There is insufficient literature on multi-directional hip strength differences and dynamic balance between people with knee osteoarthritis (KOA) and healthy controls.
ObjectiveIn people with unilateral KOA, determine if hip/knee strength and dynamic balance differs (i) between sides, and (ii) compared to controls.
MethodsThirty-six participants (17 women; 65.5 ± 8.9 years) with unilateral KOA and 36 age- and sex-matched controls were included in a cross-sectional study. Outcomes included hip strength, quadriceps strength, and dynamic balance (three directions) during the Star Excursion Balance Test. Mixed ANOVA analysis was completed to investigate differences between Limbs and Groups. Mean differences (MD) and 95% confidence intervals (CI) were calculated.
ResultsQuadriceps and hip adduction strength were 16% (95%CI:10, 22) and 9% [95%CI: 3, 16) lower on the affected compared to non-affected side. Quadriceps and hip abduction, adduction, flexion, and extension strength (MD varying from 16%, 95%CI: 8, 25; to 34%, 95%CI: 17, 50) were weaker bilaterally in individuals with KOA compared to control. Posteromedial balance was 4% (95%CI: 2, 6) lower for affected compared to non-affected limbs in those with KOA and 13% (95%CI: 6, 21) lower in the affected limb compared to controls. Individuals with KOA had lower balance bilaterally in the anterior 11% (95%CI: 7, 15) and posterolateral 21% (95%CI: 13, 30) directions.
ConclusionHip/knee strength (especially in the sagittal and frontal planes) and dynamic balance are lower bilaterally in people with KOA compared to controls. Hip adduction strength is lower on the affected than non-affected limbs of people with KOA. Clinicians should consider that knee extension strength, hip strength, and dynamic balance are lower bilaterally in people with unilateral KOA.
Knee osteoarthritis is characterised by structural joint changes and inflammation of the knee joint.1 Symptoms of pain, stiffness, and instability experienced by people with knee osteoarthritis are often accompanied by functional limitations including reduced mobility and quality of life.1 Eighty per cent of people diagnosed with unilateral knee osteoarthritis develop bilateral symptoms over 12 years.2 People with knee osteoarthritis have impairments in lower limb strength,3,4 neuromuscular control,5 and dynamic balance4 that may contribute to an increased falls risk.6,7
Understanding the ideal type and dose of exercise for greatest benefit in pain, function, and dynamic balance is a priority for people with knee osteoarthritis.8 Literature has demonstrated superior outcomes in short-term pain and function when combining hip and quadriceps exercises compared to quadriceps exercises alone.9 The addition of resistive hip exercises has superior benefits on patient-reported and functional outcomes, whilst the addition of neuromuscular hip exercises to quadriceps exercises is more beneficial for functional outcomes only.9
Clarity in direction-specific impairments may assist with exercise specificity in people with knee osteoarthritis. Hip strength deficits in people with knee osteoarthritis appear to depend on the direction of hip strength testing. Hip abduction strength is 7 to 23% lower in people with knee osteoarthritis than controls.3 There is insufficient evidence of hip adduction strength, and strength in the transverse or sagittal planes.3 Evidence suggests that greater hip abduction strength is associated with a lower risk of symptoms and radiological progression in people with knee osteoarthritis.10,11 However, the relationship between pain experienced with knee osteoarthritis and hip strength is unknown.
Dynamic balance, as measured on a Biodex stability system, is impaired in people with knee osteoarthritis compared to controls and is coupled with a higher risk of falls.12 In asymptomatic people, dynamic balance, as measured with the Star Excursion Balance Test (SEBT), is associated with hip abduction, external rotation, and extension strength.13 The SEBT has been used to assess impairments in dynamic balance in people with anterior cruciate ligament deficiency, chronic low back pain, and chronic ankle instability.14-17 Exercise programs are effective in improving dynamic balance (measured with SEBT) in people with knee osteoarthritis.18 No studies have investigated dynamic balance (measured with SEBT) in people with knee osteoarthritis and compared this with asymptomatic controls.
