No study to our knowledge has explored physical therapy utilization following lumbar spine surgery in a workers’ compensation setting.
ObjectivesDescribe physical therapy utilization and costs, and return-to-work status in patients following lumbar spine surgery under a workers’ compensation claim.
MethodsUsing data from the New South Wales (NSW) State Insurance Regulatory Authority (Australia), we audited physical therapy billing codes for patients who received lumbar spine surgery from 2010 to 2017. We summarised, by fusion versus decompression, the number of physical therapy sessions patients received up to 12 months post-operatively, total cost of physical therapy and time to initiation of physical therapy. Number of physical therapy sessions and physical therapy utilization at 12 months were summarised by return-to-work status at 12 months.
ResultsWe included 3524 patients (1220 had fusion; 2304 decompression). On average, patients received 22 ± 22 physical therapy sessions to 12 months post-operatively (mean cost=AU$1902, US$1217); 24% were receiving physical therapy at 12 months. Most had 9–24 (31%) or 25–50 sessions (25%); 11% had > 50 sessions, whereas 11% had no physical therapy. Patients who had fusion (compared to decompression) had more physical therapy and incurred higher physical therapy costs. Time post-surgery to initiate physical therapy increased from 2010 to 2017. Patients with > 50 sessions and still having physical therapy by 12 months were least likely to be working.
ConclusionsFor most patients, physical therapy utilization following lumbar spine surgery aligns with the best available evidence. However, some patients may be receiving too much physical therapy or initiating physical therapy too early.
The efficacy of lumbar spine surgery (including fusion and decompression) remains unknown as to our knowledge there are no published placebo-controlled trials,1,2 but rates of surgery are rising. In Australia, there was an increase in the annual rates of fusion (1.3–8 per 100,000) and decompression (19.0–22.1 per 100,000) from 2003 to 2013.3 In the United States, there was a 2.8–3.0-fold increase in the annual rates of fusion from 2000 to 2009.4
In terms of rehabilitation following lumbar spine surgery, low- to very low-certainty evidence (Cochrane review, 5 trials, n = 272 participants) suggests there are small, short-term benefits of exercise therapy if it commences 4–6 weeks following lumbar disk surgery (e.g. standard discectomy, microdiscectomy) and involves 8–24 sessions.5 Rehabilitation that starts before four weeks post-operatively appears to have little to no beneficial effect.5,6
Post-operative physical therapy appears widely utilized following lumbar spine surgery but there is variation in how much physical therapy is provided. A survey of 86 spine surgeons in the Netherlands found most spine surgeons always refer to physical therapy following lumbar disk surgery (65%) and nearly half believe post-operative physical therapy is essential (45%).7 A survey of 51 spine surgeons in the United Kingdom found nearly half (45%) refer their patients to physical therapy following lumbar spine surgery and these patients typically receive 3–6 physical therapy sessions.8 A survey of hospital physical therapy departments in the United Kingdom (n = 69 departments)9 found nearly 50% commenced patient rehabilitation within 0–4 weeks following lumbar discectomy (contrary to the best available evidence.)5 The study also found that 63% of patients receive 5–10 physical therapy sessions before discharge, while 12% receive more than 10 sessions.
No study to our knowledge has investigated variation in the number of physical therapy sessions patients receive following lumbar spine surgery in a workers’ compensation setting, or in Australia. Filling this evidence gap will provide information on how patients in this setting are managed, facilitating comparison to other healthcare settings as well as stimulating dialog about appropriate care pathways. It could also give insight into whether patients are receiving appropriate care according to the best available evidence. Determining the number and timing of physical therapy sessions received following lumbar spine surgery will help us understand whether some patients are receiving excessive, insufficient, or timely care following surgery. This has implications for potential implementation strategies to improve the quality and value of physical therapy in this setting.
The primary aim of this study was to describe the number of physical therapy sessions patients in a worker's compensation cohort receive in the 12 months following lumbar spine surgery, stratified by type of surgery (lumbar fusion versus lumbar decompression). The secondary aims were to:
- i.
Describe the number of physical therapy sessions patients receive up to 12 months post-operatively and cost of this physical therapy, by year (2010–2017).
- ii.
