A common misconception about low back pain (LBP) is that the spine is weak and that lumbar flexion should be avoided. Because the beliefs of health-care professionals (HCPs) influence patients, it is important to understand the attitudes of health care professionals towards LBP and lifting.
ObjectivesTo assess and compare the perceptions of different categories of HCPs regarding the safety of specific movement strategies used to lift a light load, and their beliefs regarding back pain. The secondary aim was to determine whether certain factors influenced the beliefs of HCPs.
MethodsData were collected via an electronic survey. Student and qualified physical therapists (PTs), medical students, and general practitioner (GP) trainees were included. The questionnaire included eight photographs, depicting eight different strategies to lift a light load. Respondents were requested to select the strategy(s) they considered as “unsafe” to use for asymptomatic people with a previous history of LBP and people with chronic LBP. Beliefs and attitudes towards LBP were evaluated using the Back Pain Attitudes Questionnaire (Back-PAQ).
ResultsQuestionnaires from 1005 participants were included. Seventy percent of qualified PTs considered none of the strategies as harmful (versus 32% of PT students, 9% of GP trainees and 1% of medical students). Qualified PTs had higher Back-PAQ scores (mean ± SD: 13.6 ± 5.5) than PT students (8.7 ± 5.7), GP trainees (5.9 ± 5.9) and medical students (4.1 ± 5.2), indicating less misconceptions regarding LBP. Having LBP negatively influenced beliefs while taking a pain education course positively influenced beliefs.
ConclusionMisconceptions regarding LBP and the harmfulness of lifting a light load with a rounded back remain common among HCPs, particularly medical doctors.
Low back pain (LBP) is common and is the leading cause of disability worldwide.1 The etiology of LBP is rarely known, and therefore, the condition is frequently referred to as non-specific LBP.2-4 The societal costs of this condition are considerable and are projected to increase in the coming decades.1
Misconceptions about LBP are very frequent; the media, internet, family and friends, previous experiences, and the attitude of health care professionals (HCPs) all contribute to patients’ beliefs about LBP.1 Misconceptions can negatively influence both the pain experience and its evolution.5 A large body of evidence shows that the pain experience depends on the person's perception of his/her illness, and that psychosocial factors contribute strongly to pain intensity and functional disability.6
The most common misconceptions among people with LBP, as well as the general population, are that the spine is a vulnerable structure which can be easily injured, and that bending is dangerous for the spine.7,8 A population-based cross-sectional survey in New Zealand showed that 93.5% of respondents believed that lifting without bending the knees was not safe for the back.9 Although some HCPs consider that "poor postures" (e.g. not keeping the back straight to pick-up/lift something) are a risk factor for LBP and recommend using specific lifting techniques, systematic reviews have shown that advice and training in the use of “safe strategies” do not reduce work-related musculoskeletal disorders or prevent LBP.10-13
Misconceptions are not only common in the general population, but a recent study also showed that both manual handling advisors and physical therapists believe that lifting with a round back is unsafe.14 HCPs influence patient understanding of LBP through their explanations of pathoanatomy and the advice they provide. Recent studies highlighted the impact and influence of HCPs upon the attitudes and beliefs of people with acute and chronic LBP as well as pain-free people.5,7 Misconceptions among HCPs can therefore lead to fear avoidance and maladaptive lifting strategies that may be pro-nociceptive.15
While the optimal posture/strategy for lifting a heavy load is still debated, there is no evidence to suggest that flexing the lumbar spine while lifting a light load is harmful.16 Furthermore, it has recently been demonstrated in pain-free individuals that lifting heavy loads with a flexed lumbar spine rather than a lordotic / straight posture increased the body's ability to generate a trunk extensor moment and significantly improved neuromuscular efficiency.16,17 Despite this, HCPs and the media frequently recommend systematically flexing the knees instead of flexing the spine to prevent or reduce LBP.7Another strategy frequently found in health guidelines and taught by HCPs to reduce the risk of injury is to pre-activate the abdominal muscles to increase spine stability.18,19 However, the biomechanical or motor-control advantage of abdominal bracing during lifting is unclear.20
To our knowledge, no studies have evaluated the beliefs and attitudes of different HCPs towards safe and unsafe strategies to use when lifting a light load. The primary aim of this study was therefore to assess and compare the perceptions of different categories of HCPs regarding the safety of specific movement strategies used to lift a light load, and their beliefs regarding back pain. The secondary aim was to determine whether certain factors influenced the beliefs of HCPs: e.g., having personally experienced LBP or having completed a pain education course (for qualified physical therapists [PTs]).
