Functional limitation is relatively common and can negatively influence the postoperative outcome of patients after cardiac surgery.
ObjectiveTo identify the predictive factors of functional limitation in patients undergoing elective cardiac surgery.
MethodsRetrospective cohort study was performed to evaluate patients undergoing elective cardiac surgery. All patients underwent a cardiovascular rehabilitation protocol. Functional limitation was defined based on performance in the rehabilitation protocol following cardiac surgery. Poor performance in the cardiac surgery rehabilitation protocol defined functional limitation, whereas good performance indicated no limitation.
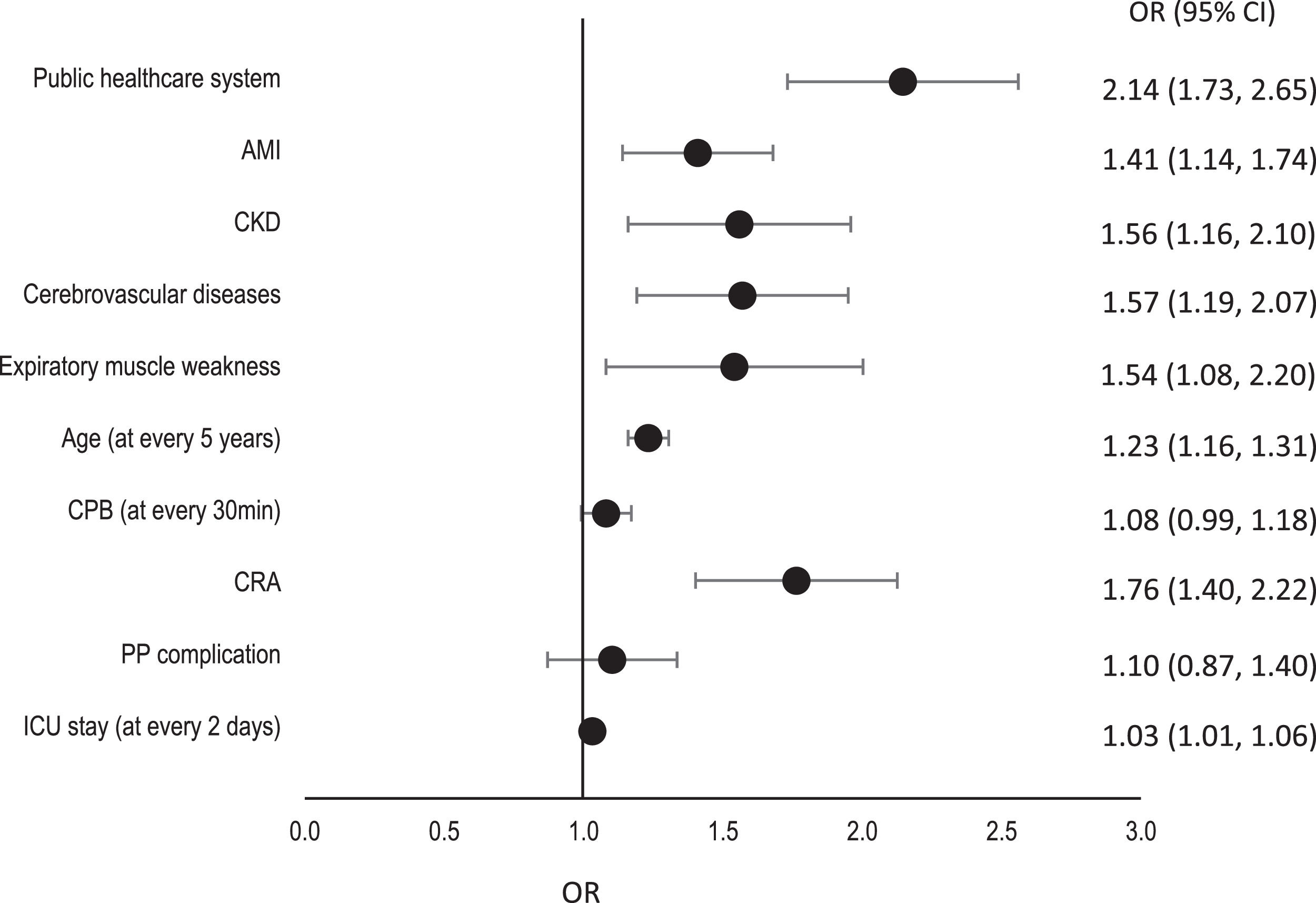
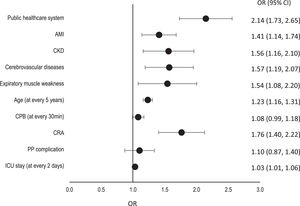
ResultsData were collected from 548 patients; of these, 190 (34.7%) had functional limitation. In multivariate analysis, the factors associated with postoperative functional limitation were as follows: hospitalization by the public healthcare system [OR: 2.14; 95% confidence interval (CI): 1.73, 2.65]; age (OR 1.23; 95% CI: 1.15, 1.31); length of hospitalization in the intensive care unit (OR 1.03; 95% CI: 1.01, 1.05); history of previous acute myocardial infarction (OR 1.40; 95% CI: 1.13, 1.73); presence of previous comorbidities [chronic kidney disease (OR 1.56; 95% CI: 1.15, 2.10); cerebrovascular disease (OR 1.57; 95% CI: 1.19, 2.07)]; presence of expiratory muscle weakness (OR 1.54; 95% CI: 1.08, 2.20); and intercurrence of cardiorespiratory arrest during hospitalization (OR 1.76; 95% CI: 1.40, 2.22).
