Duration of therapy time is an inadequate indicator of stroke rehabilitation. Steps, duration, and intensity of active therapy time may provide a better indicator of practice.
ObjectiveThis study quantified usual walking practice in terms of steps, duration and intensity of active therapy time, and distance walked during physical therapy sessions in people with sub-acute stroke undertaking inpatient rehabilitation and to examine whether usual walking practice differed depending on walking ability.
MethodsA prospective observational study was conducted across two metropolitan rehabilitation units in Australia. Twenty-four stroke survivors were observed over three physical therapy sessions. Walking ability was categorized as unassisted or assisted based on Item 5 of the Motor Assessment Scale. Walking practice was categorized as basic or advanced. Steps, duration, intensity and distance walked were measured during physical therapy sessions.
ResultsOverall, participants took 560 steps (SD 309) over 13min (SD 6) at an intensity of steps 44 steps/min (SD 17) and walked 222m (SD 143) in physical therapy. Unassisted walkers (n=6, 25%) undertook more (or trended towards more) practice of advanced walking than assisted walkers in terms of steps (MD 254 steps, 95% CI 48–462), duration (MD 5min, 95% CI 0–10), intensity (MD 18steps/min, 95% CI −8 to 44) and distance (MD 112m, 95% CI −12 to 236).
ConclusionStroke survivors undergoing inpatient rehabilitation spent approximately 20% of physical therapy actively engaged in walking practice. Those able to walk without assistance took more steps for longer, at a higher intensity.
Trial registrationACTRN12613000764730 (https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=364545).
Regaining walking ability following stroke is a key goal of stroke rehabilitation.1 The importance of task-specific repetitive practice in stroke rehabilitation is well known. If for example, the focus of the rehabilitation is to improve walking then walking practice must be undertaken.2 Recently, focus has been placed on increasing the intensity of rehabilitation which has been explored in two ways; increasing the number of repetitions completed during therapy or the duration of therapy time.
Approximately 300 repetitions of a task can be achieved in a physical therapy session after stroke.3–5 Increasing the number of repetitions or dose of practice is regarded as beneficial for motor learning.6 Certainly, for lower limb practice increasing the daily number of repetitions by even 100 repetitions has been shown to result in improvements in walking speed.5 Lower limb dose-response trials modifying the repetitions of practice have yet to be completed, although one is currently underway (NCT01915368).
Increasing the duration of therapy time or total time spent by stroke survivors in therapy by an additional 16h has been shown to improve activities of daily living in stroke survivors.7 Strategies to increase duration of therapy time include providing weekend physical therapy8 and the use of circuit classes or groups.9 However, results appear mixed. Providing weekend physical therapy at least in a rehabilitation population appears to improve patient outcomes but not necessarily reduce length of stay,10,11 for example. In contrast, a study in stroke rehabilitation pragmatically implemented weekend or circuit class therapy and found no change in patient outcomes with an extra 3–22h of therapy.12 It is possible that the required increase in duration of therapy time to be effective has been underestimated with a recent systematic review finding an additional 240% of therapy time is required to improve activity.13 Thus, there is more to be done than simply increasing the duration of therapy time.
Intensity has been defined as the amount of work completed per unit of time.14 This suggests that when referring to intensity of rehabilitation practice, what should be considered is the number of repetitions completed during a therapeutic intervention (or part thereof) or time associated with completing a therapeutic intervention. Certainly, both the number of repetitions and active therapy time (time spent actively engaged in therapeutic interventions) have been suggested as potentially useful metrics to better describe therapy dose.15 Ensuring that stroke survivors remain active during therapy may be useful for clinicians to consider as a strategy to increase practice for stroke survivors without needing to provide additional therapy duration.