MethodsParticipantsWe conducted a cross-sectional survey which was approved by the Ethics Committee of the Cliniques Universitaires Saint-Luc – Brussels (2018/10JUL/283).
Four groups of HCPs were recruited: PT students, medical students, qualified PTs, and general practitioner (GP) trainees. All faculties and schools of physical therapy and medicine in Belgium were contacted and invited to ask their students (PT and medical students and GP trainees) to participate in the survey. Nineteen schools of physical therapy in France were also contacted. Qualified PTs were recruited from physical therapy school/faculty databases and via social networks, including specific PT interest groups (Facebook, Twitter, and Instagram). The inclusion criteria were:
- -
PT students had to be enrolled in an undergraduate PT course in a French-speaking Belgian physical therapy school or in a French physical therapy school;
- -
Qualified PTs had to be practicing in Belgium or France;
- -
Medical students had to be in their sixth year of undergraduate training in a French or French-speaking Belgian university/medical school;
- -
GP trainees had to be qualified doctors who were training as GPs in a French or French-speaking Belgian university/medical school.
Only complete surveys were included in the analysis.
QuestionnaireThe questionnaire developed for this study was submitted via the online Lime-Survey platform. All questionnaires were anonymous. The questionnaire was composed of four sections. The first section provided information about the study and registered consent for participation. The second section requested demographic information (age, sex, HCP category, etc.). Respondents were also asked to indicate if they currently had LBP or had a history of LBP. The third section evaluated perceptions of unsafe movement strategies using a custom-made tool composed of photographs (see below), and the fourth section assessed evaluations and beliefs regarding LBP using the Back Pain Attitudes Questionnaire (Back-PAQ).21
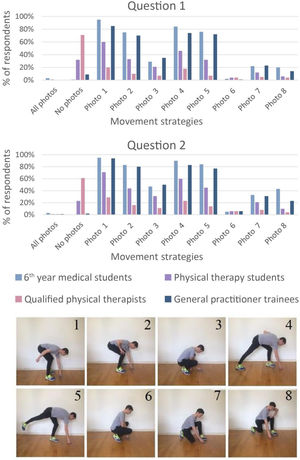
Movement strategy safety questionnaireEight photographs of different strategies used to lift a key ring from the floor were presented (Fig. 1). After observing the photographs, participants were asked to select photographs in response to the following two questions:
Q1: Which movement strategy(s) would you not recommend to an asymptomatic individual with a history of low back pain to pick up a key ring?
Q2: Which movement strategy(s) would you not recommend to a patient with chronic low back pain to pick up a key ring?
Photographs of eight movement strategies for lifting a light load from the floor used in the movement strategy safety questionnaire. According to the literature, all strategies are safe for people with a history of, or chronic low back pain. This tool was found to have content validity during a pilot study.
Any number of movement strategies (or none) could be selected.
The strategies shown in the photographs were developed from field observations, the literature, and a preliminary tool developed in a previous study.22 According to the literature, none of these strategies would be harmful if used to lift a light load from the floor.23 The validity of the 8 strategies was evaluated in a pilot study involving 12 experts (PT specialized in musculoskeletal disorders with >5 years of experience). Eleven of the 12 experts considered that these strategies were the most commonly used by the general population, suggesting good face validity. Furthermore, all 12 experts considered that none of the strategies would be harmful to either individuals with a history of LBP or with chronic LBP.
