Weaning a patient from mechanical ventilation is a complex procedure that involves clinical and contextual aspects. Mechanical ventilation also depends on the characteristics of health professionals who work in intensive care.
ObjectiveThis study described the organizational aspects associated with the physical therapist's performance in the weaning procedure from mechanical ventilation and extubation in neonatal, pediatric and mixed (neonatal and pediatric) intensive care units in Brazil.
MethodsIn order to identify the existing intensive care units in Brazil, data from the National Health Facilities Census was used to enable the researchers to obtain information about registered units. A cross-sectional survey was carried out by sending an electronic questionnaire to 298 neonatal, pediatric and mixed intensive care units in Brazil.
ResultsThis study assessed questionnaires from 146 intensive care units (49.3% neonatal, 35.6% pediatric and 15.1% mixed). A total of 57.5% of these units applied mechanical ventilation weaning protocols, and a physical therapist frequently conducted this procedure (66.7%). However, the clinician responsible for conducting the weaning and deciding when to do extubation varied regardless of ICU patient age profile. Regardless of the type of hospital or the type of units, most of these had a dedicated physical therapist. However, physical therapy care 24h/7 days per week was predominantly in pediatric intensive care units (56.0%), and in public hospitals (45.9%). Moreover, when the physical therapist was available 24h/7 days per week, (s)he was responsible for the mechanical ventilation extubation decision and patients were successfully extubated on the first attempt.
ConclusionIn this survey, intensive care units using physical therapy assistance 24h/7 days per week were associated with the use of a mechanical ventilation weaning protocol, an extubation decision and success commonly on the first attempt of extubation.
Mechanical ventilation (MV) is the main ventilation resource used to treat newborn and children admitted to Pediatric and Neonatal Intensive Care Units (PICUs and NICUs).1–3 Even though MV has saved many lives, it has also been associated with complications such as lung injury, pneumonia, cardiovascular instability due to cardiopulmonary interaction, morbidities in neurodevelopment, and injury to the respiratory tract associated with the endotracheal tube.3,4 Therefore, it is advisable to discontinue ventilation support as soon as possible.4
Weaning is an important stage of MV representing 40% of the ventilation support total time.5 Weaning a patient off MV is a complex process which combines clinical aspects (i.e. guidelines and evidence-based protocols), contextual aspects (i.e. organization, resources and professional team) and healthcare providers’ skills (i.e. education, combination of competence/experience and professional relationships).6
For the clinical aspects, there is a large variability in the clinical application of MV weaning protocols,7 hence, there is no agreement on when weaning procedure should start. Evidence of effective methods for weaning patients off MV as well as guidelines/recommendations of tests which determine the best timing or readiness for extubation, both in pediatrics and neonatology, is still necessary.8,9
For the contextual and professional aspects, MV weaning and extubation procedures may vary according to the structure of the unit, availability of a skilled professional team, the type of patients being assisted, and medical and nursing leadership models. Such factors will influence the definition of professional roles and responsibilities for MV weaning and extubation.6
Previous studies6,10–13 have presented the role of non-medical clinicians in decisions related to MV protocols and the weaning procedure. In Brazil, few studies have assessed the practice related to MV weaning procedures and the characteristics of physical therapists who assist in adult14–16 and neonatal17 Intensive Care Units (ICUs). There is no study to the authors knowledge describing the participation of physical therapists in performing MV weaning and extubation procedures on pediatric or neonatal units. Therefore, the aim of this study was to identify and assess the characteristics associated with the involvement of physical therapists in MV weaning and extubation procedures in pediatric and neonatal ICUs in Brazil.
MethodsStudy designA cross-sectional survey was carried out from January 22, 2016 to November 1, 2016. This study was approved by the Research Ethics Committee from the Universidade Federal de Uberlândia (UFU), Uberlândia, MG, Brazil (#1.301.015).
