Scapular focused exercise interventions are frequently used to treat individuals with shoulder pain. However, evidence for changes in scapular motion after intervention is limited.
ObjectiveTo compare the effects of scapular movement training versus standardized exercises for individuals with shoulder pain.
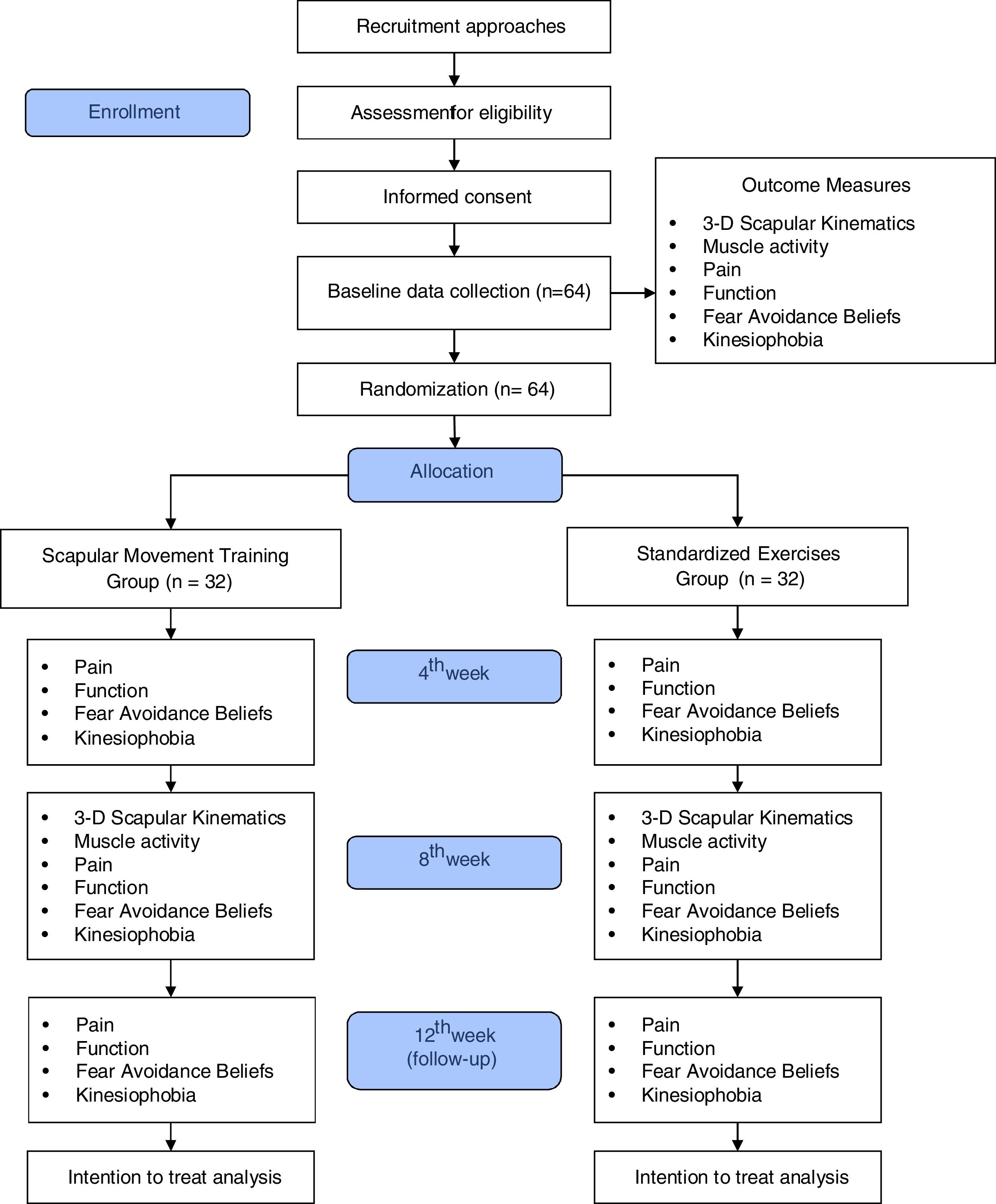
MethodsThis will be a single-blinded randomized controlled trial. Sixty-four individuals with shoulder pain for at least 3 months, scapular dyskinesis, and a positive scapular assistance test will be randomly allocated to one of two groups: Scapular Movement Training (group 1) and Standardized Exercises (group 2). Group 1 will receive education about scapular position and movement, and be trained to modify the scapular movement pattern. Group 2 will perform stretching and strengthening exercises. Both groups will be treated twice a week for eight weeks. Three-dimensional scapular kinematics and muscle activity of the serratus anterior and upper, middle, and lower trapezius during elevation and lowering of the arm will be assessed at baseline and after 8 weeks of treatment. Pain intensity, function, fear avoidance beliefs, and kinesiophobia will be assessed at baseline and after 4 and 8 weeks of treatment, and 4 weeks after the end of treatment.