ConclusionFunctional limitation after cardiac surgery could be predicted by multiple pre and postoperative factors, except for preoperative functionality, which does not suggest to be an independent factor for functional limitation after surgery.
Cardiovascular diseases are among the most prevalent illnesses, and often require surgical procedures.1 However, because these procedures are highly complex, complications in the perioperative period are frequent and may increase functional limitation in the postoperative period. Functional limitation after cardiac surgery often results in increased dependency and decreased autonomy and quality of life, and these outcomes can be associated with a worse prognosis.2-5
There are several risk factors for functional limitation, some of which have already been identified, such as age, preoperative frailty, previous comorbidities, and postoperative complications resulting in increased length of hospital stay.4-8 Functional limitation is a subject that currently receives limited attention in research, and the existing studies are composed of succinct assessments or evaluate the preoperative, intraoperative, and postoperative periods separately. This hinders obtaining an overview of all phases involved in cardiac surgery and can potentially influence the outcomes.
Therefore, functional limitation is an increasingly discussed topic, and identifying predictive factors is an important step to assist in future decision-making, especially when dealing with modifiable factors that could benefit from preventive actions. This study aims to identify the preoperative, intraoperative, and postoperative predictive factors of functional limitation at the hospital discharge in patients undergoing elective cardiac surgery.
MethodsDesign and populationThis is a retrospective cohort study. Patients who underwent elective cardiac surgery at the Hospital São Francisco were retrospectively analyzed. The hospital belongs to the Irmandade Santa Casa de Misericórdia de Porto Alegre (ISCMPA), a tertiary care university hospital specializing in the treatment of cardiovascular diseases. The data were collected retrospectively from the physical therapy service database and electronic medical records of the hospital. The data were collected from January 2017 to December 2018 (24 months). The sample included data of all patients of both sexes over 18 years of age, who were admitted to São Francisco Hospital and underwent elective cardiac surgery. Patients who died during the surgery and patients who had incomplete medical records were excluded from the analysis. The project was approved by the Research Ethics Committee of the Irmandade Santa Casa de Misericórdia of Porto Alegre, Brazil under protocol number 3.222.604.
Physical therapy care protocolThe study used a specific institutional care protocol with several steps to guide the postoperative rehabilitation of patients. The protocol began after the patient was discharged from the Intensive Care Unit (ICU), at least two days after the surgery, and continued until the patient was discharged from the hospital. The cardiovascular rehabilitation protocol consisted of six steps, where the patients would progress to the next step at each session if they were in good clinical condition, that is, if the patient had hemodynamic and ventilatory stability and was able to complete the stage without any complications. The rehabilitation protocol is detailed in Table 1.
Institutional protocol of physical therapy care in surgical cardiac patients.
ULs, upper limbs; LLs, lower limbs.
The outcome was determined by the last step reached in the protocol completed successfully with good clinical tolerance. The patients were categorized into two groups based on how far they progressed through this protocol during their hospital stay. The functional limitation group was composed of patients who were discharged from the hospital after reaching step 03 of the protocol, indicating limited functional recovery. The group with no functional limitation was composed of patients who reached step 04 or further, indicating better functional recovery.
The outcome choice was based on the intensity and energy expenditure required for climbing up and down stairs, measured using the metabolic equivalent of the task (MET). This metric corresponds to a moderate-intensity activity and differentiates between steps 03 and 04 of the institutional protocol. Further details are available in the online supplementary material.
