It is unknown whether online information about the benefits and harms of surgery contains an accurate description of evidence.
ObjectiveTo describe the proportion of webpages containing information about surgery for spinal pain (decompression and fusion) that accurately described the evidence on the benefits of surgery, described harms, and provided quantitative estimates of these harms.
MethodsWe performed a content analysis of webpages containing information about spine surgery. Two reviewers identified webpages and extracted data. Primary outcomes were the proportion of webpages that accurately described the evidence on the benefits, described harms, and provided quantitative estimates of these harms.
ResultsWe included 117 webpages. Only 29 (25%) webpages accurately described the evidence on the benefits of spine surgery, and more webpages on decompression accurately described the evidence compared to webpages on fusion (31% vs 15%, difference in proportions = 16%; 95% CI: 2%, 31%). Harms of surgery were described in most webpages (n = 76, 65%), but a much smaller proportion of webpages (n = 18, 15%) provided a quantitative estimate for the mentioned harms.
ConclusionsMost webpages failed to accurately describe the benefits and harms of decompression and fusion surgeries for spinal pain. Unbiased consumer resources and educating the public on how to critically evaluate health claims are important steps to improve knowledge on the benefits and harms of spine surgery.
Decompression and fusion are the most common surgeries performed for spinal pain, a prevalent and costly condition for individuals and health systems.1 Decompression is often indicated for people with spinal pain and radicular symptoms due to disc herniation and spinal stenosis, whereas fusion has a broader list of indications (e.g. degenerative disc disease, disc herniation, stenosis, and spondylolisthesis).2,3 Their use is increasing over time in many countries. For example, rates of decompression have increased by 138% from 1999 to 2013 in Norway.4 Spinal fusion rates have increased at a similar rate in many countries. In Australia, there has been a 167% increase from 1997 to 2006 in the private sector; a 154% increase from 1999 to 2013 has been described in Norway; and a 62% increase from 2004 to 2015 has been described in the United States.4-6
Decompression is effective for people with radicular symptoms due to disc herniation and spinal stenosis compared to non-operative treatment.7-9 However, because most patients with radicular symptoms improve without surgery in the short-term,10,11 surgery is typically recommended to those who have not responded to an initial course of non-operative care.10,12 In contrast, the benefits of fusion over non-operative treatment are unclear; randomised trials have shown that fusion is not more beneficial than non-operative treatment or less complex surgeries (such as decompression alone).13-15 In addition, 1 in 6 people undergoing spinal fusion develop early post-surgical complication such as infections, thrombosis, nerve injury, or major bleeding during the surgery.14 Given the unclear benefit of fusion compared to non-operative care and the high risk for complications, fusion is not recommended in guidelines for low back pain with or without radicular symptoms.12
To make sense of their pain and seek information about their treatment options, many people use the internet. In Australia, about 8 in every 10 people report having used the internet in the past year to obtain health information for various reasons including to assist with treatment decision-making.16,17 A previous study has shown that online information about low back pain is not accurate, but very few webpages included in that study mentioned surgery.18 Hence, it is unknown whether online information about the benefits and harms of surgery contains an accurate description of evidence. Other studies that did examine webpages providing recommendations on spine surgery have only described the readability of information available.19,20 An investigation of how webpages portray the benefits and harms of common surgeries for spinal pain has not been published. If online information about spine surgery does not include an accurate description of evidence, that might bias patients towards having spinal surgery when there is no clear evidence to support the use of this intervention rather than non-operative care and less complex surgeries. This information is relevant for health professionals, including physical therapists, who often see patients who are considering surgery and may have misconceptions about the benefits and harms of spinal surgery.
The primary aims of this study were to describe the proportion of consumer webpages containing information about surgery for spinal pain that had an accurate description of evidence on the benefits, described harms, and provided quantitative estimates of these harms.
METHODSStudy designWe performed a content analysis of online consumer information about decompression and fusion surgeries for spinal pain. Content analysis is an analysis tool used to determine the presence of certain themes or concepts within qualitative data (e.g. text).
Eligibility criteriaWe included any webpage written in English targeted to consumers that discussed the use of decompression and fusion. We excluded links to webpages that did not mention fusion or decompression (e.g. only discussed anatomy, risk factors for developing spinal pain, or non-operative care), journal articles, YouTube links, webpages aimed at health professionals, advertisements promoted by Google, and duplicates.