Describe the time to initiation of post-operative physical therapy and the percentage of patients who commence post-operative physical therapy at different time points, by year (2010–2017).
- iii.
Describe the number of physical therapy sessions (continuous variable) and physical therapy utilization at 12 months post-operatively (dichotomous variable) by return-to-work status.
The New South Wales (NSW) Workers’ Compensation system is the largest defined benefit system in Australia, is regulated by the State Insurance Regulatory Authority (SIRA), and compensates people who submit a claim for a work-place injury. Insurers are required to provide SIRA with data on claimant characteristics (e.g. age, sex, occupation, injury details) and health service provided (e.g. physical therapy, orthopedic surgery). Ethics approval was granted by the Research Ethics Office of the South Western Sydney Local Health District (HREC/16/LPOOL/189). As all data were administrative and de-identified, no individual consent was required.
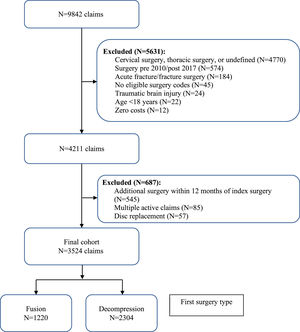
Design and participantsUsing data collected by SIRA we conducted a retrospective cohort study of people who had undergone elective lumbar spine surgery (fusion and/or decompression) funded by NSW Workers’ Compensation between 2010 and 2017. Fusion involves fusing two or more vertebrae together typically with bone grafts, screws, and rods. Decompression involves removing a section of bone from a vertebra or removing a section of damaged intervertebral disk to reduce nerve compression. Fusion was performed with or without decompression. Decompression was performed in isolation. We used data linkage to capture all physical therapy billing codes within one year of surgery. We excluded people who were < 18 years old at the time of surgery, or who had cervical or thoracic surgery, disk replacement surgery (due to a small number of cases), additional spine surgery in the 12 months following their index surgery, less than 12 months of follow-up following surgery, surgery due to fracture or dislocation, a traumatic brain injury, more than one active workers’ compensation claim, no eligible surgery codes, and missing cost data.
Physical therapy utilization, costs, and return-to-work statusWe identified whether a patient had received any physical therapy (or none) as well as the number of physical therapy sessions patients received pre-operatively and up to 12 months post-operatively using physical therapy billing codes. Billing codes from SIRA covered treatment provided in the clinic (e.g. initial consultation, standard consultation, complex treatment, group/class intervention), treatment provided in patients’ home, and other activities (e.g. case conference, report writing, activity assessment) (Supplementary File Table 1). The number of physical therapy sessions patients received to 12 months was categorised as: ‘0 sessions’, ‘1–8 sessions’, ‘9–24 sessions’, ‘25–50 sessions’ and ‘> 50 sessions’. NSW Workers’ Compensation approve physical therapy sessions in blocks of eight and the Cochrane review of rehabilitation following lumbar spine surgery suggests effective rehabilitation programs typically involve 8–24 sessions.5 Physical therapy utilization at 12 months was defined as ‘yes’ versus ‘no’: where ‘yes’ indicated patients who had at least one physical therapy session during the 12th month following surgery. We calculated time from date of surgery to initiation of post-operative physical therapy and categorized it as ‘0–4 weeks’, ‘>4–6 weeks’, and ‘>6 weeks’, based on evidence that suggests rehabilitation following lumbar spine surgery should start 4–6 weeks post-operatively.5 Cost of physical therapy per claim (Australian Dollars, AU$) was calculated by summing the cost of each eligible physical therapy session provided to that patient from the date of surgery to 12 months post-operatively. Due to inflation, we converted all costs to the same reference year (2017) using consumer price indices.10,11 Consumer price indices were obtained from the Australian Taxation Office, using values from the quarter ending on the 31st December.12 To facilitate interpretation internationally, costs reported in the body of this paper were also reported as United States Dollar (US$) using purchasing power parities in 2017 from The World Bank.13 Return-to-work status at 12 months post-operatively was defined as ‘working at full or limited capacity’, ‘not working’, or ‘retired or deceased’.