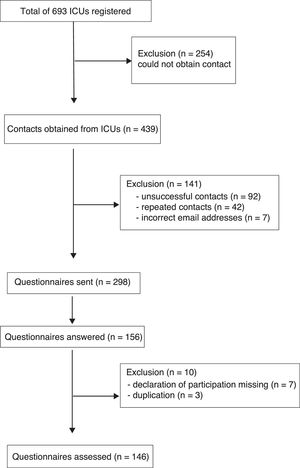
ParticipantsIn order to identify the existing ICUs in Brazil, data from the National Health Facilities Census was used to find information on 693 registered ICUs, consisting of 337 NICUs, 323 PICUs and 33 mixed PICUs (i.e. provide assistance to both newborns and pediatric patients).18 A minimum number of 82 ICUs,19 that also covered all states in Brazil, was calculated as the minimum sample size for this study. A significance level of 0.05 was adopted, as well as standard test power (1−β=0.95) for the sample calculation.
Of the 693 registered ICUs, 439 coordinators contacts (email or telephone) were obtained. It was not possible to get the individual contact of the person in charge of 254 units. Of the 439 contacts, 141 were excluded due to unsuccessful communication attempts, incorrect data or duplicate contacts (different professionals from the same ICU). Thus, 298 questionnaires were sent to the coordinators or professionals (physical therapists, physicians or nurses) in charge of each ICUs. Only one of these could represent the hospital facility. Out of 298, 156 (52.3%) answered the survey, but 10 responses were excluded (3 due to duplicity from the same unit and 7 due to the absence of the authorization statement). Therefore, 146 (48.9%) ICUs took part of the study (Fig. 1). The survey included those ICUs whose head clinician signed and forward to the researchers the consent form for this study.
Questionnaire/SurveyThe method of assessment was an electronic questionnaire created by the researchers, using the on-line Google™ Drive Form search toll. The self-administered questionnaire was made available by a link sent to the coordinators or clinicians in charge of the ICUs. After the initial invitation, emails with reminders and/or telephone texts were sent periodically to the ones who had not participated, until reaching a minimum sample in each state of the country.
The questionnaire contained closed and open-ended questions asking about characteristics of the ICUs and the role of physical therapists in performing MV weaning and extubation procedures. A pilot-test with 10 professionals representing each ICU type and each professional category was carried out to correct confounding factors in the questionnaire questions. The final version of the survey can be obtained from authors upon request.
Statistical analysisThe χ2 test of multiple comparisons amongst percentages20 was used to compare categorical variables. The descriptive results were presented as frequency and percentage. Multiple comparisons of percentages were carried out in the R free Software (R Development Core Team, 2017).21 A significance level of 5% was adopted to all analysis.
ResultsCharacteristics of Intensive Care UnitsA total of 146 ICUs participated in this survey. Of those, 72 (49.3%) were NICUs, 52 (35.6%) were PICUs, and 22 (15.1%) were mixed PICUs. The overall characteristics of the physical therapist working times, whether a single professional or team more commonly assisted with the MV weaning and extubation procedures, the protocol usage, and the number of extubation attempts are presented in Table 1. Regarding the type of medical facility housing the ICUs that were analyzed, 77.3% were public facilities and 22.6% were private facilities.
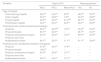
Data related to ICUs answering the study's questions (N=146), regarding MV weaning and extubation procedures/protocols.