Search strategy and selection of webpagesOur search strategy aimed to find webpages that a person interested in spine surgery might encounter if they conducted a search on Google from Australia. We conducted searches on Google between April 1st and 8th, 2021 using a combination of keywords commonly used to describe fusion or decompression surgery. We chose to only search Google as it is the most used search engine worldwide and has the best search validity (i.e., returns links to webpages that can be opened).21 We used a combination of terms described in Supplementary File - Table 1. These terms were defined by the study team, which includes professionals from various backgrounds including physical therapists and orthopaedic surgeons and based on previous studies investigating online information for musculoskeletal conditions.22 We searched the first 2 pages of results as people are unlikely to explore webpages beyond the second page of a Google search.18 Two researchers independently performed the searches using the Google Chrome web browser and selected webpages according to the inclusion criteria. Before every new search, we cleared browsing data.23 Any disagreements were resolved by consensus, which was achieved through discussion.
Characteristics of the included webpages. Data are reported as frequency (%).
*Other types of webpages include free encyclopaedia (n = 2) professional association (n = 1), medical device company (n = 1), and comparison website (n = 1).
Pairs of independent reviewers, from a panel of four, extracted the data into a piloted Excel spreadsheet. Disagreements were resolved by consensus. We extracted bibliometric data from the website (e.g. URL, title of the page, owner), data on indications for surgery (e.g. disc herniation, degenerative disc disease, fracture), information about the benefits of surgery (e.g. estimation of success rate, full recovery, reported benefits in terms of surgical or patient outcomes or both), and harms (e.g. listed at least one harm). The coding framework is described in Supplementary File - Table 2.
Primary and secondary outcomes.
Primary outcomes were the proportion of webpages that had an accurate description of evidence on the benefits, described harms, and provided quantitative estimates of these harms. For webpages on fusion, we considered that a webpage correctly portrayed the evidence on the benefits of surgery when it stated that fusion does not provide a clear benefit over non-operative care for spinal pain not related to serious spinal pathologies.12,14,15 For decompression, a webpage was considered to correctly portray the evidence on its benefits when it stated that decompression was indicated for people with radicular symptoms (e.g. leg pain) or that patients should expect to experience an improvement mainly in radicular symptoms post-surgery.8,12,24 We considered a webpage to describe harms when at least one known harm of either surgery (e.g. infection) had been described. We evaluated whether quantitative estimates of harms had been presented (e.g. proportions, natural frequencies, etc.). Harms were considered important because a description of the surgery confined to effectiveness not mentioning harms or not providing numerical estimates for these harms would not assist informed decision-making.
Secondary outcomes were the proportion of webpages (i) describing indications for surgery and the number of indications listed, (ii) providing an estimation of success rate, (iii) describing outcomes of surgery either in terms of patient-reported outcomes (e.g. improvement in pain and function) or in terms of surgical outcomes (e.g. fusion rates), and (iv) suggesting full recovery after surgery could be achieved.
Data analysisWe used descriptive statistics (counts and percentages or means [SD]) to summarise data and reported overall and stratified findings by type of surgery. Results were compared between webpages of decompression and fusion using a test of equality of proportions for dichotomous outcomes and independent t-test for continuous outcomes and presented as differences between proportions and differences between means and 95% confidence intervals (CI). We used Stata Version 16.0 (College Station, Texas, USA).
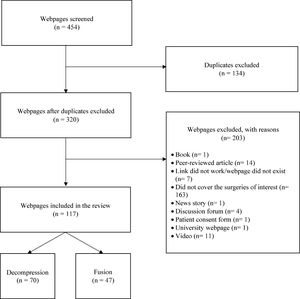
ResultsWe screened 454 potentially eligible webpages. After excluding irrelevant webpages, 117 webpages from 76 unique websites remained in the study. Of the 117 included webpages, most covered decompression (n = 70, 60%) followed by fusion (n = 47, 40%). A flow diagram describing the screening process and reasons for exclusion is shown in Figure 1. The included webpages are described in Table 1.
Primary outcomesAccurate description of evidence on benefitsOf the 117 webpages, only 29 (25%) had an accurate description of evidence on the benefits of spine surgery. A greater proportion of webpages on decompression (n = 22, 31%) had an accurate description of evidence compared to webpages on fusion (n = 7, 15%), and this difference was statistically significant (difference in proportions = 16%; 95% CI: 2%, 31%) (Table 2).
