To identify women's complaints about pain in the immediate postpartum of vaginal delivery and cesarean section; to measure the intensity of pain in postpartum women at rest and with selected movements and to compare the activity limitations in relation to the mode of delivery and parity.
MethodObservational, descriptive, cross-sectional study. Eighty-six women, in the immediate postpartum period after vaginal delivery (n=43) and cesarean section (n=43), were evaluated for physical discomforts and their difficulty in performing functional activities.
ResultsAbdominal pain (mean differences=−39.5%; 95% CI=−57.3 to −21.8%), neck pain (mean differences=−16.3%; 95% CI=−32.3 to −0.3%) and edema (mean differences=−41.4%; 95% CI=−63.3 to −20.4%) were reported of cesarean women postpartum. Perineal pain (p<0.05) was reported in vaginal delivery women postpartum. Postpartum pain was more severe during movement after cesarean section (p<0.05) resulting in pain during the activities of sitting down (mean differences=−30.2%; 95% CI=−50.7 to −9.8%), standing up from a sitting position (mean differences=−46.5%; 95% CI=−65.0 to −28.0%), walking (mean differences=−44.2%; 95% CI=−65.2 to −23.1%), lying down (mean differences=−32.6%; 95% CI=−54.9 to −10.3%) and taking a bath (mean differences=−24.0%; 95% CI=−43.1 to −5.0%). Correspondence analysis found no association between parity and functional limitations.
ConclusionThe highest number of complaints was associated with movement activities and cesarean section postpartum. There was no relationship between functional limitations and parity in this study.
The female body changes during the postpartum period returning the different body systems to the pre-pregnancy state as soon as possible. Women should receive special attention during this period because painful conditions may occur that may interfere with functional daily activities during puerperium, and therefore, with their quality of life.
The mode of birth is linked to a woman's recovery time and thus may contribute to functional limitations. Vaginal delivery may result in trauma and perineal discomfort.1 The incision area of a cesarean delivery is a predisposing factor to puerperium morbidity. Parity (i.e., previous births) may also influence puerperal recovery and be connected with pain perception in the postpartum period.2
Brazil's Ministry of Health3 recommends qualified and humanized attention for postpartum women. However, there are discrepancies between the care model of health organizations and clinical reality. The literature relates this discrepancy to a health professional's expertise based on the biomedical model and the ignorance of real needs during the puerperal period.4 Thus, to investigate the influence of the discomforts and functional limitations related to the mode of delivery and parity during the immediate postpartum period, it is important to support physical therapy procedures aimed at preventing and managing women's complaints of pain during this period.
Maternal morbidity may be a temporary or permanent condition, and presents measurement difficulties because the perception of morbidity varies in different cultures.5–7 Furthermore, this condition has a strong link with neonatal7 health, potentiating, for example, a susceptibility factor for unsuccessful breastfeeding.8 Consequently, these complications could result in higher health system due to pain prescription and care for these women.
The puerperal pain has been addressed in the literature but without considering all of its dimensions.4 This practice, commonly observed and widespread in healthcare, directs the therapeutic approach to treatment without giving due importance to the pain complaints of puerperal women. This could mean that the causes of pain are ignored and lead the professional to generalize about individuals and therapies that may help. Moreover, the presence of pain during the puerperium makes it difficult for women to perform the daily activities required during this time period, such as self-care, newborn care, mobility and rest, and may be reflected in physical, psychological and emotional issues.9
The objectives of this study were: (i) to identify women's complaints in the postpartum period of vaginal delivery and cesarean section; (ii) to measure the intensity of pain in postpartum women at rest and during movement, and (iii) to compare the limitations of activities in relation to the mode of delivery and parity.
MethodDesign, setting and participantsThis study was an observational and cross-section study. All current ethical procedures were followed and the study has been approved under protocol number 125,927 by the Ethics Committee of the Universidade Federal de Sao Paulo (UNIFSP), Sao Paulo, SP, Brazil.