Counting repetitions and monitoring active therapy time maybe a distraction for clinicians and stroke survivors alike. Physical therapists tend to overestimate the duration of therapy time and active therapy time16 while stroke survivors themselves can accurately use counters to count repetitions.17 Using counters might be feasible to count repetitions, but this does not provide an indication of active therapy time. Distance walked in a physical therapy session could be a useful proxy measure of repetitions of walking practice (steps) and could even be a possible proxy measure of active therapy time if the total duration of therapy time is unchanged. Distance walked in a physical therapy session also may be meaningful to both physical therapists and stroke survivors given the importance18 of being able to walk sufficient distances required for community walking.19
This study aimed to quantify usual walking practice in terms of repetitions (steps), duration of active therapy time, intensity of practice (number of steps per minute of active therapy time) and distance walked during physical therapy sessions in people with early sub-acute stroke undertaking inpatient rehabilitation and to investigate whether usual walking practice differed depending on walking ability.
MethodsDesignA prospective observational study was conducted with a sample of convenience of stroke survivors undergoing inpatient rehabilitation across two metropolitan sites in Australia between April and August 2013. Participants were observed across three physical therapy sessions within a one-week period by a physical therapist independent of the delivery of care to the participants. Observers were trained in the measurement and categorization of walking. They were unobtrusive and did not participate, interfere or assist with the physical therapy session. Every effort was made to minimize the effect of the observation on the prescribed physical therapy session. Treating physical therapists and participants were blinded to the aim of the study. The study was approved by institutional Human Research Ethics Committees (The Prince Charles Hospital Human Research Ethics Committee (12/QPCH/145) and The University of Queensland Institutional Human Research Ethics Approval (2012001247), Brisbane, Queensland, Australia) and was conducted in accordance with the Declaration of Helsinki. All participants provided written informed consent prior to participation in this trial. The data of this study comprises the baseline audit of Stroke-IMPACT – TRANSLATE trial (ACTRN12613000764730).
SitesOne site was an inpatient rehabilitation unit (24 beds) within a tertiary hospital and the other site was an inpatient rehabilitation unit (51 beds) within a rehabilitation hospital. Only patients housed within the inpatient rehabilitation beds in each site were recruited to this study. Sites were staffed by multidisciplinary teams including geriatricians, nursing and allied health professionals including students. Both sites provided stroke education to patients and family members.
ParticipantsPatients undergoing inpatient rehabilitation were included if they had a diagnosis of stroke, were <8 wk post stroke, were able to walk with or without a gait aid (e.g. stick) or stand by assistance, and were able to understand three-stage commands. They were excluded if unable to walk prior to their stroke, had co-morbidities that limited walking ability such as arthritis, brain injury or previous neurological condition, had unstable cardiac status, or had a planned discharge that prevented three physical therapy sessions being observed. Information such as age, sex, side of stroke, time since stroke, and walking ability were collected to describe the sample. Walking ability was categorized based on Item 5 of the Motor Assessment Scale20 as unassisted (≥4 out of 6) or assisted (<4 out of 6).
Measurement of walking practiceWalking practice undertaken during physical therapy sessions was recorded in terms of the number of repetitions (steps), duration of active walking practice and intensity of walking practice. Steps were manually counted using a clicker. Duration of active walking practice, defined as the therapy time spent actively engaged in walking practice, was measured using a stop watch. Intensity of walking practice was determined as the number of steps per minute of active walking practice time. Distance walked was measured using a calibrated trundle wheel and recorded. Walking practice was categorized as basic walking (i.e., walking on flat, firm surfaces) or advanced walking (i.e., walking backwards, walking on uneven surfaces, walking outdoors, climbing stairs or walking on the treadmill). If a category of task was not engaged in during the observed session, zero repetitions, and zero time was recorded. Total duration of the physical therapy session was also recorded.
Data analysisData were averaged across the three physical therapy sessions. Data is presented descriptively as mean (SD) or counts (%) to describe walking practice steps, duration of active therapy time and intensity. Independent sample t-tests were used to examine differences between the groups (assisted vs unassisted walkers) in walking practice (steps, duration, intensity). SPSS v23.0 was used for all analyses and statistical significance was set at <0.05 and unequal variances were assumed for between-group analyses.