ConclusionsThe results of this study may contribute to a better understanding of the efficacy of scapular focused treatments for individuals with shoulder pain. Clinical trial registration: NCT03528499
Shoulder pain is a common musculoskeletal complaint.1,2 The annual incidence of the condition in primary medical care is estimated to be 20.6 per 1000 individuals.3 The prevalence is between 20 and 33% in the general population, and it may have an impact on work productivity and healthcare expenses over time.4,5
Appropriate scapular motion is essential for shoulder mobility and function.6,7 Although scapular dyskinesis has already been associated with shoulder pain,8,9 it is not clear in the literature if scapular dyskinesis is the cause or consequence of shoulder pain.8 Scapular dyskinesis has been suggested to increase the risk for developing shoulder pain in athletes,9 and this may also be the case for the general population. Although more cohort studies are needed to provide more evidence about the role of scapular motion in shoulder pain, individuals with shoulder pain have shown decreased scapular posterior tilt, upward rotation, and external rotation during arm elevation compared to individuals without shoulder pain.6,10–12 However, other studies have identified different movements impairments, or no deviations.6,13 Increased activation of the upper trapezius (UT)14–17 and decreased activation of the serratus anterior (SA),14,16–18 and lower (LT) and middle trapezius (MT)19,20 have also been described and may contribute to shoulder pain and alterations in scapular motion.
Evidence for strengthening and stretching exercises as the most recommended management strategy to improve pain and disability in individuals with shoulder pain is currently increasing.21–23 However, the effectiveness on shoulder pain and disability has not been related to changes in scapular motion.24–28 Although pain and function improvements are more meaningful to patients than scapular motion, it is not clear yet whether scapular motion is a modifiable contributing factor to shoulder pain.27,29 One of the major issues in the past investigations is that scapular motion was not associated to shoulder symptoms during the clinical evaluation process to guide exercise prescription.24–26,28,30–33 Therefore, an approach that specifically targets scapular motion deviation that is likely related to the individual’s symptoms may be more effective to restore normal scapular motion.
The movement-based classification system follows the kinesiopathologic model that creates a diagnostic classification related to the movement impairments that are the cause of, or consequence of the patient’s pain or dysfunction.34,35 This classification then leads directly to the intervention approach (i.e. targeting to change the movement impairments). This model has been used to treat individuals with shoulder pain and showed positive effects on pain,31,36 function,30–33 and scapular motion.33,37 However, the effects of movement-based approach on scapular kinematics and muscle activity have not been compared to scapular strengthening and stretching exercises, which are frequently used in clinical practice for shoulder rehabilitation and have effectively improved pain and function.21–23 In addition, the assessment of fear avoidance and kinesiophobia is also important, as these aspects may play a role in the symptoms, prognosis, and clinical conditions of individuals with shoulder pain.38,39
The objective of this study will be to compare the effects of scapular movement training to standardized exercises on scapular kinematics, scapulothoracic muscles activity, pain, disability, fear avoidance, and kinesiophobia in individuals with shoulder pain. We hypothesized that scapular movement training will result in greater improvements compared to standardized exercises on scapular kinematics, scapulothoracic muscles activity, pain, disability, fear avoidance, and kinesiophobia.
MethodsStudy settingThis will be a single-blind randomized clinical trial, with two-arm parallel groups and a blinded assessor. The trial has been designed according to the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT)40 and CONSORT41 guidelines. This trial was prospectively registered at clinicaltrials.gov (NCT03528499).
Study settingThe study will be conducted at the Laboratory of Analysis and Intervention of the Shoulder Complex at Universidade Federal de São Carlos.