Outcomes and assessmentsAn electronic medical record of comorbidities, previous clinical history, and findings of complementary exams, such as echocardiography, was described for sample characterization and functional evaluation via frailty criteria (further details are available in the online supplementary material). Frailty was assessed according to the phenotype concept via five domains:
1 - low level of physical activity: assessed using the Duke Activity Status Index. This index consists of a simple 12-item questionnaire that evaluates activities of daily living and provides an estimate of the MET. The higher the score, the greater the functional capacity of the individual. A cutoff point of four METs was used;9,10
2- peripheral muscle weakness: assessed by measuring the strength of the peripheral muscles using a bilateral handgrip with a Saehan SH5001 hand dynamometer, following the positioning guidelines of the American Society of Hand Therapists (ASHT).11 The test was repeated three times at intervals of 1 min between attempts; the result was the mean value of these three measurements. For analysis of the strength assessment results, the predicted values adjusted for sex and body mass index were considered12;
3 - slowness: evaluated through the gait speed test, in which the individual walked at a comfortable speed on a flat surface for a predetermined distance of 5 m.13 The distance and rhythm were kept intentionally short and comfortable, below the cardiopulmonary capabilities, so that the individual reached a constant speed without reaching limits and consequent cardiopulmonary or hemodynamic symptomatology. A walking time of more than 6 s (less than 0.83 m/s) was found to correlate with a three-fold increase in mortality or severe morbidity after cardiac surgery. Therefore, a duration of 6 s was set as the cutoff point in this study14;
4 - self-reported fatigue: assessed by asking the patients the following adapted question from the depression scale of the Center for Epidemiological Studies (CES-D): "How many days in the last week did you feel like all you have done was strenuous?" The result was considered abnormal if the patient complained of strenuous effort for more than three days13;
5 - weight loss: assessed based on serum albumin levels and through an objective question: “Did the patient report unintentional weight loss (not due to dieting or exercise) in the last year?” The result was considered abnormal if the patient had a weight loss of ≥4.5 kg in the previous year and if the serum albumin level was ≤ 3.3 g/dL.12,13
Although not encompassing the phenotype of fragility, respiratory muscle strength has been extensively studied to identify the presence of respiratory muscle weakness because it interferes with ventilatory mechanics and can limit the rehabilitation of patients after cardiac surgery.15 Respiratory muscle strength production capacity was validated through the measurement of maximum inspiratory pressure (MIP) and maximum expiratory pressure (MEP) using a digital manovacuometer Globalmed® MVD300.16 The patient was positioned in a sitting position in an armchair or chair with the trunk and upper limbs supported. The test was repeated three times at one-minute intervals, and the highest value was considered, as long as the difference between the two highest values was ≤ 10%. If the variability measurement was greater than 10%, the data were disregarded, and a new measurement was performed until all the measurements had less than 10% variability. Absolute and percentage values predicted by Neder equations (predictive equations for static respiratory pressures in a randomized sample of Brazilian adults) were considered in the analysis of these results.17
These variables were collected to demonstrate the patient's functional status before cardiac surgery, and frailty syndrome has been strongly associated with higher postoperative morbidity and mortality. Additionally, respiratory muscle strength can directly interfere with the postoperative outcome.
Intraoperative data were collected from electronic medical records, including the type of surgical procedure, cardiopulmonary bypass time, cross-clamp time (XCT), the need for blood derivative transfusion, and the development of total atrioventricular block (AVB).
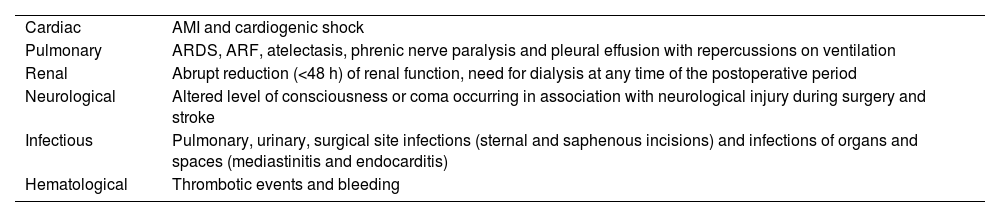
Finally, the following postoperative data were collected: length of hospitalization in the ICU, the occurrence of cardiorespiratory arrest (CRA) during hospitalization, and development of postoperative complications, including cardiac, pulmonary, renal, neurological, infectious, hematological, and other complications (Table 2). These complications were considered within 48 h of the postoperative period.
Postoperative complications after cardiac surgery.
AMI, acute myocardial infarction; ARDS, acute respiratory distress syndrome; ARF, acute respiratory failure.
