Subtalar hyperpronation and ankle dorsiflexion restriction have been theoretically associated with Achilles tendinopathy (AT). However, evidence to support these associations is lacking.
ObjectivesTo compare foot alignment and ankle dorsiflexion range of motion (ROM) between the symptomatic and non-symptomatic limbs of individuals with unilateral AT. And to verify whether differences exist between individuals with symptomatic pronated feet and individuals with symptomatic neutral/supinated feet in terms of tendon pain, structure, and symptom severity.
MethodsSixty-three participants with unilateral AT underwent a bilateral evaluation of pain during tendon palpation, symptom severity, tendon thickening, tendon neovascularization, ankle dorsiflexion ROM, and foot posture alignment [foot posture index (FPI), navicular drop, navicular drift, and longitudinal arch angle (LAA)]. Side and group comparisons were made using t-tests and correlations were evaluated using the Pearson test.
ResultsThere were no differences between the symptomatic and non-symptomatic limbs regarding foot posture alignment. Specifically, non-significant negligible differences were observed between limbs regarding FPI [mean difference (MD)=-0.23; 95% confidence interval (CI)=-0.70, 0.25), navicular drop (MD=0.58 mm; 95%CI=-0.25, 1.43), navicular drift (MD=0.16 mm; 95%CI=-0.77, 1.09), and LAA (MD=0.30º; 95%CI=-1.74, 2.34). There was no difference between limbs regarding ankle dorsiflexion ROM. However, lower ankle dorsiflexion was associated with worse symptom severity (r = 0.223). Finally, no difference was observed between individuals with symptomatic pronated feet and individuals with symptomatic neutral/supinated feet in terms of tendon pain or structure.
ConclusionsStatic foot alignment measures do not seem to be clinically relevant in patients with AT. Smaller ankle dorsiflexion ROM, however, was associated with greater symptom severity in this population.
Achilles tendinopathy (AT) is a prevalent overuse injury.1 It is characterized by localized Achilles tendon pain, impaired physical function, tendon thickening and, in more chronic cases, neovascularization.2 It can lead to significant disability and a substantial amount of patients develop persisting symptoms that can last for years.3,4 This highlights the importance of studies to better understand the factors associated with this condition. The etiology of AT is considered multifactorial, with both intrinsic and extrinsic factors contributing to the development of tendon overload.5
Excessive subtalar joint pronation has been suggested to be an important factor associated with the etiology of AT in classical theoretical studies.6-8 It has been suggested that excessive subtalar pronation (overpronation) would cause a “whipping phenomenon” or “bowstring effect” in the Achilles tendon, promoting microtrauma with possible vascular blanching within the tendon.7 Supporting this assumption, a few cross-sectional studies have observed that individuals with AT have greater subtalar pronation than healthy controls during running.9,10 Recent research has proposed that AT is a “pronation-related injury”,11 and clinical tests to identify static subtalar pronation have been recommended for rehabilitation and prevention of this condition.12 However, evidence actually supporting an association between AT and foot misalignments is not strong.13 This has led the authors of the recent clinical practice guidelines on management of AT to not include overpronation as a risk factor for AT.5,14 In addition, two recent prospective studies have shown that foot misalignments, as measured by the foot posture index, are not risk factors for the development of AT.15,16 Considering the inconsistencies in the literature looking into the association of foot misalignments and AT, more studies are necessary to see whether excessive subtalar pronation is associated with the domains of tendon health in patients with AT.
Decreased ankle dorsiflexion range of motion has also been suggested as a potential etiological factor associated with AT.7,12,17-19 Restricted dorsiflexion range of motion may increase the tension on the Achilles tendon during weight-bearing activities, thereby increasing the risk of tendinopathy.12 Conversely, a few studies have observed that individuals with AT have greater ankle dorsiflexion range of motion compared to healthy controls9,20 and one study found no difference in ankle dorsiflexion range of motion between individuals with and without AT.21 Therefore, the exact association between ankle dorsiflexion range of motion and Achilles tendinopathy remains uncertain.