Statistical analysisWe used means ± standard deviations (SDs), means (range), and medians [interquartile range] (IQRs), and counts and percentages to summarize, by year of surgery, the number of physical therapy sessions patients received to 12 months post-operatively (and per month), total annual cost of physical therapy per claim to 12 months post-operatively (expressed as 2017 AU$ and US$ as described above), and time to initiation of post-operative physical therapy. Costs were expressed using means and IQRs in the text of this paper. Mean cost is the most informative measure for healthcare resource use, while the IQR still allows the reader to understand the skewedness of the data.14 We used counts and percentages to summarize the number of physical therapy sessions (continuous variable) and physical therapy utilization at 12 months (dichotomous variable) by returned to work status at 12 months. We stratified all analyses by type of surgery (fusion versus decompression). When counting the number of physical therapy sessions per patient, we excluded non-treatment billing codes (i.e. case conference or report writing: PTA012; and physical therapist travel: PTA014). We included all billing codes when considering the cost of physical therapy. Because we had data for our total target population and this was a descriptive study, we did not use statistical inference testing. Patient characteristics were summarized by the number of physical therapy sessions they received (‘0 sessions’, ‘1–8 sessions’, ‘9–24 sessions’, ‘25–50 sessions’ versus ‘> 50 sessions’). All analyses were conducted using Stata IC Version 13.1.
ResultsStudy populationThere were 9842 claims for spine surgery from SIRA between January 1, 2010, and December 31, 2018. After relevant exclusions, our final cohort included 3524 claims/patients; 1220 had fusion and 2304 had decompression (Fig. 1).
Patient characteristicsThe mean age of patients was 41.4 ± 11.0 years, 23.9% were female, 84.9% were covered by a nominal insurer, the mean time from injury date to first surgery was 37.0 ± 51.5 months. There were 2619 (74.3%) patients who received physical therapy pre-operatively and 3126 (88.7%) who received physical therapy post-operatively (Table 1).
Characteristics of the study population by number of physical therapy sessions to 12 months post-operatively.
| Demographic and baseline variables | Total sample (n = 3524) | 0 sessions (n = 398) | 1–8 sessions (n = 814) | 9–24 sessions (n = 1068) | 25–50 sessions (n = 868) | >50 sessions (n = 376) |
|---|---|---|---|---|---|---|
| Mean Age±SD, years | 41.4 ± 11.0 | 42.9 ± 11.5 | 41.6 ± 11.1 | 41.2 ± 11.0 | 40.8 ± 11.1 | 41.5 ± 9.9 |
| Sex (Female) | 842 (23.9%) | 100 (25.1%) | 170 (20.9%) | 256 (24.0%) | 212 (24.4%) | 104 (27.7%) |
| Insurance status | ||||||
| - Nominal insurer | 2990 (84.9%) | 332 (83.4%) | 704 (86.5%) | 900 (84.3%) | 739 (85.1%) | 315 (83.8%) |
| - Self-insurer | 130 (3.7%) | 12 (3.0%) | 29 (3.6%) | 49 (4.6%) | 28 (3.2%) | 12 (3.2%) |
| - Group self-insurer | 215 (6.1%) | 24 (6.0%) | 35 (4.3%) | 66 (6.2%) | 60 (6.9%) | 30 (8.0%) |
| - Specialized | 189 (5.4%) | 30 (7.5%) | 46 (5.7%) | 53 (5.0%) | 41 (4.7%) | 19 (5.1%) |
| Type of surgery | ||||||
| - Fusion | 1220 (34.6%) | 115 (28.9%) | 240 (29.5%) | 366 (34.3%) | 333 (38.4%) | 166 (44.2%) |
| - Decompression | 2304 (65.4%) | 283 (71.1%) | 574 (70.5%) | 702 (65.7%) | 535 (61.6%) | 210 (55.9%) |
| Mean time to first surgery from injury date (SD), months | 37.0 ± 51.5 | 49.4 ± 63.4 | 38.4 ± 53.8 | 35.3 ± 49.3 | 34.3 ± 48.1 | 31.4 ± 44.0 |
| Pre-operative physical therapya | 2619 (74.3%) | 207 (52.0%) | 587 (72.1%) | 817 (76.5%) | 697 (80.3%) | 311 (82.7%) |
*: up to 12 months post-operatively.