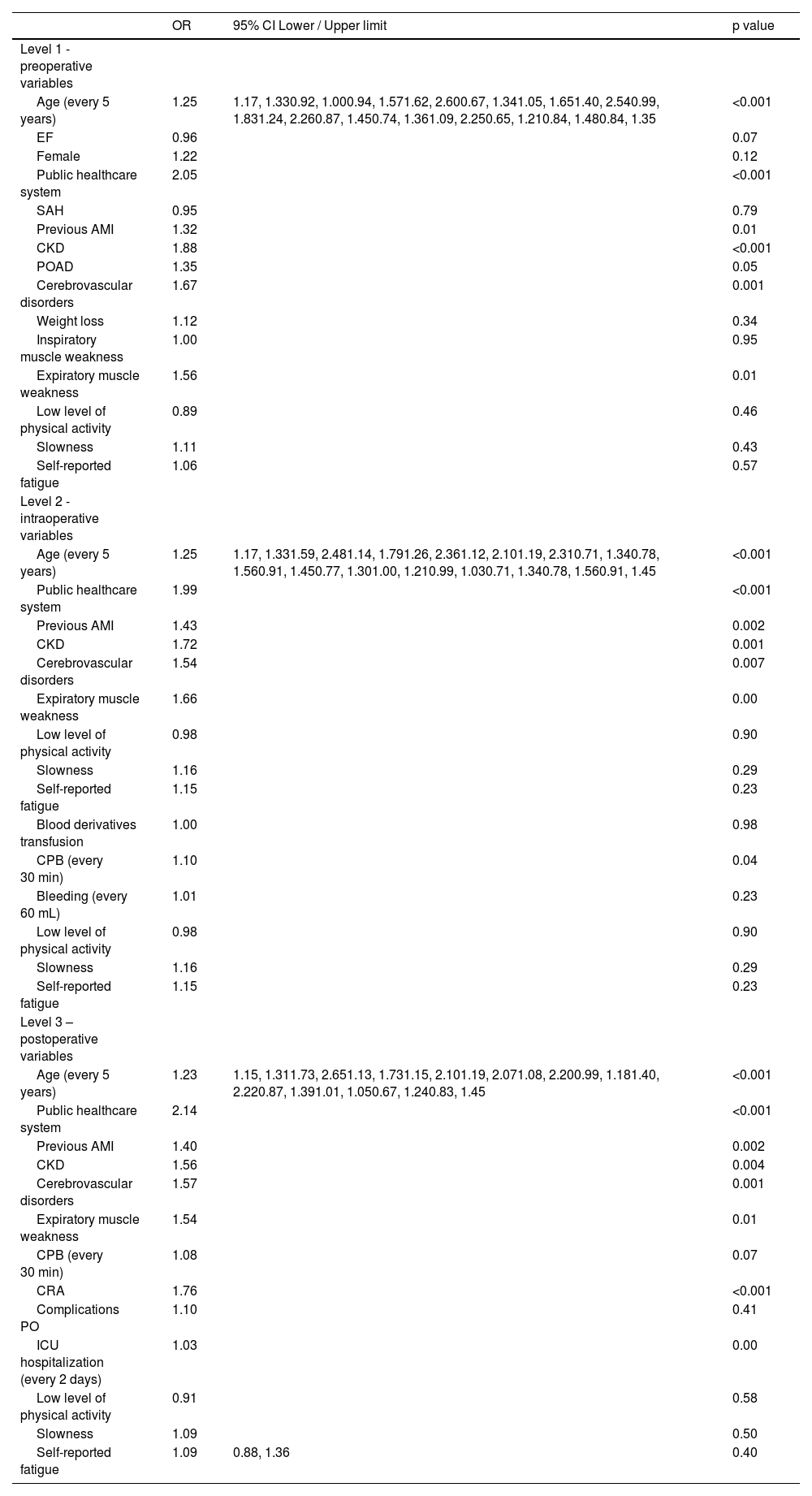
The results were presented via descriptive statistics: frequency and percentage, mean and standard deviation (SD), and median and interquartile interval, depending on the nature and distribution of the variables. The normality of data was checked using the Kolmogorov-Smirnov test. Univariate analysis was performed using a chi-square test for categorical variables, Student's t-test for quantitative variables with symmetrical distribution, and Mann-Whitney U test for quantitative variables with asymmetric distribution. Variables with p-values less than 0.20 were subjected to multivariate analysis using a hierarchical model. The hierarchical model consisted of preoperative variables in level 1, intraoperative variables in level 2, and postoperative variables in level 3. Poisson's regression with robust variance was used for the analysis, and prevalence odds ratios (OR) with a 95% confidence interval (CI) were calculated. The variables of slowness, self-reported fatigue, and low level of physical activity were included for subsequent level control, as they demonstrated the patient's functional status before cardiac surgery. A p-value of less than 0.05 was considered statistically significant, and the analyses were performed using SPSS 25.0 software.
ResultsOf 718 cardiac surgeries performed during the study period, 170 patients (19.7%) were excluded from the analysis: 28 due to intraoperative death and 142 due to data loss (see Table 1 in the online supplementary material). Data were collected from 548 patients who underwent elective cardiac surgery. Of these, 190 patients (34.7%) had functional limitations according to the institution's physical therapy protocol. The mean age of the sample was 63.8 years (SD=10.7). Male patients predominated in the overall sample (n = 383, 69.9%), with a mean body mass index (BMI) of 27.7 kg/m² (SD=4.5).