Understanding differences in hip strength and dynamic balance between limbs in people with unilateral knee osteoarthritis may inform future studies investigating the optimal type of exercise for better patient outcomes. The primary aim of this study was to determine if people with unilateral knee osteoarthritis differ on measures of hip strength, knee strength, and dynamic balance compared to (i) their non-affected limb, and (ii) matched controls. The secondary aim was to determine whether hip strength, knee strength, and dynamic balance are related to pain in people with unilateral knee osteoarthritis.
MethodsThe Prince Charles Hospital and The University of Queensland Human Ethics Committee approved this cross-sectional study (AU/1/98F1312). The study is reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.19
ParticipantsParticipants were recruited through Physiotherapy and Specialist Orthopaedic services at The Prince Charles Hospital and the general community. Volunteers were included in the knee osteoarthritis group if they: (i) were aged 45 years or over;1 (ii) had activity-related knee pain for at least 3 months;1 (iii) had morning knee stiffness lasting no longer than 30 minutes1; (iv) experienced knee pain during most days of the previous month; and (v) rated their knee pain at least 3 out of 10 on a Numeric Pain Rating Scale (NPRS) during aggravating activities.20,21 Participants in the asymptomatic control group had no knee pain and were recruited from the general community. Volunteers were selected for inclusion in the control group to match the knee osteoarthritis sample for age (within 5 years) and sex. Allocation of affected/non-affected limb in the control group was side-matched.
Volunteers for both groups were excluded if they had: (i) a musculoskeletal injury of the back or hip; (ii) knee pain post-trauma; (iii) previous lower limb realignment procedures; (iv) a diagnosed systemic condition; (v) intra-articular corticosteroid injection in the knee or hip within the last 6 months; (vi) oral corticosteroid use within the past 4 weeks; (vii) cognitive deficits that precluded provision of fully informed written consent; or (viii) low competence with written or spoken English.
ProceduresThe study was conducted between August 2018 and March 2020 at The Prince Charles Hospital. All testing was completed by the chief investigator (A.H.) who has more than 15 years of clinical physical therapy experience. Participants’ age, sex, height, and body mass were collected. Femoral and tibial moment arm length for both affected and non-affected limbs was determined (measured from the most prominent point of the greater trochanter to 5cm proximal to the lateral femoral condyle or malleolus, respectively) for the purpose of torque calculations. Patient-reported outcome measures were collected, including usual pain with activity in the past week measured with a NPRS (where 0= no pain at all and 10 = worst possible pain)22 and the Knee injury and Osteoarthritis Outcome Score (KOOS).23
Hip and knee strengthHip and knee extension strength was assessed using a Lafayette (model no. 01165) hand-held dynamometer (HHD) (3700 Sagamore Pkwy N. Indiana, USA) and included hip flexion, abduction, adduction, internal rotation, external rotation, and extension measures. Participants were asked to increase their force against the resistance applied by the investigator (A.H), up to their maximum, then to hold this for 5s before returning to rest. Participants rested for 30s between each test. Each strength test was completed 3 times. A fourth test was completed if one measure appeared inconsistent with the others. The test with the maximum force (N) was then converted to torque (Nm) by multiplying the force (N) by the lever arm distance (m), and reported as body mass normalised torque (Nm/kg).20 Knee extension strength was measured with the participant sitting on a plinth with thighs supported and hands across their chest.24 A seatbelt was used to anchor the HHD to the plinth during testing.24 These measures have been shown to be valid compared to an isokinetic dynamometer in a control population.24
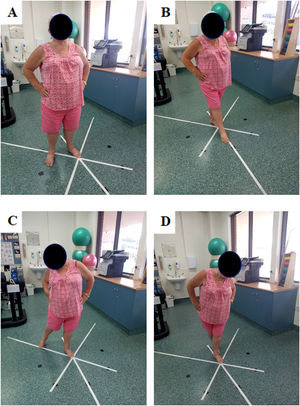
Hip strength order of testing, location of HHD, and participant position are demonstrated in Fig. 1. These tests have previously demonstrated excellent test-retest reliability in people with knee osteoarthritis (intraclass correlation coefficient 0.84–0.98).20
Dynamic balanceDynamic balance was assessed in 3 (anterior, posteromedial, and posterolateral) of the originally described 8 directions of the SEBT (Fig. 2). Reducing the number of reach directions is recommended due to both shared variance between directions and reducing the time necessary to perform the test in people with lower limb injury.25-27 The SEBT has demonstrated excellent test-retest reliability in people with knee osteoarthritis.28 Whilst standing in a comfortable relaxed stance with hands on hips, participants were instructed to “reach as far as possible and tap your big toe on the line as lightly as possible so to avoid using the reach leg for support, then return to the same relaxed stance”.16 Distance reached was recorded by the tester placing a mark on the point reached on the tape. This test was repeated three times for each direction. Tests were discarded if: (ii) the participant did not touch the tape; (ii) pressure was such that the reaching leg was used for support; (iii) the toe slid on the tape; (iv) hands did not remain on hips; or (v) initial relaxed double support stance posture was not regained between trials.28 Unsuccessful trials were repeated until a successful trial was performed. If after 6 attempts no successful trials were performed, this direction was scored as zero. Order of testing limb and direction was randomised, using a random number generator in excel. The best of three attempts in each direction was normalised by leg length.