Sample size calculationThe sample size was calculated based on estimated mean difference of 5.5° (standard deviation of 7.2°) in the scapular posterior tilt between groups, collected via an electromagnetic system device,42 with two-tailed significance set at 0.05, power at 80%, and accounting for a 15% dropout. Thirty-two individuals are needed per group. Scapular posterior tilt was considered for sample size calculation because it is commonly decreased in individuals with shoulder pain.6,10,11,16
Eligibility criteriaA physical therapist with seven years of clinical experience will screen eligibility of potential participants, according to the following criteria: individuals of both sexes, between 18–60 years old, with shoulder pain during arm elevation for at least 3 months and at least 3 points measured using a 0 to 10-point Numerical Pain Rating Scale (NPRS),43 presence of scapular dyskinesis,44 positive Scapular Assistance Test (SAT),45 and be able to elevate the arm at least 150°.
Scapular dyskinesis will be assessed with the individuals elevating both arms simultaneously to a 3-second count using the “thumbs up”, and then lowering to a 3-second count.44 At first, each individual will perform 5 repetitions of arm elevation in each plane (sagittal and frontal planes) with no weight in hands, followed by 5 more repetitions also in each plane of arm elevation with weight in hands. The planes will be randomly chosen, and the weight will be determined according to the body weight of the individual: 1.4 kg for those weighing <68.1 kg, and 2.3 kg for those weighing 68.1 kg or more. Scapular dyskinesis will be considered present when prominence of medial and/or superior scapular border, inferior scapular angles, rapid scapular downward rotation, or excessive clavicular elevation could be observed in 3 of 5 trials. The interrater reliability of this test showed an agreement between 75% and 82%, and kw from 0.48 to 0.61.44
The SAT will be performed as previously described46,47 and considered positive when pain intensity reduces 2 or more points on the NPRS during assisted elevation as compared to elevation with no assistance.
The exclusion criteria will be body mass index higher than 28 kg/m2,17 history of fracture and/or surgery in the shoulder region,26 history of shoulder dislocation and/or instability (positive apprehension test and/or sulcus test) and/or massive rotator tears (positive drop-arm test),26 pregnancy,26 adhesive capsulitis, numbness or tingling of the upper limb reproduced by the cervical compression test or upper limb tension test,26 systemic or neurologic illness,26 corticosteroid injection within 3 months prior to the intervention, physical therapy within 6 months prior to the intervention,26 and self-reported tape allergy. All eligible individuals will receive information about the study from one of the researchers, and those who accept to participate will sign an informed consent form before participation.
Individuals will be discontinued from the study if they present fractures, surgeries, musculoskeletal injuries, neurological diseases, other injuries that prevent attendance at sessions, or receive a corticosteroid injection at the shoulder complex during the treatment or follow-up periods. Individuals excluded, discontinued, or who complete study follow-up with remaining shoulder symptoms will receive written and verbal information about shoulder pain management and exercises.
ProceduresIndividuals will be recruited through flyers placed at the University buildings, local orthopedic clinics and community public places located in Universidade Federal de São Carlos. Advertisements in local newspapers and radio, and online resources (eg, university intranet and social media) will also be used to recruit patients.
Included participants will undergo a baseline assessment prior to randomization. Outcomes will be collected at each time point according to Fig. 1. The most self-reported painful shoulder will be considered for all outcome measures in those with bilateral symptoms.
Outcome measuresThe primary outcome measures will be 3-D scapular kinematics. The secondary outcome measures will be scapular muscle activity, pain, disability, fear avoidance beliefs, and kinesiophobia.