Puerperal women aged over 18 years of age, literate, who were between 6 and 24h postpartum, no longer confined to bed, healthy and with single newborns were included in this study. Exclusion criteria were: risk pregnancy, multiple birth pregnancy, and chronic musculoskeletal morbidity prior to pregnancy, puerperal and/or neonatal complications, women who were still confined to bed after delivery, postpartum less than 6h or more than 24h.
The study was conducted in a public maternity ward of a school-hospital on the São Paulo coast of Brazil. Data collection was performed by a single researcher, experienced and trained in performing the physical assessments in the postpartum period. Assessments occurred between November 2012 and June 2013 at different times of the day and on different days of the week.
Data collection proceduresThe women were at least 6h after birth because this was the time when the effect of analgesia used during labor and delivery was expected to have ceased and the mothers were advised to get out of bed. The maximum postpartum period was set at 24h because empirically, it was during this time that some discomfort begins to present itself, such as those connected with the puerperal recovery process, as well as the adoption of asymmetric postures during breastfeeding, newborn care, and positioning on the hospital bed.
The volunteer subjects were first contacted and invited to take part in the study 6–24h after birthing and while still confined to a hospital bed. After agreeing to participate and completing the Informed Consent form, personal data and gestational history was collected. Then, the puerperal women were questioned about the presence or absence of pain in the postpartum period. The reports of pain at rest and with movement were evaluated using a Pain Scale of 11 Points where: zero=no pain; 1–3=mild pain; 4–6=moderate pain; 7–9=severe pain and 10=unbearable pain.9 The body sites of the pain complaints were freely described by the women and categorized by the evaluator. During the assessment, the women were also asked about the presence of pain or discomfort that limited the performance of the activities being investigated in our study.
Only discomfort and pain that began after delivery were considered as the causes of puerperal complaints except for the presence of edema on physical assessment. Edema was considered in our study as related to the circulatory changes that occur after delivery, which may aggravate or trigger the edema formation. The edema evaluation was performed by inspection and application of thumb pressure maintained for 5s on the skin in third distal of both lower limbs (i.e., instep, retromalleolar region, pre-tibial region). The presence of edema was considered clinically positive when the depression forming on skin surface caused by thumb pressure did not disappear immediately after decompressing, i.e., positive Godet sign (pitting edema).10
To verify any functional limitation, the women were asked about the influence of pain when carrying out daily activities in the maternity hospital, related with mobility (i.e., sitting down, standing up from a sitting position, walking and lying down), self-care (i.e., urinating, deficating, taking a bath, feeding and sleeping) and newborn care (i.e., breastfeeding and changing diapers).
Sample calculationPain was considered clinically significant if there was a difference of 2 units (SD=3.1) on the Pain Scale of 11 Points.9 Samples previously collected in a pilot study provided information about the variability of the data. Using these parameters, to have power of 0.80 and a significance level of 0.05, the minimum sample size should be 38 women in each study group (vaginal postpartum group and cesarean postpartum group).
Data analysisThe participants’ characteristics were analyzed using descriptive statistics. To check the difference between the modes of delivery, according to continuous variables (pain at rest and pain during movement), the Student t test for independent samples was used. The association between mode of delivery and the variables of interest (i.e., demographic variables, pain reported, and daily activities of postpartum women) was performed using the chi-square test. To detail the combined behavior of the variables associated with mode of delivery, according to the chi-square test performed previously (mode of delivery, parity, pain when sitting down, pain when standing up from a sitting position, pain when walking, pain when lying down, and pain while taking a bath), a graphic correspondence analysis was performed.
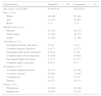
ResultsDuring the period of assessment, 345 postpartum women were present in the maternity hospital. Of these, 86 women met the inclusion criteria, becoming the study sample. Table 1 shows the profile characteristics of participants.