Characteristics were similar across categories of physical therapy use, with a few exceptions. The percentage of females was lowest among those who received > 50 physical therapy sessions (27.7%), while the percentage of patients who received physical therapy pre-operatively was highest among those who received > 50 physical therapy sessions (82.7%). The percentage of patients who had fusion was highest among those who received > 50 physical therapy sessions (44.2%) and lowest among those who did not receive physical therapy (28.9%). The percentage of patients who had decompression was lowest among those who received >50 physical therapy sessions (55.9%) and highest among those who did not receive physical therapy (71.1%). Mean time from injury date to first surgery was highest among those who did not receive physical therapy post-operatively (49.4 months). Mean time (months) from injury date to first surgery decreased as the number of post-operative physical therapy sessions increased (Table 1).
Number of physical therapy sessions, cost of physical therapy, and time to initiation of physical therapyThe mean ± SD (range) number of physical therapy sessions in the 12 months following surgery was 22 ± 22 (0–160). This figure was higher for patients who had fusion compared to decompression [25 ± 23; (0–140) versus 20 ± 21 (0–160]. The number of physical therapy sessions did not change substantially between 2010 and 2017, regardless of the type of surgery (Table 2 and Supplementary File Fig. 1). The mean number of physical therapy sessions per month following surgery peaked around 3 months (3.1 ± 3.5) and gradually decreased until 12 months (0.8 ± 2.0) (Supplementary File Fig. 2).
Number of physical therapy sessions and cost of physical therapy per claim in the 12 months following lumbar spine surgery, and days to initiation of post-operative physical therapy, by year and type of surgery.
| Mean ± SD and median [IQR] number of sessionsa | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 2010–17 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |
| Total sample, mean ±SD | 22 ± 22 | 22 ± 22 | 23 ± 22 | 22 ± 21 | 20 ± 19 | 22 ± 22 | 21 ± 21 | 22 ± 22 | 22 ± 23 |
| Total sample, median [IQR] | 16 [5 - 33] | 16 [5–34] | 17 [5–34] | 16 [6–30] | 15 [5–28] | 16 [6–34] | 16 [5–31] | 17 [5–33] | 16 [4–32] |
| Max* | 160 | 140 | 106 | 115 | 126 | 111 | 100 | 160 | 139 |
| n | 3524 | 558 | 595 | 555 | 412 | 367 | 346 | 333 | 358 |
| Fusion, mean ±SD | 25 ± 23 | 25 ± 24 | 26 ± 23 | 26 ± 22 | 22 ± 20 | 24 ± 22 | 25 ± 26 | 25 ± 22 | 25 ± 26 |
| Fusion, median [IQR] | 19 [7 to 36] | 19 [5–39] | 19 [8–38] | 21 [9–35] | 15 [7–32] | 17 [7–36] | 17 [4–42] | 20 [9–42] | 18 [5–36] |
| Max* | 140 | 140 | 106 | 115 | 126 | 111 | 100 | 112 | 139 |
| n | 1220 | 191 | 224 | 209 | 132 | 116 | 115 | 100 | 133 |
| Decompression, mean ±SD | 20 ± 21 | 20 ± 21 | 21 ± 22 | 19 ± 21 | 19 ± 18 | 21 ± 22 | 19 ± 17 | 21 ± 22 | 20 ± 21 |
| Decompression, median [IQR] | 14 [4 to 30] | 14 [4–31] | 15 [4–32] | 14 [3–28] | 14 [4–27] | 16 [5–32] | 15 [5–30] | 15 [4–32] | 14 [3–30] |
| Max* | 160 | 137 | 106 | 104 | 97 | 99 | 84 | 160 | 97 |
| n | 2304 | 367 | 371 | 346 | 280 | 251 | 231 | 233 | 225 |