Back pain attitudes questionnaire (Back-PAQ)The Back-PAQ evaluates beliefs and attitudes about LBP.8,24,25 The short version (French version) was used.21 It is composed of 10 items classified into five categories: back vulnerability (items 1 and 2), the relationship between back pain and injury (items 3 and 4), participation in activities during back pain (items 5 and 6), the psychological influences of back pain (items 7 and 8), and the prognosis of back pain (items 9 and 10).5 Each item is scored from −2 (“True”) to +2 (“False”) and the total score ranges from −20 to +20 (the scores of items 6, 7, and 8 are reversed for the calculation). More negative scores indicate greater misconceptions regarding LBP.8
Statistical analysisAll statistical analyses were conducted using SPSS Statistics 25, with a significance level of 5%. Normality was checked with the Kolmogorov-Smirnov test. If data followed a normal distribution, an additional test for homogeneity of variance was added. One-way analyses of variance (ANOVA) were used to determine between-group differences for the primary outcomes (mean number of photographs selected and mean Back-PAQ total score). If significant, post-hoc tests with a Tukey correction were applied to determine which groups differed. Mean difference (MD) and 95% confidence interval (CI) for between-group comparisons were calculated.
A chi-square test was performed to verify that the Back-PAQ score was not based on the age distribution, sex, or number of selected photographs.
Potential confounders were assessed using multivariate analysis. Poisson regression and linear regression were performed (respectively for the number of photographs selected and for the Back-PAQ total score) to investigate the association between the independent variables (number of photographs selected and Back-PAQ total scores) and the dependent variable (HCP category) with age and sex as potential covariates.
For the secondary aims, T-tests were conducted to compare respondents with/without LBP and qualified PTs who had/had not attended a course in pain education.
ResultsData were collected from 19 November 2018 to 31 December 2018. A total of 1357 individuals responded to the survey, however only 1005 fully completed the questionnaire and were included in the analysis.
Twenty-one French and Belgian physical therapy schools accepted to forward the survey web link to their students. Four hundred and seventeen physical therapy students (41.5% of total respondents) completed the questionnaire: 333 (79.9%) were from French-speaking Belgian physical therapy schools and 84 (20.1%) were from 11 French physical therapy schools.
Three hundred and ninety-five qualified PTs (39.3% of total respondents) completed the questionnaire: 249 (63.1%) worked in France and 146 (36.9%) in Belgium. Mean number of years of practice was 7 (min of 1, max of 38). They reported treating an average ± standard deviation of 12 ± 10.5 (range 0–90) patients with LBP weekly and 23.5% reported having attended a pain education course.
One hundred and eight GP trainees (10.7% of total respondents) and 85 medical students (8% of total respondents) completed the questionnaire: they came from the three French-speaking Belgian universities of medicine. The GP trainees reported seeing 6.57 ± 12 (1–100) patients with LBP on average per week.
Date on age, sex, and history of LBP for the study participants are presented in Table 1.
Descriptive summary of the four groups (n = 1005).
Data are Mean ± SD (range) or Frequency n(%).
The mean ± SD number of photographs selected by the respondents was 1.90 ± 2.08 for asymptomatic individuals with a history of LBP (Q1) and 2.54 ± 2.36 for those with chronic LBP (Q2).
Fig. 2 presents the rate of selection of each photograph for both questions in each group. Strategies 1, 2, 4, and 5 illustrating rounded backs were selected more frequently than strategies 3, 6, 7, and 8 which depicted knee flexion.
Results for the movement strategy safety questionnaire for each group expressed in percentages. Q1) Which movement strategy(s) would you not recommend to an asymptomatic individual with a history of low back pain to pick up a key ring? Q2) Which movement strategy(s) would you not recommend to a patient with chronic low back pain to pick up a key ring?