Considering the potential effects of excessive subtalar joint pronation in Achilles tendon mechanics, it is possible that this foot misalignment significantly influences tendon pain, symptom severity, and tendon structure in individuals with AT. However, to our knowledge, no study looked into the association between foot misalignments and tendon pain, symptom severity, and tendon structure in individuals with AT. The purpose of this study was to compare foot alignment and ankle dorsiflexion range of motion between the symptomatic and non-symptomatic limbs of individuals with unilateral AT. A secondary aim was to verify whether differences exist between individuals with symptomatic pronated feet and individuals with symptomatic neutral/supinated feet in terms of tendon pain and structure, symptom severity, and ankle range of motion. Finally, we aimed to verify whether relationships exist between foot alignment and ankle range of motion and pain, symptom severity, and tendon structure in individuals with AT.
MethodsParticipantsSixty-three individuals with unilateral midportion AT (33 male) participated in this study. Participants were part of a larger longitudinal study comparing the effect of exercise as treatment for men and women with midportion AT. Data were collected bilaterally at baseline, prior to treatment initiation. Participants were included if they were between the ages of 18 and 65 years old and presented with a clinical diagnosis of midportion AT. Clinical diagnosis was established by pain on palpation of the midportion of the Achilles tendon and report of Achilles tendon pain with loading.22 Exclusion criteria were previous history of Achilles tendon rupture or another injury limiting the ability to perform required tests.23 Participants were recruited from local clinics and by means of advertisements. The study setting was the University of Delaware Physical Therapy Clinic and measurements were made by researchers with over 5 years of experience with these measurements following strict standard operating procedures. All participants signed an informed consent form and protocols were approved by the Institutional Review Board at University of Delaware.
Sample size calculations were conducted using data from previous studies.24,5 Foot posture index was considered the primary outcome for the main objective of the study and the calculation used α=0.05, β=0.80, a mean difference of 2.3 points and an effect size of 0.71.24 Thirty-three participants were found to be needed for the study to be adequately powered. A second calculation was conducted using the Victorian Institute of Sport Assessment-Achilles (VISA-A) questionnaire score as the primary outcome for the secondary aim of the study. For this calculation, the parameters that were used were α=0.05, β=0.80, a mean difference of 12 points and an effect size of 0.80.25 With this calculation, it was observed that 52 participants would be needed, twenty-six in each group.
ProceduresParticipants were initially assessed with regards to pain with palpation and symptom severity, bilaterally. Then they underwent a bilateral Achilles tendon ultrasound imaging evaluation by an experienced researcher, as described below. Foot posture alignment and ankle dorsiflexion range of motion assessments were conducted by a different researcher who was blind to which of the participant's limbs was the symptomatic side. This was a strategy to minimize bias during these assessments. In addition, before the beginning of the study, the involved researchers underwent weeks of training with the standard operating procedures for the outcome measures, also as a strategy to minimize bias.