| Mean ± SD and median [IQR] cost of physical therapyb – adjusted to 2017 AU$ | |||||||||
| 2010–17 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |
| Total sample, mean ±SD | $1902 ± 2002 | $1877 ± 1878 | $1907 ± 1904 | $1813 ± 1833 | $1693 ± 1763 | $2020 ± 2308 | $1877 ± 1952 | $2033 ± 2041 | $2098 ± 2467 |
| Total sample, median [IQR] | $1352 [440 to 2751] | $1334 [402–2931] | $1408 [426–2856] | $1324 [468–2491] | $1231 [408–2377] | $1378 [501–2918] | $1444 [401–2637] | $1483 [496–2973] | $1303 [363–2869] |
| Max* | $18,576 | $13,539 | $12,430 | $10,960 | $11,294 | $18,576 | $15,963 | $12,824 | $13,265 |
| n | 3524 | 558 | 595 | 555 | 412 | 367 | 346 | 333 | 358 |
| Fusion, mean ±SD | $2170 ± 2212 | $2113 ± 2037 | $2134 ± 1947 | $2063 ± 1756 | $1861 ± 1865 | $2304 ± 2756 | $2240 ± 2551 | $2302 ± 2053 | $2508 ± 2971 |
| Fusion, median [IQR] | $1566 [616–3041] | $1582 [543–3108] | $1642 [664–3095] | $1670 [745–2864] | $1268 [609–2708] | $1500 [744–3230] | $1477 [366–3385] | $1903 [717–3910] | $1514 [408–2972] |
| Max* | $18,576 | $13,539 | $8857 | $10,960 | $10,236 | $18,576 | $15,963 | $10,157 | $13,265 |
| n | 1220 | 191 | 224 | 209 | 132 | 116 | 115 | 100 | 133 |
| Decompression, mean ±SD | $1761 ± 1867 | $1755 ± 1780 | $1769 ± 1868 | $1662 ± 1864 | $1614 ± 1710 | $1889 ± 2061 | $1696 ± 1547 | $1917 ± 2030 | $1855 ± 2082 |
| Decompression, median [IQR] | $1248 [371 to 2531] | $1156 [370–2763] | $1200 [357–2670] | $1131 [312–2281] | $1227 [381–2250] | $1316 [473–2702] | $1427 [448–2458] | $1372 [4145 to 2897] | $1205 [250–2521] |
| Max* | $16,626 | $12,886 | $12,430 | $10,221 | $11,294 | $16,627 | $9190 | $12,824 | $12,259 |
| n | 2304 | 367 | 371 | 346 | 280 | 251 | 231 | 233 | 225 |
| Mean ±SD and median [IQR] days to initiation of post-operative physical therapy [IQR]c | |||||||||
| 2010–17 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |
| Total sample, mean ±SD | 29 ± 49 | 30 ± 56 | 25 ± 45 | 25 ± 42 | 24 ± 42 | 31 ± 53 | 31 ± 51 | 34 ± 47 | 36 ± 54 |
| Total sample, median [IQR] | 2 [1 to 42] | 1 [1–40] | 1 [1–38] | 1 [1–40] | 1 [1–35] | 2 [1–44] | 12 [1–44] | 17 [1–54] | 17 [1–53] |
| Max* | 364 | 364 | 312 | 291 | 336 | 336 | 330 | 302 | 363 |
| n | 3126 | 500 | 530 | 496 | 372 | 321 | 311 | 294 | 302 |
| Fusion, mean ±SD | 32 ± 53 | 27 ± 50 | 28 ± 52 | 27 ± 46 | 25 ± 48 | 41 ± 65 | 37 ± 54 | 33 ± 43 | 48 ± 66 |
| Fusion, median [IQR] | 1 [1 to 50] | 1 [1–43] | 1 [1–42] | 1 [1–45] | 1 [1–29] | 2 [1–62] | 19 [1–61] | 10 [1 to 57] | 25 [1 to 67] |
| Max* | 363 | 299 | 304 | 285 | 238 | 336 | 329 | 238 | 363 |
| n | 1105 | 176 | 205 | 198 | 121 | 102 | 97 | 90 | 116 |
| Decompression, mean ±SD | 27 ± 46 | 31 ± 58 | 23 ± 40 | 24 ± 39 | 23 ± 40 | 27 ± 46 | 29 ± 50 | 34 48 | 28 ± 44 |
| Decompression, median [IQR] | 2 [1 to 40] | 1 [1–38] | 1 [1–37] | 1 [1–34] | 2 [1–36] | 2 [1–39] | 11 [1–41] | 19 [1–50] | 14 [1–43] |
| Max* | 364 | 364 | 312 | 291 | 336 | 315 | 330 | 302 | 362 |
| n | 2021 | 324 | 325 | 298 | 251 | 219 | 214 | 204 | 186 |
: only maximum value presented as minimum value was zero; aexcludes non-treatment billing items (PTA012 and PTA014); bincludes non-treatment billing items (PTA012 and PTA014); cexcludes patients with exclusively non-treatment billing items (PTA012 and PTA014).