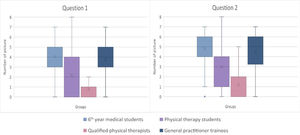
The mean number of photographs selected (Fig. 3, Table 2) differed significantly between groups for both questions, except between GP trainees and medical students (Question 1 MD=−0.4, 95%CI:−0.9, 0.1 Question 2 MD=−0.3, 95%CI:−0.8, 0.2). For both questions, the mean number of photographs selected by qualified PTs were lower than for the other three groups, and the mean number of photographs selected by PT students were lower than for medical students and GP trainees.
Mean number of photographs selected by each group of health care professionals. Q1) Which movement strategy(s) would you not recommend to an asymptomatic individual with a history of low back pain to pick up a key ring? Q2) Which movement strategy(s) would you not recommend to a patient with chronic low back pain to pick up a key ring?
Back-PAQ score, number of photographs selected for question 1 (Q1) and question 2 (Q2) for each HCP category.
Data are mean ± standard deviation and mean difference (95% confidence interval). Abbreviations: Back-PAQ, Back Pain Attitudes Questionnaire; GP, General Practitioner.; HCP, Health Care Professional; PT, Physical Therapist.
The Poisson regressions confirmed the significant group effect on the number of photographs selected for Q1 (p<0.0001) and Q2 (p<0.0001). There was no significant effect of sex for Q1 (p = 0.30) and Q2 (p = 0.10). There was no effect of age for Q1 (p = 0.98) and Q2 (p = 0.68).
Back-PAQ scoreThe mean Back-PAQ score (Table 2) for the qualified PTs was higher than that of the PT students (MD= 4.9, 95%CI: 4.2, 5.7), GP trainees (MD= 7.4, 95%CI: 6.4, 8.8), and medical students (MD= 9.5, 95%CI: 8.2, 10.8), suggesting they had fewer misconceptions regarding LBP. Mean PT student score was higher than that of the GP trainees (MD= 2.7, 95%CI: 1.5, 3.9) and medical students (MD= 4.6, 95%CI: 3.4, 5.9). There were no differences between medical students and GP trainees.
The linear regression confirmed the significant effects of group (p<0.0001), sex (p<0.0001; higher scores for men), and age (p = 0.0003: lower scores with increasing age).
Subgroup analysesResults for the subgroup analysis are presented in Table 3. The mean Back-PAQ scores for respondents with LBP (n = 142) were lower than those without LBP (n = 863) (MD= −2.6, 95%CI: −2.6, −2.5). Respondents with LBP had slightly more pictures selected than respondents without LBP for question 1 (MD= 0.4, 95%CI: 0.0, 0.8) but not for question 2.
Back-PAQ score, number of photographs selected for question 1 (Q1) and question 2 (Q2) for respondents with or without LBP since at least 24 h and for qualified PT who did or did not attend to a pain course.
Data are mean ± standard deviation and mean difference (95% confidence interval). Abbreviations: Back-PAQ, Back Pain Attitudes Questionnaire; GP, General Practitioner.; HCP, Health Care Professional; PT, Physical Therapist.
Qualified PTs who had attended a pain education course (n = 90) had higher Back-PAQ score (MD= 3.8, 95%CI: 2.6, 5.1) and fewer photographs selected for question 1 (MD= −0.8, 95%CI: −1.1, −0.4) and question 2 (MD= −0.9, 95%CI: −1.3, −0.5) than those who had not attended a pain education course (n = 305).