HarmsHarms of surgery were mentioned in most webpages (n = 76, 65%) and were similarly distributed amongst webpages covering decompression (n = 48, 69%) and fusion (n = 28, 60%) with no difference in proportions between decompression and fusion webpages (difference in proportions = 9%; 95% CI: −9%, 27%). A much smaller proportion of webpages (n = 18, 15%) provided a quantitative estimate for the mentioned harms. These were similarly distributed between webpages covering decompression (n = 13, 19%) and fusion (n = 5, 11%), with no difference between them (difference in proportions = 8%; 95% CI: −5%, 20%).
Secondary outcomesIndicationsMost webpages (n = 104, 89%) listed indications for each of the surgeries. For decompression, webpages typically described disc herniation (n = 53, 76%), pain (n = 42, 60%), failed conservative treatment (n = 41, 59%), and spinal stenosis (n = 34, 49%) as indications. For fusion, most common indications were degenerative disc disease (n = 26, 55%), spondylolisthesis (n = 23, 49%), and instability (n = 22, 47%). Webpages covering fusion listed significantly more indications than webpages covering decompression (5.2 ± 3.6 vs 3.4 ± 1.9 indications; mean difference = 1.7; 95% CI: 0.7, 2.8) (Table 2).
Estimation of success rateTwenty-six (22%) webpages provided an estimated success rate of surgery. A greater proportion of webpages estimating a success rate covered decompression (n = 21, 30%) compared to fusion (n = 5, 11%), and this difference was statistically significant (difference in proportions = 19%; 95% CI: 5%, 33%).
Of the 21 webpages providing an estimated success rate of decompression, only 9 (43%) clearly described those benefits were mostly for leg pain. For the other 12 (57%) webpages, it was unclear how they defined success. Reported success rates ranged from 70% to 98%. Of the five fusion webpages, there was variation in the estimated success rate of surgery, which ranged from 62% to 80% satisfaction rates post-operatively. One webpage mentioned that pain is typically decreased by 50% after fusion.
Outcomes describedA greater proportion of webpages described the effects of surgery in terms of a surgical outcome (n = 100, 85%) than a patient-reported outcome (n = 78, 67%). A greater proportion of pages on decompression (n = 64, 92%) described a surgical outcome compared to pages on fusion (n = 36, 77%), and the difference was statistically significant (difference in proportions = 15%; 95% CI: 11%, 29%). Similarly, a greater proportion of webpages on decompression (n = 51, 73%) described a patient-reported outcome compared to webpages on fusion (n = 27, 57%), and the difference was statistically significant (difference in proportions = 16%; 95% CI: 2%, 33%).
Expectations of full recoveryOnly 10 (9%) webpages clearly mentioned that patients should expect to fully recover after surgery. Most of them covered decompression (n = 7, 10%) and only 3 (6%) covered fusion, with no significant differences between the surgeries (difference in proportions = 4%; 95% CI: −6%, 14%).
DiscussionWe reviewed the content of 117 webpages covering fusion and decompression surgeries for spinal pain. Overall, only a quarter of webpages had an accurate description of evidence on the benefits of each surgery, but the number of webpages covering fusion that represented current best evidence was significantly lower than those covering decompression. Harms were mentioned by 65% of webpages, however, only 15% provided some quantitative estimate of harms without differences between decompression and fusion surgeries. Webpages on fusion listed significantly more indications than decompression webpages. An estimation of success rate was provided by 22% of webpages, and a greater proportion of webpages on decompression did so compared to webpages on fusion.
Previous studies assessing online information about spine surgery investigated different aspects of webpages, such as readability and quality19,20 or focused on non-commercial webpages.18 In the paper by Zhang et al.,19 quality was assessed using a scoring system ranging from unacceptable to excellent based upon the presence or absence of a list of indications, benefits, harms, alternatives, description, and whether there were references to peer-reviewed literature.19 However, that study only examined webpages covering fusion, and did not use current evidence on the benefits and harms of fusion as a benchmark for treatment recommendations. In a review of non-commercial webpages from trustworthy sources (e.g. government bodies, hospitals, healthcare organisations), 76% and 59% of webpages had no or unclear recommendations for fusion and decompression, respectively.20 Our study searched for a different subset of webpages (both commercial and non-commercial) in an attempt to replicate what a consumer interested in spine surgery would find from a Google search. This allowed us to explore publicly available online information about the benefits and harms of spine surgery.