| n (%) | |
|---|---|
| Professional who answered the questionnaire | |
| Physician | 92 (63.0) |
| Physical therapist | 49 (33.6) |
| Nurse | 5 (3.4) |
| Experience of the professional who answered the questionnaire | |
| Under 5 years | 16 (11.0) |
| Over 5 years | 130 (89.0) |
| Specialist degree | |
| Yes | 124 (84.9) |
| No | 22 (15.1) |
| Type of hospital | |
| Public teaching hospital | 50 (34.2) |
| Public hospital | 38 (26.0) |
| Private hospital | 33 (22.6) |
| Philanthropic hospital | 25 (17.2) |
| Are there physical therapists in the ICU? | |
| Yes, physical therapist who is dedicated to the ICU | 118 (80.8) |
| Yes, physical therapist who is not dedicated to the ICU | 27 (18.5) |
| No | 1 (0.7) |
| Physical therapy coverage (h/day) in the ICU (n=145) | |
| 24h/day | 62 (42.7) |
| 18h/day | 30 (20.7) |
| <18h/day | 52 (35.9) |
| No information provided | 1 (0.7) |
| Professional who carried out weaning procedures | |
| Physician | 25 (17.1) |
| Physical therapist | 3 (2.1) |
| Physician and physical therapist | 100 (68.5) |
| Physician and nurse | 0 |
| Multiprofessional team | 18 (12.3) |
| Use of MV weaning protocol | |
| Yes | 84 (57.5) |
| No | 61 (41.8) |
| No information provided | 1 (0.7) |
| Professional who decided the extubation procedures | |
| Physician | 67 (45.9) |
| Physical therapist | 2 (1.4) |
| Physician and physical therapist | 71 (48.6) |
| Physician and nurse | 0 (0.0) |
| Multiprofessional team | 6 (4.1) |
| Frequency of extubation attempts | |
| Most patients are successfully extubated on the first attempt | 130 (89.0) |
| Most patients require up to 3 attempts | 13 (8.9) |
| Most patients require more than 3 attempts | 0 (0.0) |
| No information provided | 3 (2.1) |
Results are presented in absolute number (n) and percentages (%).
ICU, Intensive Care Unit. MV, Mechanical ventilation.
Table 2 contains the percentage of professionals who performed the MV weaning procedure and made the decisions concerning the extubation procedure in the 3 types of ICUs and regarding the use of weaning protocols.
Comparison between types of ICUs, use of MV weaning protocol and other variables.
| Variables | Types of ICU | Weaning protocol | |||
|---|---|---|---|---|---|
| NICU | PICU | Mixed PICU | Yes | No | |
| Type of hospital | |||||
| Public teaching hospital | 48.0aA | 46.0aA | 6.0bB | 48.0aA | 52.0aA |
| Public hospital | 55.3aA | 36.8bA | 7.9cB | 63.2aA | 36.8bA |
| Private hospital | 48.5aA | 30.3aA | 21.2aAB | 69.7aA | 30.3bA |
| Philanthropic hospital | 44.0aA | 20.0aA | 36.0aA | 54.2aA | 46.8aA |
| Professional who carried out weaning procedures | |||||
| Physician | 52.0aA | 32.0abA | 16.0bA | 45.8aA | 54.2aA |
| Physical therapist | 66.7aA | 33.3bA | – | 66.7aA | 33.3aA |
| Physician and physical therapist | 45.0aA | 39.0aA | 16.0bA | 60.0aA | 40.0bA |
| Physician and nurse | – | – | – | – | – |
| Multiprofessional team | 66.7aA | 22.2bA | 11.1bA | 61.1aA | 38.9aA |
| Professional who decided the extubation procedures | |||||
| Physician | 41.8aA | 40.3aA | 17.9bA | – | – |
| Physical therapist | 100.0A | – | – | – | – |
| Physician and physical therapist | 54.9aA | 32.4bA | 12.7cA | – | – |
| Physician and nurse | – | – | – | – | – |
| Multiprofessional team | 50.0aA | 33.3aA | 16.7aA | – | – |
Note: Proportions in the columns followed by the same superscript upper-case letter do not differ statistically from each other by the multiple comparison test, considering significance level of 5% (p<0.05). Proportions in the rows followed by the same superscript lower-case letter do not differ statistically from each other by the multiple comparison test, considering significance level of 5% (p<0.05).
NICU, Neonatal Intensive Care Unit; PICU, Pediatric Intensive Care Unit; mixed PICU, mixed Pediatric Intensive Care Unit (with both neonatal and pediatric beds).