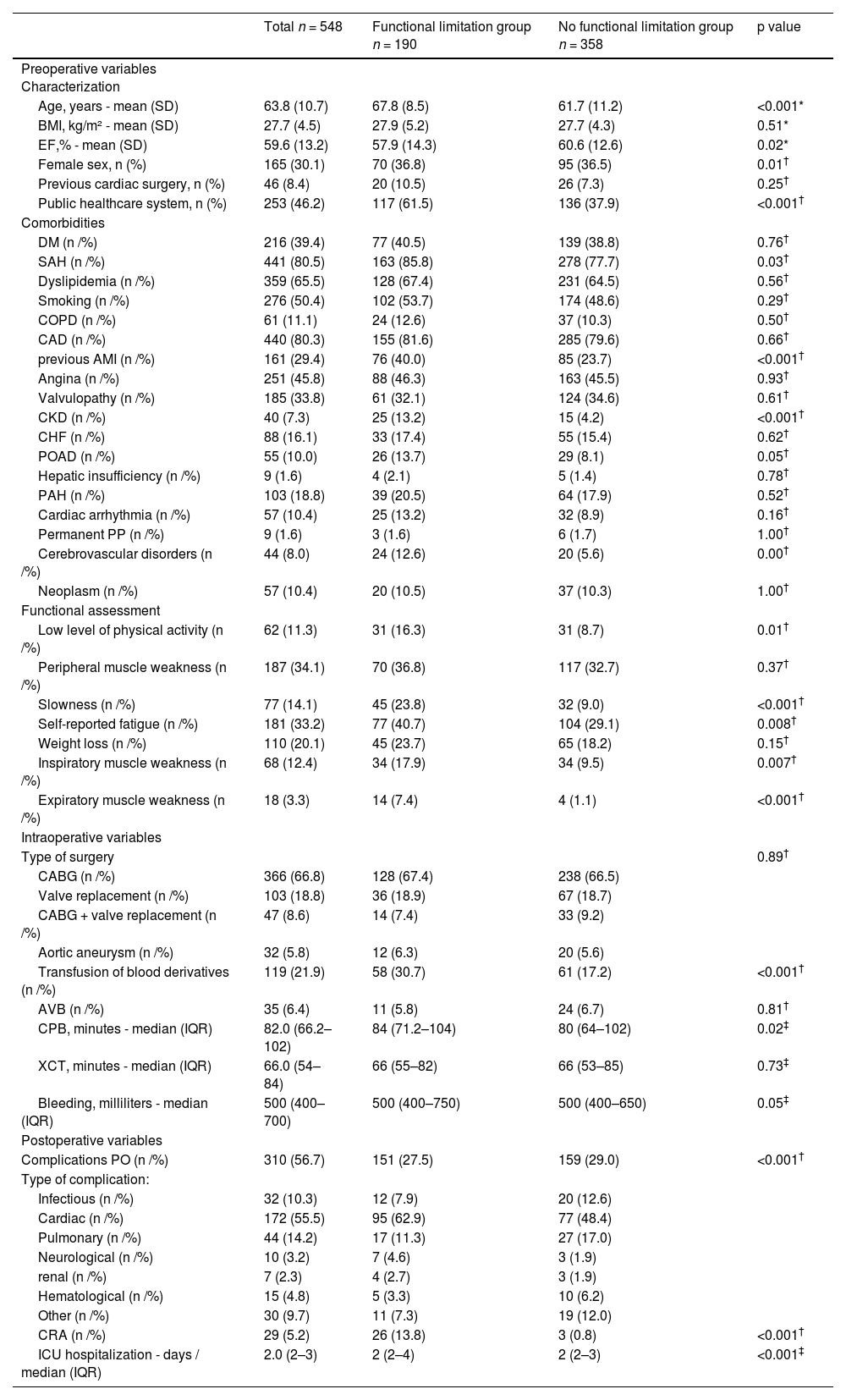
In the univariate analysis, patients with functional limitations were older on average and had a lower ejection fraction. Most females, hospitalized through the public healthcare system (Brazilian Unified Health System, SUS), had more associated diseases, and performed worse in the preoperative functional evaluation. Additionally, this group had longer cardiopulmonary bypass (CPB) times, experienced more bleeding and a higher frequency of blood derivative transfusions, more postoperative complications, more frequent cardiorespiratory arrest (CRA), and longer ICU hospitalization times (Table 3).
Univariate analysis of preoperative, intraoperative, and postoperative variables for risk of functional limitation after cardiac surgery.