Statistical analysesStatistical software Jamovi (Version 1.2.27, retrieved from https://www.jamovi.org) was used for data analysis. A score of zero on the dynamic balance test was deemed as a failed test, and this test direction for this participant was removed from analysis. To determine if affected and control cohorts differed in demographics, independent t tests were conducted for continuous variables (age, height, body mass, BMI) and chi-squared tests for the categorical variable (sex). To determine if strength and dynamic balance were dependent on the presence of knee symptoms (affected vs non-affected) or group (knee osteoarthritis or control), a mixed model analysis of variance (ANOVA) was performed. Interactions were followed up with Bonferroni-corrected (p<0.0125) post-hoc paired t-tests (between limbs stratified by group) and independent t-tests (between groups, stratified by limb) to determine where differences existed. If there was no interaction effect, main effects of group and limb were reported. Mean differences (MD) and percentage differences (with 95% CI) were reported for significant post-hoc tests and main effects to provide an estimation of the magnitude of differences. A description of the magnitude of differences was also provided by interpreting Cohen's d effect sizes [≥ 0.2 to 0.50 (small), ≥ 0.50 to 0.80 (medium), ≥ 0.80 (large)]. To evaluate associations between strength and dynamic balance outcomes and patient reported pain (NPRS and KOOS pain subscale) in the knee osteoarthritis group, a multivariable linear regression was conducted, adjusting for age and sex.
ResultsThirty-six participants with unilateral knee osteoarthritis (19 men and 17 women; mean age 65.5 ± 8.9 years) and 36 asymptomatic controls (mean age 65.1 ± 10 years) matched for age and sex were included (Table 1). Participants from the knee osteoarthritis and control groups were similar in age, height, and sex. However, the knee osteoarthritis group on average was 13.4 kg (95%CI: 4.7, 22.1) heavier and had 4.1 kg/m2 (95%CI: 1.3, 7.0) greater BMI than the controls. People with knee osteoarthritis reported significantly lower values on all KOOS subscales, indicating worse pain and symptoms, greater disability, and lower knee-related quality of life than control participants (Table 1). The knee osteoarthritis group reported a mean ± SD usual pain severity during activity of 5.5 ± 1.8, compared to 0/10 for controls.
Participant characteristics.