General characteristics of participants.
| Characteristics | Vaginal (n=43) | Cesarean (n=43) |
|---|---|---|
| Age (years), mean (SD) | 25.88 (5.9) | 26.56 (5.2) |
| Race, n (%) | ||
| White | 26 (60) | 21 (49) |
| Dun | 14 (33) | 19 (44) |
| Black | 3 (7) | 3 (7) |
| Marital status, n (%) | ||
| Married | 15 (35) | 16 (37) |
| Stable union | 13 (30) | 16 (37) |
| Single | 15 (35) | 11 (26) |
| Schooling, n (%) | ||
| Incomplete primary education | 5 (12) | 2 (4.7) |
| Complete primary education | 2 (4.7) | 2 (4.7) |
| Incomplete high school education | 4 (9.3) | 7 (16) |
| Complete high school education | 25 (58) | 26 (60) |
| Incomplete higher education | 2 (4.7) | 2 (4.7) |
| Complete higher education | 4 (9.3) | 3 (7) |
| Occupation, n (%) | ||
| Activities outside the home | 16 (37) | 23 (53) |
| Activities at home | 19 (44) | 13 (30) |
| Unemployed | 6 (14) | 5 (12) |
| Student | 2 (4.7) | 2 (4.7) |
| Parity, n (%) | ||
| Primiparous | 18 (42) | 20 (46) |
| Multiparous | 25 (58) | 23 (53) |
SD=standard deviation. n=sample number. %= frequency (percentage).
All cesarean puerperal women (100%, n=43) and 93% (n=40) of vaginal birth puerperal women reported pain in the immediate postpartum period (p=0.24). The reported complaints are shown in Table 2.
Immediate postpartum period complaints of women after vaginal or cesarean section birthing.
| Complaints | Vaginal, n (%) | Cesarean, n (%) | Mean difference (%) | 95% CI | p-Value |
|---|---|---|---|---|---|
| Low back pain | 11 (26) | 12 (28) | −2.3 | −23.4 to 18.7 | 0.99 |
| Abdominal pain | 25 (58) | 42 (98) | −39.5 | −57.3 to −21.8 | <0.05* |
| Neck pain | 2 (4.7) | 9 (21) | −16.3 | −32.3 to −0.3 | 0.05* |
| Lower limbs pain | 5 (12) | 5 (12) | 0.0 | −13.5 to 13.5 | 0.99 |
| Edema | 11 (26) | 29 (67) | −41.9 | −63.3 to −20.4 | <0.05* |
| Perineal pain | 24 (56) | 0 (0) | 55.8 | 38.6 to 73.0 | <0.05* |
| Other | 6 (14) | 10 (23) | −9.3 | −28.0 to 9.4 | 0.40 |
n, sample number; %, frequency (percentage of total sample); 95% CI, confidence interval. Chi-square test.
The abdominal pain variable encompassed cramping and pain following surgical incision. Associations were found between the mode of delivery and abdominal pain, neck pain, edema, and perineal pain. That is, the vaginal delivery postpartum period was associated with perineal pain, while the cesarean postpartum period was associated with abdominal pain, neck pain and edema.
The measurement of pain in the postpartum period was performed both at rest and during movement, considering daily activities. For pain at rest, an average of 1.98 (SD=2.76) was obtained for vaginal delivery postpartum and 1.98 (SD=3.05) for cesarean postpartum (p=0.99), indicating mild pain for both modes of delivery. The pain at movement had a mean of 3.14 (SD=2.54) for vaginal delivery postpartum and 2.06 (SD=2.31) for cesarean section postpartum (p<0.05), indicating mild to moderate pain and moderate to severe pain, respectively. The pain in the postpartum period was more severe during movement in women who had gone through cesarean procedures (Fig. 1).
The analysis of functional activities within the maternity ward indicated that 79% (n=34) of puerperal vaginal delivery women and 98% (n=42) of puerperal cesarean section women had some type of functional limitation (p=0.02). Such tasks were subdivided into: mobility, self-care and newborn care, as shown in Table 3.