ICUs which followed weaning protocols, frequently had physical therapists performing this procedure (66.7%). In units that did not follow protocols, physicians were primarily the clinicians who performed the weaning from MV (54.2%). In the NICUs, either a multiprofessional team or a physical therapist often carried out the MV weaning procedure (66.7%). NICUs were the only units where the decision regarding extubation was the sole responsibility of the physical therapist. In PICUs, a physician with a physical therapist frequently performed the weaning procedure (39.0%) while extubation decisions were primarily made by physicians (40.3%). In mixed PICUs, the MV weaning was mainly performed by physicians, being helped by physical therapists(16%) or alone (16.0%) and the decision to perform extubation were frequently made by physicians (17.9%) (Table 2).
Regarding the time of physical therapists to provide assistance, in most NICUs and mixed PICUs were less than 18h/day (38.9% and 40.9% respectively), whereas assistance provided in PICUs was frequently 24h/7 days per week (56.0%) compared to other services provided (Table 3).
Comparison of the physical therapist's presence in ICU with the other variables analyzed.
| Variables | Are there physical therapists? | Physical therapy h/day | |||
|---|---|---|---|---|---|
| Type of hospital | Dedicated | Not dedicated | 24h/day | 18h/day | <18h/day |
| Public teaching hospital | 85.7aA | 14.3bA | 44.9aA | 18.4bA | 36.7abA |
| Public hospital | 84.2aA | 15.8bA | 45.9aA | 13.5bA | 40.6aA |
| Private hospital | 75.8aA | 24.2bA | 45.4aA | 27.3aA | 27.3aA |
| Philanthropic hospital | 76.0aA | 24.0bA | 32.0aA | 28.0aA | 40.0aA |
| Type of ICU | |||||
| NICU | 84.7aA | 15.3bA | 36.1aA | 25.0aA | 38.9aA |
| PICU | 80.4aA | 19.6bA | 56.0aA | 14.0bA | 30.0bA |
| Mixed PICU | 72.7aA | 27.3bA | 36.4aA | 22.7aA | 40.9aA |
| Use of MV weaning protocol | |||||
| Yes | 86.7aA | 13.3bA | 48.8aA | 21.9bA | 29.3bB |
| No | 75.4aA | 24.6bA | 36.1abA | 18.0bA | 45.9aA |
| Professional who carried out weaning procedures | |||||
| Physician | 54.2aB | 45.8bA | 25.0aA | 25.0aA | 50.0aA |
| Physical therapist | 66.7aAB | 33.3bAB | 33.3aA | 33.3aA | 33.3aA |
| Physician and physical therapist | 88.0aA | 12.0bB | 46.5aA | 20.2bA | 33.3abA |
| Physician and nurse | – | – | – | – | – |
| Multiprofessional team | 83.3aAB | 16.7bAB | 50.0aA | 16.7aA | 33.3aA |
| Professional who decided the extubation procedures | |||||
| Physician | 72.7aA | 27.3bA | 33.3abA | 21.2bA | 45.5aA |
| Physical therapist | 100.0A | – | 100.0A | – | – |
| Physician and physical therapist | 88.7aA | 11.3bA | 51.4aA | 21.4bA | 27.1bA |
| Physician and nurse | – | – | – | – | – |
| Multiprofessional team | 83.3aA | 16.7bA | 33.3aA | 16.7aA | 50.0aA |
| Frequency of extubation attempts | |||||
| Success in the first extubation attempt | – | – | 42.2a | 21.9b | 35.9ab |
Note: Proportions in the columns followed by the same superscript upper-case letter do not differ statistically from each other by the multiple comparison test, considering significance level of 5% (p<0.05). Proportions in the rows followed by the same superscript lower-case letter do not differ statistically from each other by the multiple comparison test, considering significance level of 5% (p<0.05). ICU, Intensive Care Unit; NICU, Neonatal Intensive Care Unit; PICU, Pediatric Intensive Care Unit; mixed PICU, mixed Pediatric Intensive Care Unit (with both neonatal and pediatric beds).
For the professionals performing the weaning procedure or deciding on extubation, it was noted that when weaning were carried out by both physicians and physical therapists, 88% of the ICUs had dedicated physical therapists in the unit. When physicians were carrying out the MV weaning procedure alone, physical therapy assistance was available less than 18h/day (50.0%). In ICUs where physical therapists made a decision on extubation, they were professionals dedicated to that unit who provided coverage in the ICU 24h/7 days per week (Table 3).