| Knee osteoarthritis (n = 36) | Healthy controls (n = 36) | Mean difference (95% CI) | |
|---|---|---|---|
| Age, years | 65.5 ± 8.9 (51 to 79) | 65.1 ± 10 (49 to 84) | 0.4 (−5, 4) |
| Number (%) of men | 19 (53) | 19 (53) | |
| Height, cm | 168 ± 7.8 (152 to 185) | 165.9 ± 8 (151 to 179) | 2.1 (−5.8, 1.64) |
| Body mass, kg | 91 ± 19.5 (56 to 129.1) | 76.6 ± 16.8 (44.5 to 133.2) | 13.4 (4.7, 22.1)* |
| Body mass index, kg/m2 | 32.1 ± 7 (21.1 to 43.4) | 28.1 ± 5.7 (17.6 to 45) | 4.1 (1.3, 7.0)* |
| Affected side, left [number (%)] | 17 (47) | matched | |
| Pain NRS (0–10) | 5.5 ± 1.8 (3 to 8) | 0 | – |
| KOOS (0–100): | |||
| Pain | 53.3 ± 14.0 (22.2 to 77.8) | 96.7 ± 14.0 (55.6 to 100) | 33.8 (27.5, 41.0)* |
| Symptoms | 57.6 ± 14.9 (25 to 82.1) | 92.6 ± 14.9 (50 to 100) | 25.0 (18.5, 31.5)* |
| ADL function | 61.4 ± 14.2 (29.4 to 88.2) | 96.9 ± 5.9 (60.3 to 100) | 25.5 (19.3, 31.7)* |
| Sport/recreation function | 29.2 ± 19.6 (0 to 80) | 92.2 ± 10.3 (45 to 100) | 55.4 (46.8, 64.1)* |
| Quality of life | 34.4 ± 17.5 (0 to 62.5) | 90.6 ± 13.5 (37.5 to 100) | 46.7 (38.7, 54.7)* |
| Patellofemoral | 35.5 ± 16.1 (5 to 65) | 95.8 ± 7.8 (50 to 100) | 51.3 (44.3, 58.3)* |
Data presented as mean ± SD (range) unless otherwise stated.
NRS, numerical rating scale; KOOS, Knee injury and Osteoarthritis Outcome Score; ADL, activities of daily living.
There was a significant interaction between Limb (affected vs non-affected [and matched limb for controls]) and Group (knee osteoarthritis or control) for knee extension strength (p<0.001) and hip adduction strength (p<0.01) (Table 2, Supplementary material – Fig. S.1).
Strength and dynamic balance measures for people with knee osteoarthritis and control participants.
| Task | Group | Limb | Within Group | Within Group | Within Group | |||
|---|---|---|---|---|---|---|---|---|
| Affected | Non-affected | Mean difference | Percentage difference | Effect size | ||||
| (95% CI) | (95% CI) | (95% CI) | ||||||
| Weight normalised strength measures (Nm/kg) | ||||||||
| Knee Extensiona | Knee OA | 1.02 ± 0.43 | 1.21 ± 0.46 | 0.19 (0.12, 0.26) | 15.7 (9.9, 21.5) | 0.92 (0.52, 1.31) | ||
| Control | 1.49 ± 0.44 | 1.47 ± 0.41 | 0.02 (−0.11, 0.14) | 1.3 (−7.4, 9.5) | 0.11 (−0.21, 0.44) | |||
| Hip flexionb | Knee OA | 0.84 ± 0.28 | 0.83 ± 0.27 | −0.01 (−0.04, 0.02) | 1.2 (−4.8, 2.4) | −0.12 (−0.45, 0.21) | ||
| Control | 0.98 ± 0.23 | 1.01 ± 0.26 | 0.02 (−0.03, 0.09) | 2.0 (−3.0, 8.9) | −0.22 (−0.55, 0.11) | |||
| Hip abductionb | Knee OA | 0.82 ± 0.4 | 0.86 ± 0.4 | 0.04 (0.01, 0.07) | 4.7 (1.2, 8.1) | 0.43 (0.9, 0.78) | ||
| Control | 1.1 ± 0.31 | 1.12 ± 0.32 | 0.03 (−0.04, 0.11) | 2.7 (−4.5, 12.3) | −0.05 (−0.37, 0.28) | |||
| Hip adductionb | Knee OA | 0.67 ± 0.4 | 0.75 ± 0.42 | 0.07 (0.02, 0.12) | 9.3 (2.7, 16.0) | 0.38 (0.05, 0.71) | ||
| Control | 1.02 ± 0.3 | 1.01 ± 0.31 | 0.03 (−0.06, 0.12) | 3.0 (−6.0, 12.0) | 0.09 (−0.24, 0.42) | |||
| Hip internal rotation | Knee OA | 0.06 ± 0.02 | 0.07 ± 0.03 | 0.01 (−0.00, 0.01) | 8.5 (−0.0, 14.3) | 0.32 (−0.02, 0.65) | ||
| Control | 0.06 ± 0.02 | 0.07 ± 0.02 | 0.00 (−0.00, 0.01) | 2.8 (−5.7, 1.14) | −0.13 (−0.46, 0.20) | |||