| Total n = 548 | Functional limitation group n = 190 | No functional limitation group n = 358 | p value | |
|---|---|---|---|---|
| Preoperative variables Characterization | ||||
| Age, years - mean (SD) | 63.8 (10.7) | 67.8 (8.5) | 61.7 (11.2) | <0.001* |
| BMI, kg/m² - mean (SD) | 27.7 (4.5) | 27.9 (5.2) | 27.7 (4.3) | 0.51* |
| EF,% - mean (SD) | 59.6 (13.2) | 57.9 (14.3) | 60.6 (12.6) | 0.02* |
| Female sex, n (%) | 165 (30.1) | 70 (36.8) | 95 (36.5) | 0.01† |
| Previous cardiac surgery, n (%) | 46 (8.4) | 20 (10.5) | 26 (7.3) | 0.25† |
| Public healthcare system, n (%) | 253 (46.2) | 117 (61.5) | 136 (37.9) | <0.001† |
| Comorbidities | ||||
| DM (n /%) | 216 (39.4) | 77 (40.5) | 139 (38.8) | 0.76† |
| SAH (n /%) | 441 (80.5) | 163 (85.8) | 278 (77.7) | 0.03† |
| Dyslipidemia (n /%) | 359 (65.5) | 128 (67.4) | 231 (64.5) | 0.56† |
| Smoking (n /%) | 276 (50.4) | 102 (53.7) | 174 (48.6) | 0.29† |
| COPD (n /%) | 61 (11.1) | 24 (12.6) | 37 (10.3) | 0.50† |
| CAD (n /%) | 440 (80.3) | 155 (81.6) | 285 (79.6) | 0.66† |
| previous AMI (n /%) | 161 (29.4) | 76 (40.0) | 85 (23.7) | <0.001† |
| Angina (n /%) | 251 (45.8) | 88 (46.3) | 163 (45.5) | 0.93† |
| Valvulopathy (n /%) | 185 (33.8) | 61 (32.1) | 124 (34.6) | 0.61† |
| CKD (n /%) | 40 (7.3) | 25 (13.2) | 15 (4.2) | <0.001† |
| CHF (n /%) | 88 (16.1) | 33 (17.4) | 55 (15.4) | 0.62† |
| POAD (n /%) | 55 (10.0) | 26 (13.7) | 29 (8.1) | 0.05† |
| Hepatic insufficiency (n /%) | 9 (1.6) | 4 (2.1) | 5 (1.4) | 0.78† |
| PAH (n /%) | 103 (18.8) | 39 (20.5) | 64 (17.9) | 0.52† |
| Cardiac arrhythmia (n /%) | 57 (10.4) | 25 (13.2) | 32 (8.9) | 0.16† |
| Permanent PP (n /%) | 9 (1.6) | 3 (1.6) | 6 (1.7) | 1.00† |
| Cerebrovascular disorders (n /%) | 44 (8.0) | 24 (12.6) | 20 (5.6) | 0.00† |
| Neoplasm (n /%) | 57 (10.4) | 20 (10.5) | 37 (10.3) | 1.00† |
| Functional assessment | ||||
| Low level of physical activity (n /%) | 62 (11.3) | 31 (16.3) | 31 (8.7) | 0.01† |
| Peripheral muscle weakness (n /%) | 187 (34.1) | 70 (36.8) | 117 (32.7) | 0.37† |
| Slowness (n /%) | 77 (14.1) | 45 (23.8) | 32 (9.0) | <0.001† |
| Self-reported fatigue (n /%) | 181 (33.2) | 77 (40.7) | 104 (29.1) | 0.008† |
| Weight loss (n /%) | 110 (20.1) | 45 (23.7) | 65 (18.2) | 0.15† |
| Inspiratory muscle weakness (n /%) | 68 (12.4) | 34 (17.9) | 34 (9.5) | 0.007† |
| Expiratory muscle weakness (n /%) | 18 (3.3) | 14 (7.4) | 4 (1.1) | <0.001† |
| Intraoperative variables | ||||
| Type of surgery | 0.89† | |||
| CABG (n /%) | 366 (66.8) | 128 (67.4) | 238 (66.5) | |
| Valve replacement (n /%) | 103 (18.8) | 36 (18.9) | 67 (18.7) | |
| CABG + valve replacement (n /%) | 47 (8.6) | 14 (7.4) | 33 (9.2) | |
| Aortic aneurysm (n /%) | 32 (5.8) | 12 (6.3) | 20 (5.6) | |
| Transfusion of blood derivatives (n /%) | 119 (21.9) | 58 (30.7) | 61 (17.2) | <0.001† |
| AVB (n /%) | 35 (6.4) | 11 (5.8) | 24 (6.7) | 0.81† |
| CPB, minutes - median (IQR) | 82.0 (66.2–102) | 84 (71.2–104) | 80 (64–102) | 0.02‡ |
| XCT, minutes - median (IQR) | 66.0 (54–84) | 66 (55–82) | 66 (53–85) | 0.73‡ |
| Bleeding, milliliters - median (IQR) | 500 (400–700) | 500 (400–750) | 500 (400–650) | 0.05‡ |
| Postoperative variables | ||||
| Complications PO (n /%) | 310 (56.7) | 151 (27.5) | 159 (29.0) | <0.001† |
| Type of complication: | ||||
| Infectious (n /%) | 32 (10.3) | 12 (7.9) | 20 (12.6) | |
| Cardiac (n /%) | 172 (55.5) | 95 (62.9) | 77 (48.4) | |
| Pulmonary (n /%) | 44 (14.2) | 17 (11.3) | 27 (17.0) | |
| Neurological (n /%) | 10 (3.2) | 7 (4.6) | 3 (1.9) | |
| renal (n /%) | 7 (2.3) | 4 (2.7) | 3 (1.9) | |
| Hematological (n /%) | 15 (4.8) | 5 (3.3) | 10 (6.2) | |
| Other (n /%) | 30 (9.7) | 11 (7.3) | 19 (12.0) | |
| CRA (n /%) | 29 (5.2) | 26 (13.8) | 3 (0.8) | <0.001† |
| ICU hospitalization - days / median (IQR) | 2.0 (2–3) | 2 (2–4) | 2 (2–3) | <0.001‡ |
AMI, acute myocardial infarction; AVB, total atrioventricular block; BMI, body mass index; CABG, coronary artery bypass grafting; CAD, coronary artery disease; CHF, congestive heart failure; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; CPB, cardiopulmonary bypass; CRA, cardiorespiratory arrest; DM, diabetes mellitus; EF, ejection fraction; ICU, Intensive care unit; PAH, pulmonary arterial hypertension; PO, postoperative; POAD, peripheral occlusive arterial disease; PP, permanent pacemaker; SAH, systemic arterial hypertension; XCT, cross clamp time.