DiscussionThis is the first study carried out in Brazil that describes the role and characteristics of the work structure for physical therapists taking part in MV weaning and extubation procedures involving pediatric and neonatal patients. Our findings showed that physical therapists would carry out weaning procedures more often when there were MV weaning protocols on the units. In units in which there were dedicated physical therapists 24h/7 days per week, protocols were commonly used. In this case, the extubation decision was predominantly made by the dedicated physical therapist and the extubation procedure was frequently done successfully in the first attempt. Following the extubation, it is important for the physical therapist to follow-up and monitor the patient to assure airway patency and adequate pulmonary ventilation during this period.22
In the NICUs, MV weaning procedure was frequently performed by physical therapists individually or as part of a multi-professional team, while in the PICUs and mixed PICUs this procedure was performed more often by physician with physical therapist. For the extubation procedure, our findings revealed that it was primarily done by physicians in PICUs and mixed PICUs, and that physical therapists independently deciding to perform extubation only occurred in NICUs following set procedures.
A previous Brazilian survey16 carried out in adult ICUs in the country showed that 79.2% of physical therapists interviewed performed the MV weaning procedure. Nevertheless, only 22% of them independently conducted MV weaning. The profile of professional responsibility when making decisions on these procedures varies among countries, however, the establishment of a protocol is often shared by the health professional team.23 That being said, the ultimate decision lies with the physician whose patient is being treated. Involving a team of professionals may avoid delayed identification of when to start the weaning procedure and makes use of other clinicians skills in performing extubation, as well as unnecessary extension of MV.23 Moreover, having a health professional other than the patient's physician decide on MV weaning and extubation procedures may be influenced not only by the existence of MV and weaning protocols,23 but also the availability and involvement of the multiprofessional team of each ICU, in this process.
In pediatrics, decisions to start the MV weaning procedure is usually in the hands of ICU physicians after the assessment of clinical and functional criteria which determine the possibility of a successful weaning procedure.4,24 Previous surveys have shown that the use of MV weaning protocols in NICUs25 and PICUs6,26 are rarely used and have controversial results.8,27 On the other hand, another survey conducted in Canada, described that MV protocols were commonly used in units where there were dedicated physical therapists,10 especially in units where this professional service was available 24h/7 days per week.11 Protocols are useful to standardize MV procedures in ICUs, since they offer opportunities to engage a multi-professional team and encourage actions to be taken when facing doubt about when to initiate the MV weaning procedure.10,11
The results of the current survey showed the predominant use of protocols occurred in private hospitals. Previous studies have shown controversial results regarding the application of MV protocols in different types of hospitals.10,11 Furthermore, it is important to note that physical therapy assistance provided 24h/7 days per week was predominant in ICUs in public teaching hospitals, although a study carried out by Costa et al.,28 showed that physical therapists worked mainly in the private sector (60%) in different levels of health care.
It is important to note that, although the response rate was 48.9%, this survey included all the states of the country and was above the minimal sample required (82 units) to be representative of the total number of ICUs in Brazil. Similar surveys in Brazil actually have achieved lower response rates.29
This survey was important to understand the profile of physical therapists in different types of ICUs with regards to MV weaning and extubation procedures. Furthermore, it was significant to identify the professionals’ working conditions that might impact how these procedures are performed. Finally, it is meaningful to highlight the participation of physical therapists in MV weaning and extubation procedures as well as the involvement of different team members who work in the ICU. Future studies will be needed to assess the impact of physical therapy assistance 24h/7 days per week on the MV weaning process outcomes.
Conflicts of interestThe authors declare no conflicts of interest.
We thank the Associação de Medicina Intensiva Brasileira (AMIB/AMIBnet) and the Departamento de Fisioterapia em Terapia Intensiva (DEFITI-AMIB) for their support and promotion of the research. We are also grateful to the professionals of the Intensive Care Units and Professor Debora Feijó Villas Boas that contributed to the research.