AU$: Australian Dollars; IQR: interquartile range; n: number of patients; SD: standard deviation.
The mean [IQR] total cost per claim of post-operative physical therapy to 12 months was AU$1902 [$440-$2751] and US$1217 [$282-$1760], and this was higher for patients who had fusion (AU$2016 [$561-$2827] or US$1290 [$359-$1809]) compared to decompression (AU$1637 [$332-$2367]; US$1047 [$212-$1514]). There was a marked increase in costs between 2013 and 2014 (Table 2 and Supplementary File Fig. 3), although we are unsure of the reason (e.g. chance finding, generalized physical therapy cost increase in Australia).
The mean ± SD and median [IQR] time (days) from surgery to initiation of physical therapy was 29 ± 49 and 2 [1–42], respectively, and this was similar for patients who had fusion (32 ± 53 and 1 [1–50]) and decompression (27 ± 46 and 2 [1–40]). There was a marked increase in the median days to initiation of post-operative physical therapy between 2014 and 2015, whereas the mean showed a more gradual increase over time (Table 2).
Most patients started physical therapy within 4 weeks of surgery (n = 2124, 67.9%), compared to from > 4 weeks to 6 weeks (n = 470, 15.0%), and > 6 weeks following surgery (n = 532, 17.0%). A greater percentage of patients started physical therapy >6 weeks following fusion surgery (n = 242, 21.9%) compared to decompression (n = 290, 14.4%). The percentage of patients waiting >6 weeks to start post-operative physical therapy increased over time; increasing the most between 2013 (14.1%) and 2014 (28.4%) for patients who had fusion, and between 2015 (12.6%) and 2016 (22.6%) for decompression (Table 3).
Percentage of patients who initiated post-operative physical therapy from 0 to 4 weeks, > 4–6 weeks, and > 6 weeks.
n: number of patients. aExcludes patients with exclusively non-treatment billing items (PTA012 and PTA014).
Number of physical therapy sessions did not appear to vary by return-to-work status at 12 months. However, the percentage of patients working at 12 months post-operatively was lowest among patients who received > 50 sessions (36.2%). Patients who had fusion (compared to decompression) were less likely to be working at 12 months post-operatively (30.1% vs. 58.5%; overall 48.5%) (Table 4).
Percentage of patients who returned to work at 12 months by number of post-operative physical therapy sessions, stratified by type of surgery.
| Number of physical therapy sessions | ||||||
|---|---|---|---|---|---|---|
| Total sample | Any number of sessions | 0 | 1–8 | 9–24 | 25–50 | > 50 |
| Working | 1640 (48.5%) | 187 (49.6%) | 397 (51.5%) | 528 (51.2%) | 398 (47.3%) | 130 (36.2%) |
| Not working | 1669 (49.4%) | 170 (45.1%) | 363 (47.1%) | 477 (46.2%) | 432 (51.3%) | 227 (63.2%) |
| Retired or deceased | 72 (2.1%) | 20 (5.3%) | 11 (1.4%) | 27 (2.6%) | 12 (1.4%) | 2 (0.6%) |
| n (%*) | 3381 (100%) | 377 (11.2%) | 771 (22.8%) | 1032 (30.5%) | 842 (24.9%) | 359 (10.6%) |
| Fusion | 0 | 1–8 | 9–24 | 25–50 | >50 | |
| Working | 357 (30.1%) | 33 (30.0%) | 70 (30.0%) | 118 (32.9%) | 92 (28.5%) | 44 (27.3%) |
| Not working | 796 (67.1%) | 70 (63.6%) | 158 (67.8%) | 229 (63.8%) | 224 (69.4%) | 115 (71.4%) |
| Retired or deceased | 33 (2.8%) | 7 (6.4%) | 5 (2.2%) | 12 (3.3%) | 7 (2.2%) | 2 (1.2%) |
| n (%*) | 1186 (100%) | 110 (9.3%) | 233 (19.6%) | 359 (30.3%) | 323 (27.2%) | 161 (13.6%) |
| Decompression | 0 | 1–8 | 9–24 | 25–50 | >50 | |
| Working | 1283 (58.5%) | 154 (57.7%) | 327 (60.9%) | 410 (60.9%) | 306 (59.0%) | 86 (43.4%) |
| Not working | 873 (39.8%) | 100 (37.5%) | 205 (38.1%) | 248 (36.9%) | 208 (40.1%) | 112 (56.6%) |
| Retired or deceased | 39 (1.8%) | 13 (4.9%) | 6 (1.1%) | 15 (2.2%) | 5 (1.0%) | 0 (0%) |
| n (%*) | 2195 (100%) | 267 (12.2%) | 538 (24.5%) | 673 (30.7%) | 519 (23.6%) | 198 (9.0%) |
n: Number of patients.
