education (primary, secondary, or tertiary). Variables related to lifestyle, such as smoking (current smoker, former smoker, and non-smoker) and activity level (sedentary or active) were also collected, as well as the presence of comorbidities that can influence the prognosis of spinal disorders such as depression, fibromyalgia, and obesity. The variables related to lifestyle were extracted according to the patient's answers to the health professional and inserted in the medical record. Comorbidities were collected according to the proven diagnosis and registered in the system by a qualified professional.
To map the pathways of patients in the Health Care Networks, we considered visits to these four settings: Primary Health Care, Specialized Care (Outpatient units), Emergency Department, and Hospital Admission. The number of visits to the Health Care Networks due to non-specific spinal disorders for each individual and the instance in which they started their follow-up in the SUS (first appointment) were extracted from the electronic medical record considering the period of the study.
To collect the number of resources and procedures accessed during the care pathway, the following information was extracted for each individual: 1) number of drug prescriptions; 2) number of imaging tests requested; 3) number of resources prescribed or intervention strategies implemented, such as referral to physical therapy; and 4) other interventions recorded in the system.
Data analysisData normality assumptions were evaluated using the Shapiro-Wilk test, which confirmed the non-parametric distribution of the sample's characterization data. Thus, data were analysed descriptively by median and quartiles (25%; 75%), absolute and relative frequencies.
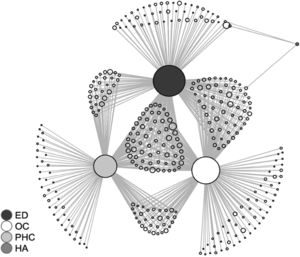
A graphic representation of the pathways of individuals in the Health Care Network was generated using an indirect network graph in the R-statistical program (version 4.1.1) and the “igraph” package.27 The incidence of the non-oriented matrix was generated by mapping all participants to the health settings visited (Primary Health Care, Specialized Care, Emergency Department and Hospital Admission), in a chronological order of visits between 2012 and 2018, which were represented by the central circles. The stems indicate the use of the settings, and each individual was represented by circles at the tip of the stems. The variables ‘number of resources’ and ‘intervention strategies’ were presented descriptively to characterize the pathway of participants in the Health Care Network.
Generalized linear models were used to estimate the association between response variables and their predictors. Variables with a low number of occurrences were not considered in the models. The first model considered the total number of requested imaging tests as the response variable, and the second model adopted the total number of prescribed drugs as the response variable. The predictors adopted in both models were age, sex, first access to the Network, presence of comorbidities, and use of physical therapy interventions. These predictors were chosen based on available data from the electronic medical records. The Poisson distribution was the most suitable for the first model, while the binomial was the most suitable for the second model. This choice was based on the Akaike information criterion (AIC) and the Bayesian information criterion (BIC), for which lower values indicated a more adequate fit of the data.
The third regression model adopted was a multinomial logistic regression, with the objective of estimating the association among the predictive variables age, sex, and presence of comorbidities, and the first access point in the Health Care Network. In the process of data analysis, Nagelkerke's pseudo R2 was calculated.
The statistical significance adopted in all analyses was 5% (p<0.05), with a confidence interval of 95%.
ResultsThe records of 398 individuals were evaluated for eligibility. Fifty-eight (58) records were excluded because the access to the network was not related to spinal disorders. Another 13 individuals were excluded (i.e., well-defined spinal condition). After applying the inclusion and exclusion criteria, 327 patients were included in the cohort of seven years (from 2012 to 2018). The participant selection flowchart is presented in Supplementary Material - S2.
Table 1 presents the data on participant characteristics. The median age was 57 years. The majority were female, married, sedentary, and with comorbidities. Most participants were service workers and retail salespeople. Most participants did not have recorded data related to level of education and smoking. The listed comorbidities included high blood pressure (50.8%), depression (19.3%), diabetes mellitus (19%), fibromyalgia (16.5%), and obesity (15.9%).
Characteristics of participants with non-specific spinal disorders, 2012–2018, Federal District.
Data are absolute frequency (proportion) and median (interquartile range: 25th percentile; 75th percentile).
In total, we found 1390 visits to the Heath Care Network for non-specific spinal disorders. The condition responsible for the highest number of visits was low back pain (84.5%), followed by neck pain (12.2%), and scoliosis (1.7%). The other spinal conditions (e.g., spondylosis) totalled 1.5%.