DiscussionTo our knowledge, this is the first study to investigate and compare the perceptions of different groups of HCPs regarding the harmfulness of specific movement strategies used to lift a light load from the floor for patients with a history of LBP or chronic LBP. The results revealed that some HCPs have misconceptions regarding the safety of certain movement strategies. Whereas the majority of qualified PTs (77%) and PT students (71%) were aware that none of the strategies depicted were unsafe, more than 90% of the medical students and GP trainees believed that at least one strategy should not be recommended. The strategies involving a rounded back (photos 1, 2, 4, and 5) were often considered as unsafe, as was found by Nolan et al.14 These HCPs also had significantly lower Back-PAQ scores indicating that they had a higher level of misconceptions regarding LBP than the PT groups. Such misconceptions among doctors have previously been found and may be due to the use of a biomedical approach to LBP.5 Doctors are therefore more likely to advise patients with LBP to use caution when moving, lifting, and exercising to protect the spine, advice which is considered to have a negative effect on recovery as it can lead the patient into a vicious circle of fear and protective behavior.1,5,8,14,26-30 In contrast, reassurance and positive attitudes and beliefs towards LBP and movement has been shown to promote recovery.31 The perceived vulnerability of the spine is a well-known risk factor for chronic LBP and should be countered by education that helps patients to understand that their spine is a strong structure, rather than advice to be cautious when bending the back.32,33
In vitro and in vivo studies performed in the 1960s that suggested that lumbar flexion increased intradiscal pressure and favored disk injuries led to the classical recommendation that lifting should be performed with a straight back.34-36 Also, Nachemson et al.33,35 reported that lifting with a rounded back generated greater intradiscal pressure and a higher risk of disk injury.35,37 More recently, measurements from instrumented vertebral body replacements (VBRs) indicated that differences in intradiscal pressure between stoop and squat lifting were only minor for light loads.34,38,39 A recent systematic review and meta-analysis found no evidence from in vivo studies that lumbar spine flexion should be minimized to prevent LBP onset, persistence, or recurrence.23 Furthermore, straight back lifting postures have been shown to be associated with higher levels of fear of movement and lower levels of self-efficacy.40,41 Despite this, Nolan et al.14 reported that 76% of physical therapists and 91% of manual handling advisors considered that lifting with a straight back is safer than with a rounded back. These results demonstrate that work is needed to change HCPs understanding of LBP so that patients receive appropriate advice that facilitates, rather than impedes their recovery.
The large difference in the attitudes and beliefs of the MD and PT groups found in this study could be explained by differences in the models of care taught to these professions. Physical therapy training follows a biopsychosocial model and includes understanding of psychosocial factors (e.g. misconceptions regarding LBP), the importance of moving, and the fact that pain is different from nociception. In contrast, medical training is more often based on a biomedical approach (i.e. linear relationship between structural pathology and the experience of pain).42 McCabe et al.41 showed that a targeted educational session on LBP successfully dispelled some back pain myths among medical students.43 Furthermore, in the present study, the qualified PTs who had attended a pain education course had fewer misconceptions than those who had not. Targeted education programs on LBP would therefore be pertinent as part of the undergraduate medical training course.43
Regarding our secondary aims, we found that respondents who had LBP showed a higher level of misconception than those without LBP. Our results are consistent with the finding by Christe et al.44 showing that not having current LBP was significantly associated with a lower Back-PAQ score indicating a lower level of misconception in the 34 items version of the Back-PAQ used in that study. However, the difference between these two groups were less present regarding the number of movement strategies considered as unsafe.
We finally found that attending a pain education course positively influenced the Back-PAQ score and the number of strategies depicted as unsafe to lift a light load. It was also previously shown that attending a pain neurophysiology course directly improved sport therapy and rehabilitation student's attitudes towards athletes with pain as well as physical therapy student's knowledge, attitudes, and recommendations for pain management.45,46
Although the present study has a large sample size, it has several limitations. First, the use of an online survey may have led to selection bias because it favored the inclusion of people who were active on social media. Second, despite the recruitment of more than 1005 respondents, our sample might not be representative: the MD groups came only from Belgium while the PT groups came from Belgium and France. Finally, qualified GPs were not included.
ConclusionThis study found that misconceptions about LBP and the harmfulness of specific movement strategies used by people with a history of LBP or chronic LBP to lift a light load are common among HCPs. Misconceptions were significantly more common in doctors and medical students compared with PTs. Misconception about LBP was negatively influenced by currently experiencing LBP. Moreover, attending a pain education course impacted beliefs positively. These results suggest that targeted education programs are required for PTs and particularly for doctors to improve their understanding of LBP and the effects of movement on LBP.
The authors would like to thank Ms Céline Bugli for reviewing the statistics.