Most patients had 9–24 (n = 1032, 30.5%) or 25–50 physical therapy sessions (n = 842, 24.9%) to 12 months post-operatively. There were 359 (10.6%) patients who had >50 sessions in the total sample, and a higher percentage of patients had > 50 sessions among those who had fusion compared to decompression (13.6 versus 9.0%). Overall, 377 (11.2%) patients had no physical therapy, and this percentage was higher among those who had decompression compared to fusion (12.2% versus 9.3%) (Table 4).
There were 811 (24.0%) patients who were still receiving physical therapy at 12 months post-operatively, and this percentage was higher among patients who had fusion compared to decompression (29.7 versus 20.9%). At 12 months post-operatively, a lower percentage of patients were still receiving physical therapy while working compared to not receiving physical therapy while working (39.8% versus 51.2%). A smaller percentage of patients were receiving physical therapy while working at 12 months post-operatively following fusion compared to decompression (28.4% versus 48.6%) (Supplementary File Table 2).
DiscussionPatients who had lumbar spine surgery funded by NSW Workers’ Compensation between 2010 and 2017 had, on average, 22 physical therapy sessions to 12 months post-operatively (costing AU$1902 and US$1217 per patient). One-third had 9–24 sessions, one-quarter had 25–50 sessions, and one in 10 had > 50 sessions. Patients who had fusion had more post-operative physical therapy and higher physical therapy-related costs compared to those who had decompression. Although the number of physical therapy sessions patients received following lumbar spine surgery remained stable between 2010 and 2017, the time to initiate postoperative physical therapy increased. One in four patients were still receiving physical therapy at 12 months, and most of these patients were not working.
Some patients who have lumbar spine surgery funded by NSW Workers’ Compensation are receiving physical therapy treatment beyond what may be necessary. Effective rehabilitation programs following lumbar spine surgery typically involve 8–24 sessions,5 and in our sample 35% of cases had 25 sessions or more and one in 10 had > 50 sessions in the 12 months following surgery. This suggests that some of the funded physical therapy care received by the workers may be unnecessary. Modest return-to-work rates at 12 months following surgery and the percentage of patients still receiving physical therapy at 12 months (24%) also raises questions about the effectiveness of lumbar spine surgery and post-operative physical therapy for some patients.
The median number of days to initiation of post-operative physical therapy increased from 1 to 2 days between 2010 and 2014 to 12–17 days between 2015 and 2017. This increase could be explained by possible uptake of new evidence that emerged in 2014. A 2014 Cochrane review found low- to very low-certainty evidence that exercise therapy improves pain and function in the short-term compared to no treatment, but only if exercise was delayed until 4–6 weeks post-operatively.5 Although there was an increase in the percentage of patients who commence physical therapy at least 6 weeks following surgery over time, there remains an evidence-practice gap. Since 2015, over 60% of patients still commence post-operative physical therapy within 4 weeks of surgery.