Most webpages failed to have an accurate description of evidence on the benefits of fusion and decompression surgery, and webpages on fusion performed significantly worse compared to webpages on decompression. One potential explanation for our findings is that 62% of webpages included in our study are from orthopaedic surgery or neurosurgery private practices, and therefore it may not be within their interests to describe that some surgeries such as spinal fusion are not more effective than some forms of non-operative treatment such as intensive rehabilitation or less complex surgeries such as spinal decompression (e.g. laminectomy).14,25
A very small proportion (11%) of webpages provided quantitative estimates of the potential harms of fusion. As about 1 in 6 patients undergoing lumbar fusion develop some form of early complication after surgery (e.g. infection, thrombosis, nerve injury, etc.), providing quantitative estimates of harm is important for patients to make informed decisions about their care by correctly weighing benefits against potential harms.26
Definitions of ‘success’ after surgery varied considerably across webpages. Some expressed success in terms of percentage of pain reduction, others described the percentage of patients achieving significant reduction in pain, good to excellent results, or long-term success. Importantly, no webpage described the success in relation to other options, such as other treatments or even no treatment at all. This points to the urgent need for the development of resources for patients containing unbiased information about the benefits and harms of spinal fusion. A decision aid providing estimates of the benefits and harms of spinal fusion compared to less complex surgeries or non-surgical treatments could improve patients’ informed decision-making process about whether or not to have this type of surgery.27
This study has some limitations. Searches were conducted in Australia and we only included webpages written in English, so it is unclear whether our findings are generalisable to other countries and to webpages written in different languages. However, we designed our search strategy to replicate what a person interested in spine surgery might search for and what they would find if they conducted the search in Google from Australia. We cleared browsing data before conducting every search; however, it is possible that our searches might not reflect those made by someone who has never searched anything about spinal pain or spine surgery before. We also excluded advertisement webpages, which means we might have missed some important webpages. Nevertheless, we included a range of websites from local clinics that are likely to come up on any Google search. We also ran multiple searches using different terms which we believe would have reduced the number of missed webpages. We used the best evidence available from randomised trials, systematic reviews, and guidelines as benchmarks for one of our primary outcomes: evidence of benefit. However, it is possible future research may change what we considered to be the best available evidence for each of the surgeries.
There is some preliminary evidence that websites containing evidence-based information about the management of spinal pain may improve treatment decisions – although it is unclear whether this improvement might be clinically relevant.28 For example, the MyBackPain website was developed by experts with extensive input from consumers and contains evidence-based updated information about the management of low back pain.29 Interestingly, this website has not appeared in any of our searches, which highlights the need for further development of this resource to make it more visible to consumers interested in treatments for back pain. Clinicians from various backgrounds, including physical therapists, could improve uptake of websites containing evidence-based information by referring their patients to these resources. Addressing misconceptions from poor online information could be one strategy physical therapists could use to reduce the overuse of these surgeries. There are also opportunities for adapting the content to other languages to address the language barrier in non-English speaking countries. These initiatives will contribute to improving knowledge translation of the benefits and harms of surgeries for spinal pain.
Besides creating and promoting websites with more accurate information for consumers, mass advertisement campaigns on the internet could be a promising way to harness the benefits of websites containing evidence-based treatments for patients. For example, a recent trial showed that professionally designed public health advertisements increased interest in healthy lifestyle searches (e.g. weight loss) by 50%.30 Social media also offers opportunities for media campaigns. Social media messages recorded by health professionals before the winter holidays in the United States led to a significant reduction in holiday travel and subsequent COVID-19 infections.31 There are also opportunities to investigate the effectiveness of different aspects of such advertisements, such as language and framing.32
ConclusionMost webpages covering fusion and decompression failed to accurately describe the evidence on the benefits of these surgeries, and webpages on fusion were less likely to provide such description. Although harms were mentioned by many webpages, a very small proportion provided a quantitative estimate of harms. Webpages on fusion listed significantly more indications than webpages on decompression. Overall, webpages included in our study present an optimistic view of surgery, particularly fusion. This may mislead patients into thinking spinal fusion is an effective surgery for a range of conditions affecting the spine. There is an urgent need for further developing and promoting unbiased consumer resources on the benefits and harms of spine surgery, particularly fusion.