Details pertaining to the number of visits by healthcare setting are presented in Fig. 1 and Supplementary Material - S3. The Emergency Department was the most accessed setting (43.2% of the visits). Approximately 33.4% of the visits were in the Outpatient Clinic, 23% in the Primary Health Care, and 0.4% were Hospital Admissions. These findings illustrated in Fig. 1 demonstrate the higher frequency of access at the Emergency Department.
Graphic representation of the pathways of patients in the Health Care Network, for non-specific spinal disorders, between 2012 and 2018. The central circles represent the settings of the health system investigated (ED: Emergency Department; PHC: Primary Health Care; OC: Outpatient Care; and HA: Hospital Admission) and the larger their size, the greater the frequency of access by users in this instance. In the edges, each circle represents an individual. The stems represent the usage of the service in the settings for each individual. The more frequently the user visits the Health Care Networks, the larger the size of the circle. In cases where the stems are connected in more than one setting, the position of the individuals' circles is closer to the central circles (OC, PHC, HA, or ED), greater access is inferred in this setting.
More than 60% of the participants received a prescription for at least one imaging test. X-ray was the most prescribed (48%), followed by Magnetic Resonance Imaging (22.6%) and Computerized Tomography (4.3%). Details on diagnostic imaging use are presented in Supplementary Material - S4.
Eighty-six percent of the individuals were prescribed medication, with analgesics and anti-inflammatory drugs being the most often used (69% and 64%, respectively). Those drugs were mostly prescribed for low back pain, neck pain, and spondylosis (Supplementary Material - S5).
Furthermore, physical exercise was prescribed to approximately 13% of the individuals and 55% were referred to physical therapists. The majority of exercise prescriptions were performed in the Outpatient and Primary Care (i.e., 2.9% and 0.9% of the total number of visits, respectively). Exercise prescriptions rarely occurred in the Emergency Department (0.3% of the total number of visits). Prior to 2013, there were no occurrences of exercise prescription, which was more frequently adopted starting in 2016.
The number of imaging tests prescribed was not associated with the variables included in the regression model. In contrast, the number of medications prescribed to individuals with first access to the Primary Care or Outpatient Clinic was significantly lower compared to those with first access via Emergency Departments (Tables 2 and 3).
Factors associated with the number of imaging tests reported in electronic medical records of patients with non-specific spinal disorders, 2012–2018, Federal District.
| Total exam prescription | B (SE) | 95 % CI | p-value |
|---|---|---|---|
| Intercept | − 0.176 (0.252) | − 0.67, 0.31 | – |
| Age | 0.001 (0.004) | − 0.01, 0.01 | 0.835 |
| Sex | |||
| Female | 0.010 (0.136) | − 0.26, 0.28 | 0.940 |
| Male† | – | – | – |
| 1st access: | |||
| PHC | 0.065 (0.133) | − 0.19, 0.32 | 0.626 |
| OPC | − 0.228 (0.148) | − 0.52, 0.06 | 0.125 |
| ED† | – | – | – |
| Received physical therapy intervention | 0.176 (0.121) | − 0.08, 0.43 | 0.175 |
| Did not receive physical therapy intervention † | – | – | – |
| Comorbidities | − 0.005 (0.139) | − 0.28, 0.27 | 0.972 |
Generalized linear model with Poisson distribution. B, coefficient; SE, standard error; CI, confidence interval.
Factors associated with the number of imaging tests reported in electronic medical records of patients with non-specific spinal disorders, 2012–2018, Federal District.
| Total drug prescription | B (SE) | 95 % CI | p-value |
|---|---|---|---|
| Intercept | 1.283 (0.301) | 0.69, 1.88 | |
| Age | < 0.001 (0.005) | − 0.01, 0.01 | 0.985 |
| Sex: | |||
| Female | 0.115 (0.158) | − 0.19, 0.42 | 0.468 |
| Male† | |||
| 1st access: | |||
| PHC | − 0.535 (0.156) | − 0.84, 0.23 | 0.001 |
| OPC | − 0.630 (0.164) | − 0.95, −0.30 | < 0.001 |
| ED† | |||
| Received physical therapy intervention | 0.103 (0.140) | − 0.17, 0.38 | 0.461 |
| Did not receive physical therapy intervention † | – | – | – |
| Comorbidities | 0.096 (0.156) | − 0.20, 0.40 | 0.537 |
Generalized linear model with binomial distribution. B, coefficient; SE, standard error; CI, confidence interval.