| Hip externalc rotation | Knee OA | 0.4 ± 0.17 | 0.42 ± 0.16 | 0.03 (0.01, 0.06) | 7.1 (2.4, 14.3) | 0.41 (0.07, 0.75) | ||
| Control | 0.46 ± 0.18 | 0.48 ± 0.15 | 0.02 (−0.03, 0.07) | 1.9 (−6.3, 14.6) | −0.17 (−0.46, 0.20) | |||
| Hip extensionb | Knee OA | 0.88 ± 0.35 | 0.88 ± 0.37 | 0.01 (−0.03, 0.05) | 1.1 (−3.4, 5.7) | 0.06 (−0.27, 0.39) | ||
| Control | 1.13 ± 0.28 | 1.13 ± 0.28 | 0.03 (−0.05, 0.12) | 2.7 (−4.4, 10.6) | 0.00 (−0.32, 0.33) | |||
| Leg length normalised balance measures (% of leg length) | ||||||||
| Anteriorb | Knee OA | 0.76 ± 0.12 | 0.78 ± 0.11 | 0.02 (−0.00, 0.04) | 2.6 (−0.6, 4.9) | 0.27 (−0.07, 0.61) | ||
| Control | 0.9 ± 0.14 | 0.89 ± 0.14 | 0.00 (−0.01, 0.01) | 0.3 (−1.1, 1.1) | 0.06 (−0.26, 0.39) | |||
| Posteromediala | Knee OA | 1.02 ± 0.18 | 1.07 ± 0.17 | 0.04 (0.02, 0.06) | 3.7 (1.9, 5.6) | 0.65 (0.28, 1.01) | ||
| Control | 1.18 ± 0.21 | 1.17 ± 0.19 | 0.02 (−0.01, 0.04) | 1.7 (−0.9, 3.4) | 0.24 (−0.09, 0.57) | |||
| Posterolaterala | Knee OA | 0.78 ± 0.19 | 0.82 ± 0.2 | 0.04 (−0.01, 0.07) | 4.9 (−1.2, 8.5) | 0.27 (−0.07, 0.61) | ||
| Control | 1.0 ± 0.17 | 0.96 ± 0.19 | 0.04 (0.01, 0.07) | 4.2 (1.0, 7.3) | 0.40 (0.06, 0.74) | |||
Values are mean ± SD unless otherwise indicated. OA, osteoarthritis.
Post-hoc within-group comparisons between Limbs indicated that the strength of the knee extensors and hip adductors were 15.7% (95%CI: 9.9, 21.5) and 9.3% (95%CI: 2.7, 16.0) lower, respectively, in the affected than non-affected limb of people with knee osteoarthritis (medium and small effect, respectively). There was no significant difference in knee extension or hip adduction strength between limbs in controls. Post-hoc comparisons between Groups, stratified by Limb, indicate that knee extension and hip adduction strength were 31.5% (95%CI: 17.9, 45.3) and 33.3% (95%CI: 17.3, 50.0) lower (large effect), respectively, in the affected limb of knee osteoarthritis participants; and 17.6% (95%CI: 3.2, 32.0) and 25.6% (95%CI: 8.4, 42.7) lower (medium effect), respectively, in the non-affected limb of knee osteoarthritis participants compared to controls.
For strength directions with no interaction effects, main effects of Group indicate that strength was 24.3% (95%CI: 13.6, 35.1), 16.4% (95%CI: 7.9, 25.1) and 22.1% (95%CI: 12.7, 31.8) lower bilaterally in the hip abduction, flexion, and extension directions, respectively, for people with knee osteoarthritis compared with controls (medium effect) (Table 2). There were no significant main effects of Limb for any knee or hip strength measures.
The relationship between hip and knee strength and patient reported pain (NPRS and KOOS-pain) in people with knee osteoarthritis is presented in Table 3 and Supplementary material – Fig. S.2. A significant 62% (p<0.01) of the variance in knee extension strength can be explained by KOOS-pain score, when also adjusted for age and sex (Table 3, Supplementary material – Fig. S.2). There was no significant linear relationship between hip strength and KOOS-pain in people with knee osteoarthritis (r< 0.45; p>0.06).