The multivariate analysis revealed that several variables increased the risk of a worse functional outcome, including patients hospitalized through the public healthcare system, older age, longer ICU hospitalization time, history of previous acute myocardial infarction (AMI), chronic kidney disease (CKD), cerebrovascular disease, expiratory muscle weakness, and CRA during hospitalization (Table 4).
Hierarchical model of multivariate analysis of preoperative, intraoperative, and postoperative risk factors for functional limitation after cardiac surgery.
AMI, acute myocardial infarction; CKD, chronic kidney disease; CPB, cardiopulmonary bypass; CRA, cardiorespiratory arrest; EF, ejection fraction; ICU, intensive care unit; SAH, systemic arterial hypertension; PO, postoperative period; POAD, peripheral occlusive arterial disease.
Specifically, the following factors were associated with a higher risk of functional limitation: (1) Patients who were hospitalized through the public healthcare system had a risk of functional limitation twice as high as patients who were not hospitalized through the public healthcare system (OR 2.14; 95% CI: 1.73, 2.65). (2) Age was associated with an increased risk of 23% for every 5 years of life (OR 1.23; 95% CI: 1.16, 1.31). (3) Every two days of ICU hospitalization increased the risk of functional limitation by 3% (OR 1.03; 95% CI: 1.01, 1.06). (4) Regarding comorbidities, patients with a history of AMI had a functional limitation risk of 41% (OR 1.41; 95% CI: 1.14, 1.74), those with CKD had a functional limitation risk of 56% (OR 1.56; 95% CI: 1.16, 2.10), and those with previous cerebrovascular disease had a functional limitation risk of 57% (OR 1.57; 95% CI: 1.19, 2.07). (5) The presence of expiratory muscle weakness increased the risk of functional limitation by 54% (OR 1.54; 95% CI: 1.08, 2.20). 6) CRA during hospitalization increased the risk of a worse functional outcome by 76% (OR 1.76; 95% CI: 1.40, 2.22) compared to those who did not experience this complication (Fig. 1).
Graphical representation of the multivariate analysis of preoperative, intraoperative, and postoperative risk factors for functional limitation after cardiac surgery. Patients were categorized into two groups: functional limitation group (discharged from the hospital after reaching up to step 3 of the protocol) and not functional limitation group (reached step 4 or further of the institutional protocol).
AMI, acute myocardial infarction; CKD, chronic kidney disease; CPB, cardiopulmonary bypass; CRA, cardiorespiratory arrest; PP, postoperative period; ICU, intensive care unit.
This study demonstrated that hospitalization through the public healthcare system, age, ICU length of stay, history of AMI, CKD, previous cerebrovascular disease, expiratory muscle weakness, and CRA during hospitalization are independent factors for functional limitation after elective cardiac surgery. Cardiac surgeries are frequent worldwide, and multiple studies confirmed factors related to postoperative morbidity and mortality.18-30 However, there is a clear need for studies on functional limitation, because studies evaluating cardiac surgery outcomes have traditionally focused on mortality.
Functional limitation is relatively common after cardiac surgery. In a prospective and multicenter cohort study, Hoogerduijn et al.8 observed that approximately 16% of all participants had functional limitation after cardiac surgery.8 In existing studies that have evaluated the conditions associated with functional limitation in the postoperative period of cardiac surgery (POCS), certain risk factors have already been established, such as age, length of hospitalization, and previous comorbidities as kidney failure.4-8 These studies support our findings and suggest that these factors play an important role in functional limitation after cardiac surgery. However, to date, no study has observed the relationship between the presence of AMI and cerebrovascular disease prior to the surgical procedure.