Logistic regression analysis showed that females had a greater chance of first accessing the Emergency Department compared to Primary Care. The model also showed that for each extra year in age, there was an increase in the chance of a greater use of Outpatient compared with Primary Care (Table 4).
Factors associated with the setting of the first access recorded in the electronic medical record of patients with non-specific spinal disorders, 2012–2018, Federal District.
| 1st access: | OR | 95 % CI | p-value |
|---|---|---|---|
| ED | |||
| Age | 1.00 | 0.98; 1.02 | 0.740 |
| Sex: | |||
| Female | 1.994 | 1.07, 3.72 | 0.030 |
| Male† | |||
| Comorbidities | 0.572 | 0.31, 1.07 | 0.082 |
| OPC | |||
| Age | 1.039 | 1.02, 1.06 | 0.001 |
| Sex: | |||
| Female | 1.462 | 0.73, 2.93 | 0.284 |
| Male† | |||
| Comorbidities | 1.477 | 0.68, 3.22 | 0.327 |
| PHC† | – | – | – |
| Observations | 327 | ||
| Pseudo R2 (Negelkerke) | 0.12 |
Multinomial logistic regression. OR, odds ratio; CI, confidence interval.
We observed that non-specific low back pain was the most prevalent condition and the Emergency Department was the most accessed setting. We found that most patients underwent imaging tests and were prescribed drugs. In contrast, exercises were prescribed for only a small portion of individuals and referrals to physical therapy were recorded for approximately half of the participants. Women were more likely to first access the Emergency Department, and when this setting was the choice for the first access, more drugs were prescribed. There was an association between increasing age and greater chance of first access via Outpatient Care.
We found that the Emergency Department was the most accessed setting by individuals with non-specific spinal disorders. Currently, it is recommended that individuals with this condition, especially low back pain, be treated and monitored within Primary Care,7,8,17-19 because only a small minority of cases present red flags or indications of severe spinal involvement.10,17,19,20,28-30 Furthermore, the care of individuals with low-severity spinal disorders in the Emergency Department was associated with frequent use of resources and interventions considered of low value (i.e., low or no evidence), such as routine imaging tests, which do not provide additional clinical benefits30 and increase costs to the health system.12,13,28 These findings are worrying and are supported by previous studies reporting increased use of emergency services by patients with non-serious spinal disorders.11,28
Although there is an effort, through the Family Health Strategy, to strengthen Primary Care as the first level of care for the management of non-specific chronic pain,25 there are some organizational inconsistencies in the health care process, such as the scarcity of human resources and the lack of engagement in implementing evidence-based interventions.11,16,25 However, one of the main recommendations, particularly in cases of non-specific spinal disorders,15 involves treatment by a multidisciplinary team in Primary Health Care, with the objective of rational use of resources and avoiding the fragmentation traditionally observed in the biomedical model.7,16,31
Our findings showed that most individuals underwent imaging tests. In addition, drugs were prescribed to the vast majority, corroborating the findings from a previous study in Brazil.21 The use of medications and routine diagnostic imaging was determined to have limited evidence of clinical benefits, especially in cases of non-specific low back pain and uncomplicated spinal disorders.8,18,30,32 An interesting finding was the low prescription of muscle relaxants for back pain, which is in accordance with current recommendations and was also observed by a previous study in Brazil.33 Previous studies have shown that the unjustified use of imaging tests and medication increases direct healthcare costs9,13,34 and can be harmful due to exposure to radiation and greater likelihood of performing unnecessary surgeries, in addition to gastrointestinal toxicity and other side effects.17,35 International clinical guidelines7,19,20 and previous studies15,17,30 recommend, preferably, non-pharmacological treatment (e.g., exercise therapy) and recommend imaging tests only in cases with indications of serious spinal pathology. Thus, our findings demonstrate that there is a gap between scientific evidence and its implementation in clinical practice in Brazil.