Strength, dynamic balance, Numerical Pain Rating Scale, and Knee Injury and Osteoarthritis Outcome Score – pain subscale multi-linear regression analyses.
| NPRS | KOOS-PS | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Sex | Age | Adj. R2 | Sex | Age | Adj. R2 | ||||
| Strength | |||||||||
| Knee | Extension* | −0.08* (−0.13,−0.02) | .51* (0.32, 0.69) | −0.01* (−0.03,−0.003) | 0.59 | 0.01* (0.004, 0.02) | 0.53* (0.35, 0.72) | −0.0195* (−0.03, −0.01) | 0.62 |
| Hip | Flexion | −0.04 (−0.08, 0.009) | .24* (0.09, 0.39) | −0.01* (−0.02, −0.002) | 0.37 | .004 (−0.002, 0.01) | .25* (0.09, 0.4) | −0.013* (−0.02 to −0.004) | 0.36 |
| Abduction | −0.06 (−0.13, 0.01) | .37* (0.15, 0.59) | −0.01 (−0.02,.003) | 0.34 | .007 (−0.002, 0.02) | 0.39* (0.16, 0.62) | −0.014* (−0.03, −0.001) | 0.33 | |
| Adduction | −0.05 (−0.12, 0.02) | .36* (0.13, 0.58) | −0.01 (−0.02, 0.002) | 0.32 | 0.0078 (−5.37×104, 0.017) | 0.38* (0.16, 0.60) | −0.015* (−0.03, −0.002) | 0.34 | |
| Internal rotation | −0.002 (−0.01, 0.002) | .02* (0.004, 0.03) | −0.001* (−0.002, −4 × 104) | 0.35 | 1.19×106 (2.28×104, −4.63×104) | 0.02* (0.004,0.03) | −0.001* (−0.002, −4.23×104) | 0.34 | |
| External rotation | −0.01 (−0.04, 0.02) | .19* (0.10, 0.28) | −0.005 (−0.01, 4 × 104) | 0.39 | 0.002 (−9.5 × 104, 0.006) | 0.19* (0.1, 0.28) | −0.006* (−0.01, −7.16×104) | 0.42 | |
| Extension | .04 (−0.1, 0.02) | .3* (0.11, 0.50) | −0.01* (−0.02, −0.002) | 0.34 | 0.006 (−0.002, 0.013) | 0.32* (0.12, 0.51) | −0.016 (−0.03,.005) | 0.35 | |
| Dynamic balance | |||||||||
| Anterior | −0.02 (−0.04, 0.01) | .06 (−0.01, 0.13) | −0.005* (−0.009, −4 × 104) | 0.23 | 0.002 (−6.05×10−4, 0.005) | 0.07 (−0.004, 0.14) | −0.005* (−0.01, −0.0016) | 0.24 | |
| Posteromedial | .01 (−0.04, 0.03) | 0.01 (−0.1, 0.12) | −0.01* (−0.02, −0.004) | 0.24 | 0.002 (−0.002, 0.006) | 0.02 (−0.09, 0.13) | −0.12* (−0.18, −0.006) | 0.27 | |
| Posterolateral | −0.04* (−0.08, −0.01) | .07 (−0.05, 0.20) | −0.002 (−0.01, 0.01) | .13 | 0.005* (1.61×10−4, 0.01) | 0.086 (−0.04, 0.21) | −0.005 (−0.01, 0.003) | 0.10 | |
NPRS, Numerical Pain Rating Scale. KOOS-PS, Knee injury and Osteoarthritis Outcome Score pain subscale. * p <0.05.