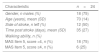
ResultsFlow of participants through the studyTwenty-six participants were recruited to this study. Data from two participants were removed from further analysis; one participant was discharged early and had only one physical therapy session observed and the other was more than 8-weeks post stroke. Characteristics of the remaining 24 participants are presented in Table 1. Six participants (25%) scored more than 4 on Item 5 of the Motor Assessment Scale, and were classified as unassisted walkers. Participants were treated by 12 physical therapists (average 10 SD8 years post-graduation). Participants spent on average 64min (SD 21) in each physical therapy session – 43min (17 SD) engaged in any practice and 13min (SD 6), or 20% of time, engaged in walking practice.
Participant characteristics.
| Characteristic | n=24 |
|---|---|
| Gender, n males (%) | 18 (75) |
| Age (years), mean (SD) | 70 (14) |
| Side of stroke, n left (%) | 12 (50) |
| Time post stroke (days), mean (SD) | 35 (27) |
| Walking ability, n (%) | |
| MAS Item 5, score <4, n (%) | 18 (75) |
| MAS Item 5, score ≥4, n (%) | 6 (25) |
MAS, Motor Assessment Scale.
Table 2 presents walking practice across the three observed physical therapy sessions in terms of steps, duration, intensity and distance walked. Overall, participants took 560 steps (SD 309) over 13min (SD 6), at an intensity of 44 steps/min (SD 17) and walked 222m (SD 143). In terms of practice of basic walking, participants took 168 steps (SD 159) over 5min (SD 5) at an intensity of 34steps/min (SD 18) and walked 55m (SD 47). In terms of practice of advanced walking, participants took 392 steps (SD 281) over 8min (SD 6) at an intensity of 47steps/min (SD 18) and walked 168m (SD 133).
Mean (SD) steps, duration, intensity and distance walked during a physical therapy session for all, unassisted and assisted walkers and mean difference (95% CI) between groups.
| Walking/session | All (n=24) | Walkers | Difference between walkers | |
|---|---|---|---|---|
| Unassisted (n=6) | Assisted (n=18) | Unassisted minus assisted | ||
| Steps (#) | ||||
| Basic | 168 (159) | 116 (91) | 185 (175) | −69 (−226 to 87) |
| Advanced | 392 (281) | 583 (172) | 328 (284) | 254 (48 to 462) |
| Total | 560 (309) | 699 (207) | 514 (327) | 185 (−112 to 483) |
| Duration (min) | ||||
| Basic | 5 (5) | 3 (2) | 6 (6) | −3 (−8 to 2) |
| Advanced | 8 (6) | 12 (5) | 7 (5) | 5 (0 to 10) |
| Total | 13 (6) | 14 (7) | 13 (7) | 1 (−5 to 8) |
| Intensity (steps/min) | ||||
| Basic | 34 (18) | 42 (28) | 31 (14) | 11 (−6 to 29) |
| Advanced | 47 (27) | 60(30) | 42 (25) | 18 (−8 to 44) |
| Total | 44 (17) | 56 (26) | 40 (11) | 17 (1 to 32) |
| Distance walked (m) | ||||
| Basic | 55 (47) | 55 (55) | 55 (45) | 0 (−47 to 47) |
| Advanced | 168 (133) | 252 (123) | 140 (128) | 112 (−12 to 236) |
| Total | 222 (143) | 306 (125) | 194 (141) | 112 (−22 to 246) |
There was no difference in total or basic walking practice between groups. Unassisted walkers undertook more (or trended towards more) practice of advanced walking than assisted walkers in terms of steps (p=0.02), duration (p=0.07), intensity (p=0.16) and distance (p=0.07) (Table 2).
DiscussionThis study aimed to quantify usual walking practice in terms of repetitions, duration and intensity of active therapy and distance walked during physical therapy sessions in ambulatory stroke survivors with early sub-acute stroke undertaking inpatient rehabilitation and to examine whether usual walking practice is dependent on walking ability. Stroke survivors spent two-thirds of physical therapy sessions actively engaged in practice, of which nearly a third was walking practice, where they took 560 steps to walk 222m. There was no influence of walking ability on the practice of basic walking undertaken, but walkers who needed no assistance were able to undertake more practice of advanced walking, particularly in terms of steps and duration.