Functional limitation by pain in the immediate postpartum period for women after vaginal or cesarean section birthing.
| Activities | Vaginal (n=43) | Cesarean (n=43) | Mean difference (%) | 95% CI | p-Value |
|---|---|---|---|---|---|
| Mobility, n (%) | |||||
| Sitting down | 24 (56) | 37 (86) | −30.2 | −50.7 to −9.8 | <0.05* |
| Standing up from a sitting position | 21 (49) | 41 (95) | −46.5 | −65.0 to −28.0 | <0.05* |
| Walking | 15 (35) | 34 (79) | −44.22 | −65.2 to −23.1 | <0.05* |
| Lying down | 15 (35) | 29 (67) | −32.6 | −54.9 to −10.3 | <0.05* |
| Self-care, n (%) | |||||
| Urinating** | 12 (28) | 14 (36) | −8.0 | −30.6 to 14.6 | 0.59 |
| Evacuating** | 3 (21) | 0 (0) | 21.4 | −16.1 to 59.0 | 0.80 |
| Taking a bath** | 4 (9.3) | 14 (33) | −24.0 | −43.1 to −5.0 | 0.01* |
| Feeding | 5 (12) | 8 (19) | −7.0 | −24.4 to 10.4 | 0.55 |
| Sleeping** | 2 (8.3) | 8 (31) | −22.4 | −47.3 to 2.5 | 0.10 |
| Care of the newborn, n (%) | |||||
| Breastfeeding** | 19 (46) | 21 (49) | −2.5 | −26.2 to 21.2 | 0.99 |
| Changing diapers** | 4 (11) | 9 (31) | −19.9 | −42.8 to 2.9 | 0.09 |
IC 95%, confidence interval; n, sample number; %, frequency (percentage of total sample). Chi-square test.
There was an association between the mode of delivery and the following functional activities: sitting down (p<0.05), standing up from a sitting position (p<0.05), walking (p<0.05), lying down (p<0.05) and taking a bath (p<0.05). To detail the set behavior of these statistically significant variables in relation to the mode of delivery and parity, a correlation analysis was performed which showed that there were two particular patterns strongly characterized by the subjects, as can be seen in Fig. 2.
The identified pattern indicates that puerperal cesarean women felt pain when: sitting down, standing up from a sitting position, lying down and taking a bath, while puerperal vaginal-delivery women did not feel pain when performing the same functional activities. Correspondence analysis showed that the limitation of functional activities was related to the mode of delivery (i.e., vaginal or cesarean section) and not parity (primiparous and multiparous).
DiscussionPain complaints, in the immediate postpartum period during the hospital stay, were made by most of the women in the study. The investigation of the pain and functional limitation of puerperal women, regardless of the mode of delivery and parity, could provide support for the role of the physical therapist.
Abdominal pain, strongly present in cesarean postpartum women, is related to the surgical incision, which involves several layers of tissue that need to go through repair processes, and are thus susceptible to the onset of pain.11,12 However, there are other factors that could also contribute to the onset of pain in the abdominal area immediately postpartum, such as inherent contractions of the uterine involution process and cramping stimulated by breastfeeding,13 use of manipulation during delivery, the presence of gases, and intestinal constipation.14
Neck pain was also a widely reported puerperal complaint in this study. Gestational postural changes and adoption of antalgic postures during labor, delivery and postpartum period, such as positions adopted during breastfeeding15 and newborn care, are some factors that could have influenced the occurrence of the women's complaints.
Edema was found to occur during the cesarean postpartum period, which suggested, as predisposing factors, a longer stay in bed due to the anesthesia recovery period, and the limitation of inherent mobility after surgery.
Pain in the perineal region was reported only by vaginal delivery women, which may be related to episiorrhaphy, which was present in 81.4% of the women. The lack of information in the medical records about the type of episiotomy and any presence of spontaneous lacerations (with or without suture) constituted a limitation of our study since it prevented a more detailed analysis of the cause of perineal pain in puerperal women having a vaginal delivery.