Outcome measuresSymptoms
Pain with palpation of the midportion of both Achilles tendons was recorded using the numerical pain rating scale (NPRS) from 0 (no pain) to 10 (worst pain imaginable).26 The VISA-A was used to measure symptom severity in both limbs.27 VISA-A is an eight-question measurement tool that has good validity and reproducibility.28 Scores range from 0 to 100 with lower values indicating greater disability.27
Ultrasound imagingUltrasound images were taken using a LOGIQ E ultrasound system (GE Healthcare, Chicago, IL, USA) with brightness mode ultrasound (10 MHz). Three extended field images were taken bilaterally from the distal Achilles tendon insertion on the calcaneus to the musculoskeletal junction between the Achilles tendon and the soleus.29 Power doppler was used to assess for presence of neovascularization along the length of the Achilles tendon.30 Presence or absence of neovascularization was used for data analysis. Tendon thickness was measured at 2 cm proximal to the calcaneal notch and at the thickest portion of the tendon. Tendon thickening was defined as the difference between the measurement of width at the thickest portion minus the width at 2 cm proximal to calcaneal notch.29,31 The average of three trials at each location were used for analyses. Previous research has shown that this measure has high reliability [intraclass correlation coefficient (ICC3,3) = 0.898; standard error of measurement (SEM) = 0.01 cm].29
Foot posture alignmentFoot posture alignment was evaluated bilaterally using clinician-friendly static alignment measuring tools. Specifically, the alignment of both feet of all participants were evaluated using the foot posture index,32 longitudinal arch angle,33 navicular drop, and navicular drift.24,34
Foot posture index (FPI) is a six-item observation tool measuring foot alignment in bilateral standing.32 Each of the six items are measured from −2 to +2. Total scores range from −12 (highly supinated) to +12 (highly pronated). The six measures include talar head palpation, curves above and below the malleoli, calcaneal inversion/eversion, medial arch height, talo-navicular congruence, and forefoot abduction/adduction as previously described.32 Measures were taken with the participants standing in a comfortable position with their arms by their sides and looking straight ahead. Previous literature has described the FPI as a reliable tool (ICC2,1 = 0.92‒0.98).24
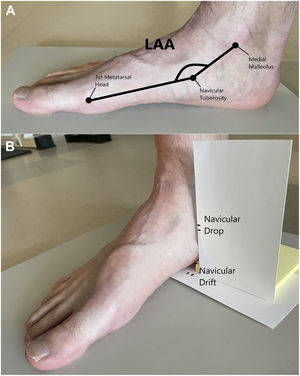
Longitudinal arch angle measures the angle between the line from the center of the medial malleolus to the navicular tuberosity and the line from the first metatarsal head and the navicular tuberosity (Fig. 1a).33,34 The angle was calculated using a plastic goniometer in weight-bearing and reported in degrees. This measurement has been shown to be reliable in previous research (ICC2,1 = 0.74‒0.81).24
Navicular drop measures the vertical displacement of the navicular tuberosity when an individual goes from subtalar joint neutral to relaxed weight-bearing.24,34 For this measurement, participants were placed in subtalar neutral in a seated position and the height of their navicular tuberosity was marked on an index card. The participants then stood, and the new height of the navicular tuberosity was marked on the same card. The distance between the two marks was measured and recorded in millimeters (Fig. 1b).24 Navicular drift measures the medial displacement of the navicular tuberosity when an individual goes from subtalar joint neutral to relaxed weight-bearing. For this measurement, participants were placed in subtalar neutral in a seated position and the position of their navicular tuberosity was marked on an index card flat on the floor. The participants then stood, and the new position of the navicular tuberosity was marked on the same card. The distance between the two marks was also measured and recorded in millimeters (Fig. 1b).24 Good to excellent reliability has been reported for the measurement of navicular drop (ICC2,1 = 0.88‒0.95) and navicular drift (ICC2,1 = 0.92‒0.95).24
Dorsiflexion range of motionWeight-bearing ankle dorsiflexion range of motion was evaluated in a knee extended and knee flexed positions.35,36 For these measurements, participants stood in a split stance with the trailing limb being the limb of interest. They were instructed to lunge forward as far as possible while maintaining knee extension and keeping their heel on the floor. A digital inclinometer was placed on the mid tibial shaft and degrees of dorsiflexion range of motion was recorded at the point just before the heel starts to rise. To obtain weight-bearing ankle dorsiflexion range of motion with the knee flexed, the participants were instructed to bend their knee and lunge forward as far as possible while maintaining knee flexion and keeping their heel on the floor. Degrees of dorsiflexion range of motion were recorded at the point just before the heel starts to rise from the ground. High reliability has been reported for weight-bearing ankle dorsiflexion with knee extended (ICC2,4 = 0.95)36 and knee flexed (ICC2,3 = 0.89‒0.99).35 Due to problems with data entry into the database, the results of 11 participants were unable to be used in data analysis, with the results of 52 participants being used in the analysis of ankle dorsiflexion range of motion measurements.