It is promising that stroke survivors in our study spent two-thirds of their physical therapy session actively engaged in practice. A systematic review of 7 studies across 8 countries found stroke survivors were active for approximately 60% of a physical therapy session.21 Stroke survivors in our study spent 13min actively engaged in walking practice which is at the upper end of the range of 4–15min reported by Kaur et al.21 Similarly the number of repetitions (steps) in our study is similar to repetitions reported in previous studies.5,22 Although the intensity of walking has not been reported, our findings are likely to be in line with previous studies, since the number of steps and duration of walking is similar.
Providing repetitive, high-intensity, task-specific practice is key to driving drive motor learning6 which underpins recovery from stroke. Increasing the duration of therapy time is not feasible in traditional 1:1 therapy models. However, other models such as semi-supervised practice,23 circuit classes,12,24 or weekend therapy9,25 may increase the duration of therapy time. Against this happening is the reality that the duration of therapy time appears to have changed little in the last 10 years.26 Increasing the intensity of walking practice may be an alternative strategy to increase the practice dose. High intensity walking practice has been investigated in terms of treadmill training,27,28 aerobic exercise training29 or most recently, interval training.30 It may be useful to monitor the repetitions undertaken in order to use the information to drive intensity. Accelerometers, pedometers and other similar devices offer clinicians a possible application for measuring steps and intensity of walking practice. Although many different devices exist31 some commercially available devices can be reliably used with stroke survivors.32
Perhaps not surprisingly, we found that unassisted walkers were able to complete more steps at a higher intensity compared with assisted walkers. Previous research has found that walking ability influenced time spent in advanced walking activities.26 This raises the question of how to increase the intensity of walking for the more severely disabled walker after stroke, i.e., how can we enable them to complete as many repetitions within the time available. One strategy is treadmill training because it is a high-intensity intervention compared with overground walking regardless of walking ability27,33 and has been shown to be effective across the continuum of walking ability.34
Only the duration of physical therapy time was investigated in this study yet stroke survivors spend much of their time not engaged in therapeutic activities.35 Stroke guidelines recommend that survivors undergoing sub-acute rehabilitation complete at least 2h of active task practice per day.36 Regardless of whether this target is met, a substantial amount of time remains unaccounted for. Several factors have been identified by stroke survivors, carers and staff in inpatient rehabilitation that affects the ability of stroke survivors to engage in tasks outside therapy time.37 Addressing issues such as increasing the patient's motivation and knowledge, providing an enriched environment and developing daily routines may provide structure to facilitate active practice outside therapy. Older adults admitted to sub-acute rehabilitation with mixed diagnoses including stroke spent a median of between 33 and 43min/day walking.38 Our findings suggest that approximately 30% of this walking practice is occurring in physical therapy. Additionally, the number of steps completed in physical therapy falls short of what is completed in the first few weeks following discharge from hospital39 and by stroke survivors40 and older adults41 living in the community. Similarly the distance walked during a physical therapy session falls short on what is required for community ambulation.42
This study is not without its limitations. This was a small sample of convenience of ambulant stroke survivors recruited from two rehabilitation units located in the same metropolitan area with only a small proportion of participants able to walk with no assistance on admission to the study. Results from this study are unlikely to be generalizable to stroke survivors unable to walk or requiring hands on physical assistance of a therapist to walk such as facilitating the movement of the paretic lower limb. The study recruited all eligible participants admitted to each rehabilitation unit, so that the sample is likely to be representative of people in the sub-acute stage of stroke undergoing inpatient rehabilitation. Direct observation was used to collect data. We attempted to minimize any change in behaviour by blinding therapists and participants to the aims of the study, but it is possible that physical therapist and/or stroke survivor behaviour changed despite our attempts.
In summary, stroke survivors spend approximately 20% of a physical therapy session actively engaged in walking practice. Those able to walk without assistance take more steps at a higher intensity. Consideration needs to be given to intensity of walking rehabilitation practice to maximize opportunities to drive neuroplasticity.
FundingThis study was supported by a OHMR Physiotherapy Project, Grant 2012–2015.
Conflicts of interestThe authors declare no conflicts of interest.
Nicole Cox and Annette Stouter for their assistance with data collection and cleaning.