Three-dimensional scapular kinematicsThe TrakSTAR hardware (Ascension Technology Corporation, Burlington, VT) integrated with the MotionMonitor software (Innovative Sports Training, Inc, Chicago, IL) will be used to assess 3-D scapular kinematics. The 3-D position and orientation of each sensor will be tracked simultaneously at a sampling rate of 100 Hz. The 3-dimensional scapular tracking methodology is described elsewhere.42 This procedure has been shown to be reliable over time during elevation and lowering of the arm in individuals with shoulder pain with intraclass correlation coefficient (ICC) ranging between 0.54 and 0.85, standard error of measurement between 3.6° and 7.4°, and minimal detectable change between 8.4° and 17.2°.42 The 3-D scapular kinematics and EMG data will be collected during three cycles of arm elevation and lowering, with duration of approximately 3 s for each phase, in the sagittal, scapular, and frontal planes, and with individuals standing in front of the transmitter.42
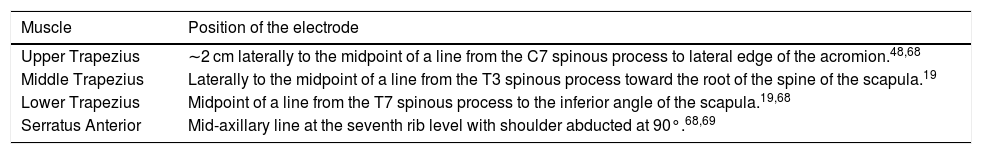
Muscle activityMuscle activity of the UT, MT, LT, and SA will be measured during elevation and lowering of the arm using Trigno TM Mobile System, DelSys®, Boston, USA. Electromyography (EMG) electrodes will be attached to the individual’s skin using double-sided tape. Position of each electrode is described on Table 1.
Position of the EMG electrodes.
| Muscle | Position of the electrode |
|---|---|
| Upper Trapezius | ∼2 cm laterally to the midpoint of a line from the C7 spinous process to lateral edge of the acromion.48,68 |
| Middle Trapezius | Laterally to the midpoint of a line from the T3 spinous process toward the root of the spine of the scapula.19 |
| Lower Trapezius | Midpoint of a line from the T7 spinous process to the inferior angle of the scapula.19,68 |
| Serratus Anterior | Mid-axillary line at the seventh rib level with shoulder abducted at 90°.68,69 |
For normalization of the data, a reference submaximal contraction will be collected at 90° of arm elevation in the scapular plane19 with the individual holding an 1 kg dumbbell for 5 s.48 Two trials will be collected with 1 min of rest in between.19 The weight and duration for the submaximal contractions was based on a previous study.48
EMG signals acquisition will be synchronized with scapular kinematics (MotionMonitor®) at 2000 Hz and a voltage gain of 1000. Data will be processed using Matlab (version 2015, The Mathworks Inc., Natick, MA, USA), filtered with a 6th order zero-lag Butterworth filter in the 20−450 Hz band, and a notch filter centered on 60 Hz and harmonics. Signals will be converted into root-mean-square using 100 millisecond moving windows with overlap of 99.5%, and normalized as a percentage of the average of the reference contractions.48
Pain scoresShoulder pain at rest and during arm elevation and the worst and the least pain during the past week will be assessed with the NPRS, which is a valid and reliable scale for individuals with shoulder pain. The minimal clinically important difference (MCID) is 2 points or a 30% change score.49,50
Disability of the upper limbDisability of the upper limb will be assessed with the Brazilian version of Disabilities of the Arm, Shoulder and Hand (DASH), which is valid and reliable to assess individuals with upper limb disorders.51 Final score ranges from 0 to 100, where higher scores indicate higher disability. The MCID is 10.8 points.52
Fear-avoidance beliefsFear-Avoidance Beliefs will be assessed with the Brazilian version of Fear-Avoidance Beliefs Questionnaire.53 This questionnaire is divided in two subscales: physical activity and work. The score of the physical activity subscale ranges from 0 to 24, and the work subscale ranges from 0 to 42.53 Higher scores of this questionnaire indicate worse conditions. The Brazilian version was shown to be reliable for test-retest.53
KinesiophobiaThe Brazilian version of the Tampa Scale for Kinesiophobia will be used to measure kinesiophobia.54 The score ranges from 17 to 68 points, where higher scores indicate worse conditions. This version of the scale was considered reliable for test-retest.54
Global rating of change scaleThe individual’s perception of improvement/deterioration over time will be measured with the Global Rating of Change Scale. They will be asked to rate the overall change in their shoulder condition from baseline evaluation. This scale ranges from −7 to 7, where positive and higher scores indicate higher perception of health improvement, negative and lower scores indicate worsening of health perception, and zero means no change.55
Random allocationPatients will be randomly assigned to one of the two groups: Scapular Movement Training Group or Standardized Exercises Group. Randomization will be computer-based and conducted at a 1:1 ratio according to a random sequence generated by the website http://www.randomization.com, stratified by age (< or ≥50 years)56 and sex (female or male). An independent researcher, not involved in the treatment or assessment, will perform the randomization process and prepare the consecutively numbered sealed opaque envelopes with group allocation. The envelopes will be securely stored and will be opened in sequence to reveal group allocation prior to the first treatment session by the researcher responsible for the treatments.