Data processing and statistical analysisAll data were collected and managed using the Research Electronic Data Capture (REDCap) tool. REDCap is a web-based software platform that allows secure data registry and allows audit trails for tracing data manipulation and export procedures.37,38 Statistical analysis was performed using IBM SPSS Statistics (version 28.0, SPSS, Chicago, Illinois). Demographics were reported descriptively. The Shapiro-Wilk test was used to verify statistical distribution. Paired t-tests were used to compare the symptomatic limb in relation to the non-symptomatic limb with regards to pain during palpation, symptom severity, foot posture alignment, and tendon structure. For comparisons between individuals with pronated symptomatic limbs (foot posture index≥6) and individuals with neutral/supinated symptomatic limbs (foot posture index<6) with regards to the same variables, independent t-tests were used. Mean differences and 95% confidence intervals were calculated to determine the meaningfulness of the observed differences. Finally, correlations between measures were evaluated using the Pearson correlation test. The r values for correlation were interpreted as follows: 0.00‒0.19=none to slight, 0.20‒0.39=low, 0.40‒0.69=modest, 0.70‒0.89=high, and 0.90‒1.00=very high.39 For all analyses, a significance level of P<.05 was used.
ResultsThe mean age and body mass index of the included participants (n = 63) were 47.65 ± 12.8 years and 29.09 ± 5.5 kg/m2, respectively. As expected, there was a significant difference between the symptomatic and non-symptomatic limbs with regards to pain during tendon palpation [mean difference (MD)=3.7; 95% confidence interval (CI)=3.10, 4.30], symptom severity (MD=−38.62; 95%CI=−42.79, −34.44), and tendon thickening (MD=0.15 cm; 95%CI=0.10, 0.20). Neovessels were present in 27 of 63 symptomatic limbs and in 3 of 63 non-symptomatic limbs (MD=38%; 95%CI=24.8, 51.4). However, there were no differences between the symptomatic and non-symptomatic limbs with regards to foot posture alignment or ankle dorsiflexion range of motion (P>.05; Table 1). Specifically, negligible differences were observed between limbs regarding foot posture index (MD=−0.23; 95%CI=−0.70, 0.25), navicular drop (MD=0.58 mm; 95%CI=−0.25, 1.43), navicular drift (MD=0.16 mm; 95%CI=−0.77, 1.09), longitudinal arch angle (MD=0.30º; 95%CI=−1.74, 2.34), ankle dorsiflexion with the knee extended (MD=0.21º; 95% CI=−1.32, 0.90) and ankle dorsiflexion with the knee flexed (MD=0.81º; 95%CI=−2.15, 0.54) (Table 1).
Foot alignment, tendon structure, pain, and symptom severity in the symptomatic and non-symptomatic limbs of the participants.
| Symptomatic (n = 63) | Non-Symptomatic (n = 63) | Mean Difference(95% CI) | |
|---|---|---|---|
| Pain during palpation (0–10) | 4.57 ± 2.55 | 0.87 ± 1.21 | 3.70 (3.10, 4.30)⁎ |
| VISA-A (0–100) | 49.30 ± 18.99 | 87.92 ± 12.33 | −38.62 (−42.79, −34.44)⁎ |
| Foot Posture Index (−12 to +12) | 4.36 ± 3.14 | 4.59 ± 3.39 | −0.23 (−0.70, 0.25) |
| Navicular Drop (mm) | 7.41 ± 4.51 | 6.83 ± 4.28 | 0.58 (−0.25, 1.43) |
| Navicular Drift (mm) | 5.95 ± 4.00 | 5.79 ± 4.14 | 0.16 (−0.77, 1.09) |
| Longitudinal Arch Angle (°) | 143.98 ± 11.52 | 143.68 ± 11.81 | 0.30 (−1.74, 2.34) |
| Ankle DF Knee Extended† (°) | 36.02 ± 8.52 | 36.23 ± 7.11 | −0.21 (−1.32, 0.90) |
| Ankle DF Knee Flexed† (°) | 42.30 ± 8.11 | 43.11 ± 6.42 | −0.81 (−2.15, 0.54) |
| Tendon Thickening (cm) | 0.26 ± 0.21 | 0.12 ± 0.12 | 0.14 (0.10, 0.20)⁎ |
| Neovascularization n (%) | 27 (42.9%) | 3 (4.8%) | 38.1 (24.8, 51.4)⁎ |
Data are (mean ± standard deviation).