An episiotomy has been described in literature as a triggering factor for complications and morbidity, such as perineal laceration, pain in the perineal region, and dyspareunia.16 A study of postpartum women having a vaginal delivery indicated that pain after perineal trauma restricted the women when sitting down, walking, sleeping and caring for a newborn for up to 72h after delivery,17 suggesting a tendency for the women to continue to complain, and have consequential morbidity, beyond their hospital stay. In a recent Brazilian study,9 drug therapy was reported as the main method of managing women's pain complaints following an episiotomy, with only 23.2% of women in that study reporting pain after perineal trauma, using hot or ice showers for pain relief. This showed that the use of medication for pain was a culturally entrenched clinical practice, contributing to the low use of physical therapy for puerperal care on the maternity ward.
The pain experienced in the postpartum period may restrict the daily activities related to mobility, self-care and newborn care. The puerperal cesarean women were found to have greater functional limitation mainly when performing the activities of mobility and self-care, as they were limited when sitting down, standing up from a sitting position, walking, lying down, and taking a bath. It is important to emphasize that such activities require movements of various body segments, especially the trunk and hips, and movements that have to overcome gravity, which increase the muscle demand to do the activity.
Literature shows that parity may represent a confounding variable in the assessment of pain in the postpartum period. Thus, previous experience from delivery and pain may be considered as modulators of the pain threshold. At same time, multiparity appeared as a risk factor for maintaining the integrity of physical structures, such as the abdominal muscles, which may result in increased report of pain and discomfort.2
Our study showed that the functional limitations were related to the mode of delivery (vaginal or cesarean section) and not parity (primiparous and multiparous). That is, puerperal cesarean women showed a pattern of pain presence for the activities of sitting down, standing up from a sitting position, walking, lying down and taking a bath, regardless of parity, while puerperal vaginal delivery women did not have such limitations.
Another study18 showed that having a cesarean delivery was not a protective factor against the overall morbidity of women throughout the first year following delivery compared with women who had a vaginal delivery. Although our puerperal evaluations were for a period of 6–24h after delivery, it might be expected that there was a tendency to continue the limitation of activities after this time, as well as the occurrence of new discomfort or pain. This reinforces the need for monitoring and physical therapeutic intervention as soon as possible, to relieve pain and improve the women's functionality during this period.
Compared with women who had unassisted vaginal deliveries, the risk of a reduction in health and well-being in the postpartum period is higher among women who have had some kind of unplanned care, such as the use of forceps or emergency cesarean section.19 As for the emotional aspects, the literature indicates a strong relationship between functional incapacity and reduced emotional health in postpartum women,20,21 as well as increased susceptibility to symptoms of depression in puerperal cesarean section women.22
Physical therapy can provide pain management of individuals in different areas of intervention.23 During the postpartum period, physical therapy could aim to reduce pain and discomfort, promotion of the quality of life and morbidity prevention in women and baby health.
Among the main physical therapy resources used for postpartum pain management are: cryotherapy, electrotherapy (especially the use of Transcutaneous Electrical Nerve Stimulation) and kinesiotherapy (which includes early movement and training of the pelvic floor muscles, the abdominal muscles, and respiratory retraining).24 Moreover, low-level laser therapy (LLLT) is a resource that is being increasingly investigated. Recently, LLLT has been reported in scientific literature as beneficial in reducing perineal pain and improving the post-episiotomy wound in puerperium of vaginal delivery.25
Considering the subjectivity and individuality of painful experiences, pain management should be based on investigation of the biological processes, psychological responses, and environmental influence of the pain experience. A physical therapist, working in maternity care as part of a multidisciplinary team, could broaden the process of care of postpartum women.
The current trend observed is that of an increasing number of cesarean births.26 Thus, a corresponding increase in the number of complaints of postpartum pain, and consequently, increasing functional morbidity, may be expected. It is essential that health professionals are able to identify the causes of these complaints and provide the best individual care possible during this period.
Conflicts of interestThe authors declare no conflicts of interest.
This study was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Brazil.