Data on physical therapy utilization following lumbar spine surgery are limited. If we compare our findings to the findings of a UK study,9 there appears to be substantial variation in the number of post-operative physical therapy sessions patients receive. The UK study, a survey of 69 outpatient physical therapy departments in the National Health Service (NHS), found 40% of patients in that setting receive 5–6 physical therapy sessions following lumbar disk surgery, while only 12% receive more than 10 sessions.9 Our study found that most patients in the workers’ compensation setting have 9–24 (30.5%) or 25–50 physical therapy sessions (24.9%) to 12 months post-operatively, and 10.6% have > 50 sessions. Variation in the amount of physical therapy provided could be explained by the increased clinical complexity of compensable patients and financial incentives to provide more care for these patients.
While numerous studies have explored the amount of physical therapy provided to patients with musculoskeletal conditions, most have reported substantially lower physical therapy utilization compared to our study. An audit of clinical notes for 200 patients with acute low back pain treated at a community-based physical therapy department in the United Kingdom found physical therapists provide a median of 5 sessions per patient (IQR: 4–7).15 A survey of 324 physical therapists in New Zealand found most physical therapists (67%) provide three treatments for patients with acute low back pain.16 For chronic low back pain, three retrospective audits of clinical notes (n = 200 patients in the United Kingdom,15n = 1254 in the Netherlands,17 and n = 3587 in the Netherlands18) and one survey of Irish physical therapists (n = 280)19 found that most physical therapists provide 6–10 sessions, with a small percentage providing over 20 sessions (< 10%). More data on practice patterns for physical therapists working with compensable patients is needed to better understand whether the relatively high amount of treatment provided in our sample can be explained by the practice setting.
Ensuring physical therapists provide care according to the best available evidence for compensable patients is vital. In NSW, there were nearly 5000 major work-related back injuries in 2015/16, costing over AU$99 million and representing 20% of all major workplace injuries.20 The lack of data on physical therapy practice patterns in this setting highlights the need for more research in this space. A separate issue yet to be investigated is what drives patterns of physical therapy practice in settings involving compensable patients. Physical therapists managing patients funded by NSW Workers’ Compensation are initially approved to provide eight sessions. Physical therapists do not need to justify the necessity of these sessions and can request additional sessions (in blocks of eight) if needed. Having physical therapy sessions approved in blocks through a relatively straight-forward process may be contributing to ongoing treatment in this setting despite any measurable improvement in outcomes such as return to work. Future qualitative research is needed to better understand the barriers and facilitators to providing evidence-based care in this setting and inform the development of interventions to improve physical therapy practice if necessary.
Our sample represents almost the entire population of patients who underwent elective lumbar spine surgery funded by NSW Workers’ Compensation between 2010 and 2017. A large sample size and 8 years of data allowed us to explore how physical therapy utilization and costs have changed over time. A key limitation is that we used administrative, billing data so were unable to discern whether physical therapy improved patient outcomes. We also had no data on the type of physical therapy provided (e.g. exercise, electrotherapy) so could not determine whether physical therapy provided following lumbar spine surgery aligns with current best available evidence. Because our data were limited to claims funded by NSW Workers’ Compensation, physical therapy treatments received after claims had closed or outside the scheme would not be detected.
ConclusionThere is substantial variation in how many physical therapy sessions patients funded by NSW Workers’ Compensation receive in the 12 months following lumbar spine surgery in Australia, the cost of this care, and the time from surgery to the initiation of physical therapy. On average, patients received 22 physical therapy sessions and generated physical therapy-related costs of AU$1902 and US$1217 per patient in the 12 months following lumbar spine surgery. For most claimants, the number of physical therapy sessions received aligned with the best available evidence. However, some patients may have received an excessive amount of physical therapy and initiated physical therapy too early. One in three patients received >24 sessions, one in 10 received >50 sessions, one in four were still having physical therapy by 12 months, and over two-thirds commenced physical therapy within 4 weeks of surgery. Physical therapists should reflect on these data when planning the management of patients following lumbar spine surgery. Patients who received > 50 sessions and who were still having physical therapy by 12 months were least likely to be working. Future research is needed to determine the value of physical therapy being provided in this setting.
The authors would like to acknowledge Professor Robert Herbert for his help with the analyses.