The present study also revealed the association of hospitalization through the public healthcare system with functional limitation in the POCS. The current findings showed that patients hospitalized through the public healthcare system presented greater functional limitation in the POCS than those with private health insurance. At the hospital where the study was conducted, patients receive assistance through the public or private health care system. This is a characteristic of the Brazilian health care system, where most private hospitals also encompass and serve the public health system. According to Andersen et al., the lack of private health insurance was associated with higher morbidity and mortality in aortic surgeries.31 This finding agrees with the results of Tumin et al., which showed that the transition from private health insurance to the public healthcare system after heart transplantation was associated with worse long-term outcomes, directly interfering with survival after transplantation.32
In Brazil, the demand for patients requiring cardiac surgery generally exceeds the availability of hospital resources. According to data from the National Council of Medicine, the waiting list for elective surgical procedures in the Brazilian Unified Health System in 2022 exceeded 1.000.000 held back procedures.33 This increased waiting time may be associated with the deficient infrastructure of the Unified Health System, which may be directly linked to the patient's clinical deterioration due to the worsening of their condition while waiting for the surgical procedure, and consequently be associated with worse outcomes. Moreover, the difference in demand for care between patients with and without health insurance should be considered, where patients assisted by private health insurance probably receive greater preoperative and postoperative care due to the demand and costs related to hospital resources.
Another finding of this study was the association between expiratory muscle weakness and functional limitation in the POCS. It is known that expiratory muscle strength is directly linked to cough strength in the POCS and thus with the ability to generate sufficient pulmonary volumes to protect the airway and prevent postoperative pulmonary complications, which can directly interfere with the postoperative outcome.13 In a study involving 117 patients undergoing elective CABG, Hulzebos et al.34 observed that expiratory muscle strength of ≥75% of the predicted value was a protective factor against postoperative pulmonary complications.34 Therefore, expiratory muscle weakness, which can be easily assessed in the preoperative period, can provide important information on surgical prognosis.
The present study found an association between cardiac arrest (CRA) during hospitalization and functional limitation after cardiac surgery (POCS). CRA is a severe adverse event that can have various causes and lead to different complications degrees. It is noteworthy that the result found in this study includes both intraoperative and postoperative complications related to CRA, although it should be differentiated from the intentional cardiac arrest induced by cardioplegia, often necessary for the surgical procedure. Numerous studies have highlighted the safety and significance of physical therapy in preventing or reducing postoperative complications and its potential to enhance clinical outcomes for patients.35-37 It is also known that more effective recovery is associated with the implementation of a structured protocol for early mobilization and comprehensive exercises for the upper and lower limbs.37-39 Therefore, this type of protocol was used in this study.
Unlike the expected result, the functionality assessed preoperatively through the frailty phenotype had no impact on the outcome, and only expiratory muscle weakness was associated with the outcome studied. There is no explanation for these findings, as the frailty syndrome has previously been strongly associated with increased postoperative morbidity and mortality.23 One hypothesis is that it reflects the profile of patients who are eligible for elective heart surgery since their heart disease is stabilized, and the management of associated diseases is optimized, which prevents exacerbations and complications. More severe patients, who probably have had worse functionality in the preoperative period, may not have been included in the sample because they were considered unfit for surgery or died during surgery. Therefore, probably expiratory muscle weakness may be a complementary factor to the preoperative functional evaluation in predicting the outcome of the study.
Almost all the functionality variables assessed in the preoperative period showed a statistically significant difference in the univariate analysis, including a low level of physical activity, slowness, self-reported fatigue, weight loss, and inspiratory weakness. However, this statistical difference was not maintained in the multivariate analysis. A possible explanation for this result is that these factors may have influenced another variable that showed a significant difference in the multivariate analysis, such as age, but individually they lost their statistical power.
The findings of this study could potentially provide valuable insights for future decision-making, particularly regarding modifiable factors such as expiratory muscle weakness that can be addressed in the preoperative period. Additionally, this study may have identified weaknesses in the routines of a large healthcare service, with high rates of cardiac arrest, cardiopulmonary bypass use, and prolonged ICU stays. These findings may suggest that improvements could be achieved to the organization of care during the perioperative period to mitigate these adverse outcomes.
Regarding the strengths of the study, firstly, it associates functional limitation with a comprehensive functional evaluation, along with other preoperative, intraoperative, and postoperative factors, using a standardized postoperative rehabilitation protocol. The authors have provided a detailed clinical picture of patients undergoing cardiac surgery, contrary to previous studies that evaluated each period in isolation or with less detail.4-8 Another strength of the study is that the functional status of the patient was controlled in the preoperative period through data such as slowness, self-reported fatigue, and level of physical activity. These data provide insight into the patient's functionality prior to the surgery. Thus, the results indicate the factors that are related to functional limitation caused by the stress of cardiac surgery itself.
Considering the limitations of the study, as it is a retrospective study, potential biases; and limitations of this type of study should be considered, because the medical records may be incomplete or inaccurate. Sample loss of 19.7% is a limitation, primarily attributed to the loss of data from the preoperative evaluation, which was recently implemented in the institution. Sample size calculation was not performed, as all available patients were included in the study, so there is a possibility of type II error. The statistical model used may not have been the most appropriate, because the intraoperative variables may have been underestimated as they were not associated with the outcome studied, contrary to data from the literature. Conducting the study at a single private center limits the generalizability of the results.
ConclusionFunctional limitation after cardiac surgery could be predicted by multiple preoperative and postoperative factors, except for preoperative functionality, which does not suggest to be an independent factor for functional limitation.