BlindingThe assessor and the statistician will be blinded to treatment group assignment. Patients will be treated individually and blinded to the study hypothesis.57 Circumstances that unblinding is permissible have not been planned.
InterventionsIndividuals of both groups will attend 16 individualized treatment sessions, at a frequency of twice a week for 8 weeks, with at least one-day interval between sessions. If the participants miss a treatment session, it will be rescheduled. The estimated duration of each treatment session will be 45−60 min. The therapist will manage symptoms by applying ice or reducing active trigger points through deep friction in the deltoid and upper trapezius as necessary.58,59 Two physical therapists will be responsible for delivering the interventions. The therapist who will be in charge of the scapular movement training has 10 years of clinical experience, and specializations in sports rehabilitation and manual therapy. The therapist who will be in charge of the standardized exercises group has five years of clinical experience, and residency in orthopedics rehabilitation. Both therapists will receive 6 h training about shoulder rehabilitation and scapula movement impairments by the principal investigator. To improve adherence to the protocol, participants retention and complete follow-up, the participants will receive face-to-face adherence reminders in every session, and/or cellphone reminders or text messages. We have not planned any change on the intervention protocols.
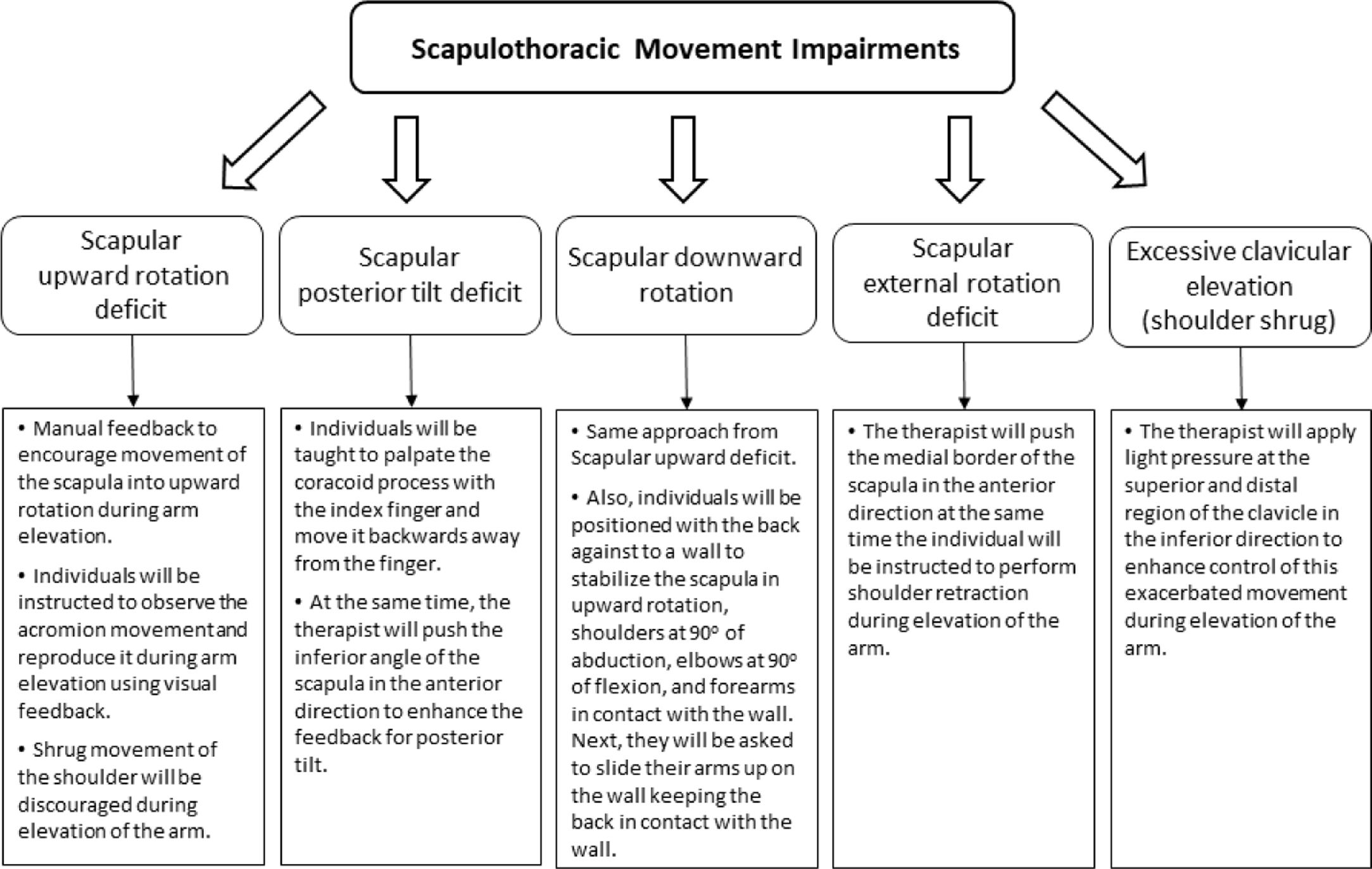
Scapular movement training groupThe scapular movement training will be divided in two phases: educational phase in the first week of treatment and scapular movement training phase during the remaining weeks (Supplemental material online and Fig. 2).