Results of the comparisons between individuals with pronated symptomatic limbs (foot posture index≥6; n = 26) versus individuals with neutral/supinated symptomatic limbs (foot posture index<6; n = 37) are presented in Table 2. As expected, the individuals with pronated symptomatic limbs had greater navicular drop (MD=2.96 mm; 95%CI=0.77, 5.16), navicular drift (MD=2.70; 95%CI=0.76, 4.64), longitudinal arch angle (MD=−5.67º; 95%CI=−11.43, −0.09), and foot posture index (MD=4.88; 95%CI=3.85, 5.91) when compared to the individuals with neutral/supinated symptomatic limbs. However, there was no difference between groups with regards to pain during palpation, symptom severity, tendon thickening, neovascularization, or ankle dorsiflexion range of motion (P>.05) (Table 2).
Comparisons of participants’ demographics, foot alignment, tendon structure, pain, and symptom severity between individuals with symptomatic pronated feet vs individuals with symptomatic neutral/supinated feet†.
| Pronated (n = 26)† | Neutral/Supinated (n = 37)† | Mean Difference (95% CI) | |
|---|---|---|---|
| Age (years) | 46.04 ± 11.70 | 48.78 ± 13.60 | −2.74 (−9.32, 3.83) |
| Sex | 14 male (53.8%) | 19 male (51.4%) | 2.40 (−22.5, 27.5) |
| Body Mass Index (kg/m2) | 28.69 ± 4.26 | 29.38 ± 6.22 | −0.69 (−3.50, 2.13) |
| Foot Posture Index (−12 to +12) | 7.23 ± 1.21 | 2.35 ± 2.42 | 4.88 (3.85, 5.91)⁎ |
| Navicular Drop (mm) | 9.15 ± 4.23 | 6.19 ± 4.35 | 2.96 (0.77, 5.16)⁎ |
| Navicular Drift (mm) | 7.54 ± 4.04 | 4.84 ± 3.62 | 2.70 (0.76, 4.64)⁎ |
| Longitudinal Arch Angle (°) | 140.65 ± 8.62 | 146.32 ± 12.77 | −5.67 (−11.43, −0.09)⁎ |
| Ankle DF Knee Extended§ (°) | 35.99 ± 9.16 | 36.04 ± 8.22 | −0.05 (−4.94, 4.84) |
| Ankle DF Knee Flexed§ (°) | 41.70 ± 9.09 | 42.71 ± 7.50 | −1.01 (−5.65, 3.63) |
| Pain during Palpation (0–10) | 4.27 ± 2.25 | 4.78 ± 2.75 | −0.51 (−1.82, 0.79) |
| VISA-A (0–100) | 49.88 ± 20.18 | 48.89 ± 18.38 | 0.99 (−8.80, 10.79) |
| Tendon Thickening (cm) | 0.29 ± 0.18 | 0.25 ± 0.23 | 0.04 (−0.07, 0.15) |
| Neovascularization n(%) | 11 (42.3%) | 16 (43.2%) | −0.94 (−25.7, 23.9) |
Data are mean ± standard deviation, unless otherwise indicated.