We found that interventions such as exercise were prescribed, but without referral to a physical therapist. In addition to guidelines and studies recommending intervention strategies such as supervised exercise for non-specific spinal disorders,8,15,30 a recent Cochrane systematic review36 showed that exercise was effective in managing non-specific low back pain compared to no treatment, usual care or placebo. However, referral to a physical therapist was performed for approximately half of the individuals. Oliveira et al.21 corroborate our findings, as they also identified a low referral rate of patients with non-specific low back pain to other health professionals such as physical therapists. The physical therapist is a vital professional in the management of spinal disorders17 and contributes with the prescription of specific exercises, strategies for self-management and health education, in addition to functional diagnosis and other actions.37,38 Moreover, early referral to the physical therapist provided several benefits, such as reduced disability and pain intensity,37 further reducing the use of unnecessary clinical resources and lowering subsequent direct costs.37,38 This aspect is relevant because, although physical therapy has been part of the Family Health Support Centres since 2008, its operation is limited, e.g., the low population coverage due to the deficit in the number of professionals and the great demand imposed for conditions such as low back pain.16,39,40 It is possible to assume that these aspects explain the low frequency of referrals to this professional.
We observed an association between increasing age and greater use of Outpatient Care, as well as a greater chance of women first accessing the Emergency Department. Even though Primary Health Care is recommended as a gateway to health services and has a characteristic of longitudinal care for patients with chronic pain,1-3,25 there is the possibility of direct access to specialists in the Public Health System (SUS).41 Such access may represent competition between Primary Care and other settings and represents a challenge for the strengthening of Primary Health Care as the initial access point for health care.42 Moreover, organizational barriers in accessing Primary Care, such as shorter operating hours and long waiting lines can encourage access through other settings, such as the outpatient clinic and Emergency Department.40 With regard to women having first access via Emergency units, although previous studies33,43 reported similar findings, this was unexpected. Traditionally, men tend to neglect their health compared to women and, consequently, seek care in Emergency units only when the condition gets worse.44,45 In contrast, women have a profile of regular use of the health care system, seeking prevention and monitoring.44 It is possible to assume that these results were influenced by the smaller number of men in our sample.
Implications for policymakersThere is a worldwide effort towards the adequate management of non-specific spinal disorders, especially low back pain, aiming at saving scarce health resources and offering cost-effective interventions.7-9,18 Our findings might contribute to managers and multidisciplinary teams, as they reinforce the importance of implementing evidence-based strategies; such as avoiding low-value care such as analgesics and routine referral for imaging, and integrating pathways involving early referral to physical therapists.
It is recommended to increase efforts to improve the workforce in Primary Care in Brazil, including the increase in numbers of physical therapists, particularly in the Family Health Strategy and Family Health Support Centres. A greater prominence of this professional in this setting could contribute specifically to the reduction in drug prescriptions and unnecessary imaging tests, promoting a treatment more aligned with the best scientific evidence.
Strengths and limitationsTo the best of our knowledge, this was the first study to investigate the pathway for the management of non-specific spinal disorders within a Public Health Care Network in Brazil. In addition to the empirical originality, our findings shed some light on how care is delivered to our target population in the public system, relying on real-world data from a cohort with a 7-year follow-up.
There are limitations such as under-reporting and imprecision of data in electronic medical records. The sample consisted of the total number of individuals who entered the Outpatient Care from the investigated hospital in 2018. Therefore, the data may not be generalizable for all patients with non-specific spinal disorders treated in the network. The variable “first access” must be interpreted with caution. We cannot guarantee that this was the first access because our study started in 2012 and, prior to that year, the electronic medical record system was not consistent. Although the study started from a large sized-hospital, it is not a specialty-hospital for spinal disorders, hence, our sample size could have been larger. Therefore, we recommend future prospective studies, with an increase in the number of clinical settings investigated, and focusing on non-specific low back pain, which is the most frequent condition managed by Primary Care physical therapists in Brazil.46
ConclusionWe found that the Emergency Department was the most accessed setting by individuals with non-specific spinal disorders using the HCN of the Federal District, Brazil. Most individuals underwent a large number of imaging tests and received a high number of drug prescriptions, and individuals who used Outpatient and Primary Health Care received a lower number of drug prescriptions. Few patients were prescribed physical exercise, and only half were referred to a physical therapist. We also found that women were more likely to access the HCN for the first time via the Emergency Department, and increasing age was associated with a greater chance of accessing Outpatient Clinics as the first contact with the Network.
Coordination for the Improvement of Higher Education Personnel (CAPES) – funding code 001; FAPDF [grant n. 00193-00000814/2021-21]; UnB/DPI. The funding agencies has no role in the design and implementation of the study or in the data analysis and presentation of the results.