Two 79-year-old female participants in the knee osteoarthritis group failed at least one reach direction on the SEBT. One of them failed all 3 reach directions with both affected and non-affected limbs. The other failed the posterolateral reach direction with both limbs. There was a significant interaction between Limb and Group for posteromedial (p<0.01) and posterolateral (p<0.01) dynamic balance directions (Table 2, Supplementary material - Fig. S.1). Posteromedial dynamic balance was 3.9% (95%CI: 1.8, 5.9) lower when people with knee osteoarthritis stood on the affected limb compared to their non-affected limb (medium effect). Difference in posterolateral dynamic balance between limbs in people with knee osteoarthritis was not statistically significant (MD= 4.9%, 95%CI: −1.2, 8.5. There were no significant differences in posteromedial or posterolateral dynamic balance between limbs in controls. In people with knee osteoarthritis, posterolateral and posteromedial dynamic balance was 21.0% (95%CI: 12.6, 29.8) and 13.6% (95%CI: 5.6, 21.5) lower, respectively, whilst standing on the affected limb (large effect), and posterolateral dynamic balance was 15.0% (95%CI: 5.4, 24.7) lower whilst standing on the non-affected limb (medium effect), compared to controls. An 8.5% (95%CI: 1.1, 15.9) difference in posteromedial dynamic balance between the non-affected limb of the knee osteoarthritis group and control limb of the healthy group did not meet significance after Bonferroni correction (p = 0.02). Anterior dynamic balance was 13.8% (95%CI: 9.2, 18.5) lower in people with knee osteoarthritis, compared to controls, irrespective of Limb (large effect). There was no main effect of Limb (p = 0.27) on dynamic balance in the anterior direction.
The relationship between dynamic balance and pain in the affected limb of people with unilateral knee osteoarthritis is described in Table 3 and Supplementary material – Fig. S.2. NPRS and KOOS-pain were significant variants (p<0.05) when modelled with age and sex for posterolateral dynamic balance, however the regression models themselves did not meet significance (adj.R2= 0.14, p = 0.06 and adj.R2 = 0.1, p = 0.10, respectively). NPRS and KOOS-pain were not significant when modelled with age and sex variables for anterior or posteromedial dynamic balance.
DiscussionThis study demonstrates that people with unilateral knee osteoarthritis have lower knee extension and hip adduction strength in the affected than non-affected limb. People with unilateral knee osteoarthritis also have bilateral deficits in knee extension strength, hip strength (abduction, adduction, flexion, and extension) and dynamic balance (anterior, posteromedial, and posterolateral) compared to matched controls. When adjusted for age and sex, KOOS-pain explains 62% of the variance in knee extension strength, and KOOS-pain and NPRS explain 14% and 10% respectively, of the variance in posterolateral dynamic balance of the affected limb. Pain severity is not associated with hip strength in any direction or dynamic balance in the anterior or posteromedial directions.
Strength asymmetries may exist due to limb dominance,29 unilateral pathology,30 and older age.31,32 Knee extension strength asymmetry in the older population has been estimated at 15–20%, and more than 10% asymmetry in older females may be predictive of falls.31,32 Targeting strength symmetry through unilateral exercise may be beneficial in reducing falls risk in the older population.33 Knee extension strength asymmetry of 15.7% (95% CI: 9.9, 21.5) identified in this study may be a therapeutic target to reduce falls risk in people with unilateral knee osteoarthritis. The relevance of a 9.3% (95% CI: 2.7, 16.0) asymmetry between affected and non-affected limbs to functional performance in people with unilateral knee osteoarthritis should be further investigated.
This study confirms previous work that found lower hip strength in the frontal and sagittal planes of people with knee osteoarthritis compared to asymptomatic controls.20 We found that differences were greatest in the frontal plane compared to sagittal or transverse planes. The lower hip abduction strength demonstrated in this study (24.3% [95%CI: 13.6, 35.1]), supports a previous systematic review demonstrating that hip abduction strength in people with knee osteoarthritis is 7 to 23% lower than controls.3 Our study also confirms that people with knee osteoarthritis have lower hip adduction strength compared to controls.9
In contrast to prior research, we did not find significantly lower strength in the transverse plane in people with knee osteoarthritis compared to controls.20 The discrepancy between these studies could be related to the position of testing. In our study, hip rotation strength was assessed with the hip in an extended position, the same position as for regular functional tasks like walking, in contrast to 90° hip flexion.20 It is plausible that the hip testing position could alter the lever arm and/or recruitment of various hip rotators or their relative segments. For example, the deep hip rotators and the anterior segment of gluteus minimus and medius have increasing activity with greater hip flexion.34-36
We have demonstrated comparable deficits in knee extension and hip adduction strength in the affected (31.5% and 33.3% respectively) and non-affected (17.6% and 25.6% respectively) limbs of people with unilateral knee osteoarthritis compared to asymptomatic controls. Our findings in people with moderate to severe knee osteoarthritis symptoms contrasts those of people with mild to moderate unilateral symptoms, who demonstrate no difference between affected and non-affected limbs in knee extension or hip adduction strength (Nm/kg).37 The difference in outcomes between studies may provide evidence that knee extension and hip adduction strength reductions in the affected limb coincide with symptom progression. Previous research has demonstrated that unilateral pain is associated with gait asymmetries, including greater varus angle and lower external flexion moment in the painful knee.38 The asymmetries in knee extension and adduction strength observed in this study may reflect these unilateral changes in knee biomechanics.