In the educational phase, instructions about proper scapular position in the rest position and during arm elevation, as well as muscle activation during elevation of the arm will be delivered to each individual (Fig. 2). The instructions will be reinforced with verbal, tactile, and visual feedback with the aid of a mirror, anatomical models, and EMG. During the pilot of this study, the ability to learn and control scapular motion and muscle contractions varied between individuals. Therefore, it would not be possible to standardize the number of repetitions and movements for all participants during the educational phase. Detailed information of the treatment protocol is described in Supplemental online material.30–33,37,60Fig. 2 displays a diagram of the approaches based on the scapular movement impairments.
Scapular movement training phase: This phase will aim to improve scapular movement pattern during arm elevation and during a functional activity relevant and chosen by the patient. The exercises will be performed with slow, conscious, and paced movements in 3 sets of 10–15 repetitions, or until the individual report muscle fatigue.31,33 The exercises will progress in the following order according to the individual ability to control scapular movements and to reach full range of arm elevation: wall slide, arm elevation with elbow flexion, arm elevation with elbow extension, and arm elevation against resistance. The therapist will supervise all exercises to guarantee proper execution.
EMG biofeedback will be used in the education and training phases. EMG sensors (Trigno TM Mobile System, DelSys®, Boston, USA) will be placed at the same muscles and positions as previously described to allow individuals to observe their muscles activations. The EMG signals will be displayed at real-time on a screen, showing amplitude (Y-axis) and time (X-axis). The therapist will give verbal instructions and tactile feedback to assist the individuals to increase SA, LT, and MT activation and decrease UT activation. As soon as the individuals are able to control their scapular muscles by themselves the EMG biofeedback will no longer be used.32 The individuals allocated in this group will not receive any additional strengthening exercises or intervention targeting other impairments.
Standardized exercises groupThis group will perform stretching and strengthening exercises commonly used to treat individuals with shoulder pain (Appendix A, Supplementary data).26,61 The self-stretching exercises will address the UT,26 pectoralis minor,25 and posterior shoulder.62 Each stretch will consist of 3 repetitions of 30 s, with an interval of 30 s between repetitions.
The strengthening exercises will be performed using elastic resistance bands (Theraband ®) with 4 progressive levels of resistance: red, green, blue, and gray. The resistance will be progressed through the colors when the sets are performed easily (with no muscle fatigue reported by the individual).26 The therapist will ask the level of effort to perform the exercises and if it would be possible to increase the level of resistance. Three sets of 10 repetitions for each exercise will be completed, with 1 min of rest between sets. The following exercises will be performed: prone extension,63 prone horizontal abduction with external rotation,63 serratus punch,64 and side-lying external rotation.63
Data managementData about recruitment, characteristics of the individuals who will complete or dropout of the study, as well as the outcome measures will be stored in a secure place at Universidade Federal de São Carlos. All data will be entered into a computer software (Excel™ Microsoft, 2016) and weekly double-checked by an assistant, using standard coding to ensure the confidentiality of the participants. Also, only the researchers involved in this study will have access to the database.