CI, confidence interval; DF, dorsiflexion; VISA-A, Victorian Institute of Sports Assessment‒Achilles questionnaire (higher scores indicate fewer symptoms).
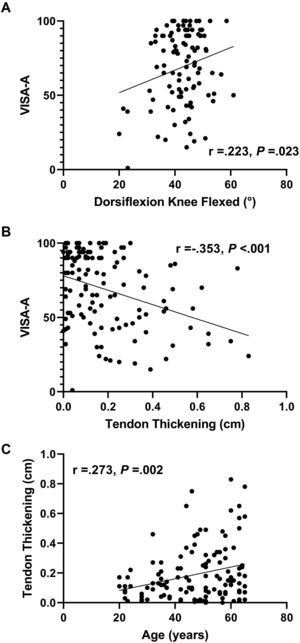
There were no correlations between any of the foot alignment measures and pain, symptom severity, or tendon thickening (P>.05). However, a significant, although low, correlation was observed between symptom severity and ankle dorsiflexion range of motion with the knee flexed (r = 0.223; P=.023) (Fig. 2). Significant but low correlations were also observed between tendon thickening and age (r = 0.273; P=.002) and symptom severity (r=−0.353; P<.001) (Fig. 2).
Correlations between symptom severity and ankle dorsiflexion range of motion with the knee flexed (A); symptom severity and tendon thickening (B) and; tendon thickening and age (C). VISA-A, Victorian Institute of Sports Assessment‒Achilles questionnaire (higher scores indicate fewer symptoms).
The purpose of this study was to compare static foot alignment measures and ankle dorsiflexion range of motion between the symptomatic and non-symptomatic limbs of individuals with unilateral AT. Considering the theoretical assumptions that excessive pronation could lead to Achilles tendon overload, we were interested in investigating whether there was a higher prevalence of pronated feet versus neutral/supinated feet in individuals with AT. We also aimed to compare tendon pain and structure, symptom severity, and ankle range of motion between individuals with symptomatic pronated feet and individuals with symptomatic neutral/supinated feet. Results showed no difference between the symptomatic and non-symptomatic limbs in any of the most popular methods of static foot alignment assessment: foot posture index, navicular drop, navicular drift, and longitudinal arch angle. Also, there was a similar number of pronated and neutral/supinated feet with symptoms in this sample and there was no difference between individuals with symptomatic pronated feet and individuals with symptomatic neutral/supinated feet with regards to tendon pain and structure, symptom severity, or ankle range of motion. Finally, a low positive correlation was observed between ankle dorsiflexion range of motion with the knee flexed and symptom severity, indicating that smaller range of motion in the ankle is associated with worse symptom severity.
Previous studies had suggested that excessive subtalar pronation would cause a “whipping phenomenon” in the Achilles tendon, promoting microtrauma with possible vascular blanching within the tendon.6,7 In an attempt to test this hypothesis, Karzis et al.40 measured the blood flow in the Achilles tendon in healthy participants with and without overpronated feet. The authors found that individuals with foot overpronation had increased vascular resistance and a reduced Achilles tendon blood flow.40 Similarly, Wezenbeek et al.41 measured the blood flow in the Achilles tendon of healthy runners before and after a 10-minute run. The authors found that greater foot pronation (eversion excursion) during running was associated with reduced blood flow in the tendon after the run.41 Collectively, these studies seemed to indicate that there was plausibility to consider excessive foot pronation as an important etiologic factor for the development of AT.
However, in a follow up prospective study, the same authors found that foot alignment, as measured by the foot posture index, was not a risk factor for the development of AT.15 Similarly, Nielsen et al.,16 in a prospective study, also found that runners with feet categorized as pronated or highly pronated using the foot posture index, were not at a higher risk of developing AT when compared to runners with neutral or supinated feet. More recently, a cross-sectional study found no difference between adolescents with and without Achilles tendon pain with regards to foot posture index measures,42 which is consistent with our results. It is possible that static foot alignment evaluations, such as the foot posture index, are not sensitive enough as a predictor of eversion range of motion during a dynamic running activity15 and considering the current evidence, these static measurements do not seem to be of relevance for injury risk or symptoms severity in individuals with AT.