In addition to knee extension and hip adduction strength differences, people with unilateral knee osteoarthritis also display lower hip abduction (24.4%), flexion (16.5%), and extension (22.1%) strength bilaterally. This is important because greater knee extension and hip abduction strength have been shown to have a protective effect against the development of symptoms and structural progression, respectively.10,39 When identifying patient impairments clinicians should consider that hip and knee strength differences are bilateral in people with unilateral knee osteoarthritis.
There is some evidence that a gain of at least 30% in knee extension strength and the addition of a resistive type hip strengthening program to quadriceps strengthening is required for consistent benefits across pain and disability for people with knee osteoarthritis.9,40 However this has only been demonstrated in the short-term, with longer term follow up needed to determine long term benefits for such rehabilitation strategies. Future clinical trials should investigate the effect of high-intensity bilateral hip resistance strengthening and the associated benefits on pain, function, dynamic balance, risk of falls, and the potential for prevention of developing bilateral affected knee osteoarthritis. Hand-held dynamometry may also be used to improve adherence to these exercise programs.
There are likely to be multiple factors contributing to the bilateral deficits in dynamic balance [affected limb range (13.6% to 21.1%), non-affected limb range (8.5% to 14.6%)] that were observed in all three directions in people with unilateral knee osteoarthritis compared to controls. Greater dynamic balance is associated with higher hip strength in controls.13 Therefore, it is plausible that lower hip strength that we observed in both limbs of participants with unilateral knee osteoarthritis may contribute to observed deficits in bilateral dynamic balance. Due to the presence of bilateral deficits in dynamic balance and patient-reported pain not contributing to these differences, factors other than pain must affect dynamic balance in people with unilateral knee osteoarthritis.
The two oldest participants in the knee osteoarthritis group failed at least one SEBT attempt, whereas those older participants in the asymptomatic group were able to complete all dynamic balance attempts successfully. Our findings supports other studies that have demonstrated that whilst ageing results in neuromuscular changes, even greater neuromuscular deficits that contribute to dynamic balance and increased risk of falls are seen in people with knee osteoarthritis.6,41 Exercise programs have been shown to improve dynamic balance in people with medial knee osteoarthritis.18 Clinicians should consider the role of bilateral strengthening programs for people with unilateral knee osteoarthritis to address bilateral dynamic balance impairments that are known to be associated with increased falls risk.42
The limitations of this study include its cross-sectional design. It should be considered an exploratory study in nature as it may be underpowered to measure multiple strength outcomes. Whilst previously reported reliability data has been adapted by this study,20 the specific methods of reliability testing are not available for peer review. The study design is unable to demonstrate causality between lower limb strength, dynamic balance, and the presence of knee osteoarthritis. The generalizability of this study is also a limitation. Participants were recruited from referrals to orthopaedic specialist services in a public health facility to consider knee arthroplasty and therefore may not be representative of the general population. Further clinical trials need to be conducted to investigate if identifying bilateral and multi-directional hip strength and tailoring interventions accordingly leads to greater patient benefits.
ConclusionCompared to age and sex-matched asymptomatic controls, people with unilateral knee osteoarthritis have lower knee extension and hip strength, especially in the frontal and sagittal planes, and dynamic balance. While bilateral strength and balance deficits are present in those with unilateral knee osteoarthritis, hip adduction strength is significantly lower in the affected limb than their non-affected limb. Patient-reported pain is associated with knee extension strength but not hip strength or dynamic balance. When assessing individual patient impairments, clinicians should consider that changes in knee extension strength, hip strength and dynamic balance are bilateral in people with unilateral knee osteoarthritis.
This work was supported by the Common Good, The Prince Charles Hospital Foundation (EM2019-04, 2019)