Statistical methodsAnalysis of the effects of treatmentThe statistical analysis will be performed using Statistical Package for the Social Sciences version 24.0 (SPSS Inc, Chicago, IL). Mean ± standard deviation (SD) values and 95% confidence interval (CI) will be calculated for continuous data. Data normality will be tested by visual inspection of histograms and using the Shapiro-Wilk´s test. The significance level will be 0.05 for all statistical analyses.
The statistical analysis will follow the principles of intention-to-treat analysis. Three-D scapular kinematics, scapular muscle activity, pain, disability, fear avoidance beliefs, and kinesiophobia will be the dependent variables. Data analysis for scapular orientation and muscle activity will be performed for selected angles of humerothoracic elevation (30°, 60°, 90°, and 120°) and lowering (120°, 90°, 60°, and 30°). The between-group differences (treatment effects) and their respective 95% CIs will be calculated by multilevel linear mixed models.65 For kinematics and EMG outcomes, longitudinal models will be constructed using fixed effects for group, angle, and group versus angle interaction terms, with baseline values used as covariate to the adjustment of the model. For clinical outcomes, models will be constructed using group, time, and interaction term of group versus time as fixed effects. For all models, individuals will be modeled as random effects. If the residual distribution violates the assumptions for the mixed linear models, data will be analyzed using repeated measures Analysis of Variance (ANOVA). If data are not normally distributed, statistical analysis will be performed using non-parametric correspondent tests.
Data monitoringAn independent researcher will monitor data collection progress and safety. No interim analyses have been planned. Data will be analyzed when all recruitment and data collection are done.
HarmsAll self-reported adverse effects will be registered by the therapists and/or assessor and reported to the Human Research Ethics Committee from Universidade Federal de São Carlos, São Carlos, São Paulo, Brazil. Use of pain medication, ice, and hot pack during of the study will also be recorded.
AuditingAn independent researcher will monitor the progress of the study every 6 months, and audit the quality and completeness of the data, and verify if all steps of the protocol is being followed as planned.
EthicsThis protocol was approved by the Human research Ethics Committee of the Universidade Federal de São Carlos (CAAE: 86974318.7.0000.5504). Any protocol modifications will be reported to the Human research Ethics Committee and to the trial registry.
Dissemination policyThe study will be disseminated through publication in journals, as well as presentations in conferences. The data of this study will be shared under reasonable request. The researchers that substantively contribute to the design, conduct, interpretation, and reporting of a clinical trial will be considered an author on the final study.
DiscussionAlthough physical therapy is the first recommended treatment to patients with shoulder pain, the rate of full recovery of these patients is still far from ideal.1,66,67 If the scapular movement training can significantly improve scapular kinematics and function, and reduce pain, as compared to standardized exercises, the results might support the clinical application of this intervention for individuals with shoulder pain and scapular dyskinesis. These findings may assist therapists and health care providers to choose better treatment strategies for this population.
Strengths and weaknesses of the studyThis high quality randomized controlled clinical trial will provide important information about scapular movement training efficacy on scapular biomechanics and clinical outcomes. This study will provide evidence of simple shoulder exercises and feedback for specific scapular movement alterations, both consistent with clinical practice. Moreover, the randomization of this clinical trial is blinded and stratified by age and sex, two variables that may influence the prognosis.56 Finally, the calculated sample size will provide the appropriate statistical power to detect differences in the primary and secondary outcomes. Also, the outcomes may contribute to the design of further studies on clinical and biomechanics changes resulting from scapular focused approaches. Moreover, we believe that this study will contribute to the evidence-based practice of scapular focused-approach in individuals with shoulder pain and scapular dyskinesis.
Unfortunately, due to the nature of the interventions, we will not be able to blind therapists and patients for treatment allocation. Furthermore, effective dosages of exercise interventions and movement training are unknown, and the criteria of assessments for specific movement pattern deviations are not well established in the literature. Deep friction will be used when myofascial trigger point is found on the upper trapezius and deltoid. However, it may systematically influence the pain and muscle stiffness of both groups. Finally, this study will treat individuals with chronic shoulder pain, scapular dyskinesis, and positive scapular assistance test, and the findings of this study might not be applicable for individuals with different characteristics.
Conflict of interestThe authors have no conflicts to disclose.
The trial was supported by the São Paulo Research Foundation (Grant 18/07571-7, Fellowship 2018/04911-1), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES), and Conselho Nacional de Desenvolvimento Científico e Tecnológico - CNPq (142373/2018-4).