Regarding ankle dorsiflexion range of motion, no difference was observed between the symptomatic and non-symptomatic limbs of participants of the current study. Contrasting with these results, previous studies have identified ankle dorsiflexion restriction in individuals with AT.7,17 In addition, in prospective studies, ankle dorsiflexion restriction was found to be a risk factor for the development of AT.18,19 The absence of differences between limbs in the present study may have occurred due to the relatively small sample size and the great variability among participants. However, in the present study, a low but significant positive correlation was observed between ankle dorsiflexion range of motion and symptom severity, which indicates that smaller dorsiflexion range of motion is associated with worse symptom severity in individuals with AT. To our knowledge, this is the first study that looked into the relationship between ankle range of motion and tendinopathy symptom severity and due to the cross-sectional nature of the study it is not known if the restriction in range of motion preceded injury development or is a result of the injury.
It has been hypothesized that patients who exhibit decreased dorsiflexion range of motion experience increased tension in the Achilles tendon and therefore are at a greater risk of developing tendinopathy.12 A few studies have also suggested that restricted range of ankle dorsiflexion excursion may limit the capacity of the ankle plantar flexors to absorb eccentric loads and result in greater loading rates in lower limb tendons.43-45 A recent systematic review concluded that restricted dorsiflexion range of motion is associated with alterations in the mechanics of weight-bearing activities such as jump-landings in a manner that may predispose individuals to injury.46 Specifically, it was observed that restricted dorsiflexion range of motion increases frontal plane ankle and knee excursion, reduces knee and hip sagittal excursion, and increases peak vertical ground reaction force, which potentially increases the risk of overload injuries.46 However, studies looking into the effects of dorsiflexion restriction in activities typically associated with the development of AT, such as running, are still lacking and should be the focus of future research.
Finally, in the current study tendon thickening had low to modest positive correlations with age and low negative correlation with symptom severity. This means that thicker tendons were observed in older participants and in participants with higher symptom severity. These results were expected, considering that tendon thickening is a typical sign of tendinopathy2,47 and considering that the risk of AT has been shown to increase with age.5,48
The limitations of this study need to be acknowledged. The study had a cross-sectional design and only symptomatic participants were included, therefore, no assumptions can be made about whether the outcome measures of this study are risk factors for AT. The absence of a control group is considered a limitation, because a few recent studies have shown bilateral changes in individuals with unilateral tendinopathy.49,50 However, the asymptomatic limb of the participants of the present study showed significant differences in relation to the symptomatic limb in terms of tendon pain, symptom severity, tendon thickening, and neovascularization, indicating that it served as a proper comparator. Only young adults and middle-aged individuals were evaluated in this study, so the generalization of these results to other populations should be done with caution. Finally, considering the multifactorial etiology of AT, future studies should conduct multivariable analyses to encompass all aspects of tendon health.
ConclusionsNo differences were observed in foot alignment, evaluated by static measures, between the symptomatic and non-symptomatic limbs of individuals with unilateral AT. There was also no difference between individuals with symptomatic pronated feet and individuals with symptomatic neutral/supinated feet regarding tendon pain and structure, symptom severity, or ankle range of motion. In addition, pronated foot posture was not more prevalent in this population when compared to neutral/supinated postures. Static foot alignment measures do not seem to be clinically relevant in patients with AT. Smaller ankle dorsiflexion range of motion, however, was associated with greater symptom severity and may, therefore, be relevant for this population.
Research reported in this publication was supported by the National Institute Of Arthritis And Musculoskeletal And Skin Diseases of the National Institutes of Health under Award Number R01AR072034. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors would like to thank past and current members of the Delaware Tendon Research Group who have assisted in the data collections.