Despite the well-known positive effects of exercise in patients with coronary artery disease, the best exercise training protocol is still under discussion.
ObjectiveWe performed a systematic review and a meta-analysis to investigate the effects of high-intensity interval training (HIIT) versus moderate-intensity continuous training (MICT) on exercise capacity and health-related quality of life (HRQoL) in patients with coronary artery disease.
MethodsWe searched MEDLINE/PubMed, the Cochrane Library EMBASE, and the PEDro database for randomized controlled trials that evaluated the effects of HIIT versus MICT. Mean difference and 95 % confidence intervals (CI) were calculated.
Results27 studies, with 1454 patients, met the eligibility criteria. Twenty-four studies with 1259 patients assessed peak oxygen consumption (VO2peak) as an outcome. The HIIT group showed an increase of VO2peak (MD = 2.11 mL/kg/min; 95 % CI: 1.14, 3.07; I2 = 78 %; N = 1259) compared with the MICT group. Six studies with 316 patients assessed HRQoL as outcome. No differences in physical, emotional, and social domains of HRQoL were found between the HIIT and MICT groups. In the subgroup analysis of 10 studies with isocaloric exercise training, the HIIT and MICT groups showed similar VO2peak (MD = 0.72 mL/kg/min; 95 % CI: −0.03, 1.48; I2 = 44 %; N = 453).
ConclusionsOur meta-analysis showed low-quality evidence that HIIT training was more effective than MICT for improving VO2peak but not HRQoL in patients with coronary artery disease. However, when the analysis was limited to isocaloric protocols no difference between HIIT and MICT was found for VO2peak.
Exercise capacity is an independent predictor of all-cause and cardiovascular mortality in patients with coronary artery disease.1 Poor health-related quality of life (HRQoL) is an independent risk factor for mortality and major cardiac events.2 Exercise-based cardiac rehabilitation has been established as a safe intervention for improving aerobic capacity, HRQoL, and survival in patients with coronary artery disease.3-5 However, the most efficient form of exercise training remains a topic of debate.
High-intensity interval training (HIIT) is a type of training that involves repeated bouts of high intensity effort interspersed by recovery times.6 High intensity is performed at 70–85 % peak oxygen consumption (VO2peak), 75–90 % maximal heart rate, 70–85 % heart rate reserve, or a rating of 14–16 on the Borg scale.7 Performing HIIT allows the patient to exercise at high intensity in a more tolerable manner, which is expected to provide a superior effect on peak aerobic capacity gain when compared to traditional moderate-intensity continuous training (MICT).5 Moderate intensity is exercise performed at 40–69 % VO2peak, 55–74 % maximal heart rate, 40–69 % heart rate reserve, or 12–13 rating on the Borg scale.7
Previous meta-analyses reported the superiority of HIIT over MICT in improving VO2peak (mean difference [MD] = 1.3 mL/kg/min, 95 % confidence interval [CI]: 0.6, 1.9).8-10 However, to our knowledge, the first meta-analysis comparing only isocaloric protocols, which was performed in 2017, showed that HIIT was not superior to MICT.11 Isocaloric protocols aim to adjust the energy expenditure within aerobic exercise sessions performed with different intensities. A limitation of this previous meta-analysis was that only four trials (n = 137) out of the 11 included studies reported the use of isocaloric protocols.11 In addition, a recent meta-analysis12 also showed an increase in VO2peak in favor of HIIT compared to MICT (MD = 1.92 mL/kg/min, 95 %CI: 1.3, 2.5). An even higher increase in VO2peak (2.36 mL/kg/min, 95 %CI: 1.99, 2.74) was observed when non-isocaloric protocols were analyzed separately. However, an analysis including studies using only isocaloric protocols was not performed.12 Since the publication of this recent meta-analysis12 new randomized controlled trials (RCTs) have been published. Moreover, none of these previous systematic reviews assessed the certainty of the evidence.
This systematic review investigates the effects of HIIT compared to MICT on exercise capacity (i.e., VO2peak) and HRQoL in patients with coronary artery disease. This is an update of our previous meta-analysis published in 2017. Moreover, we aimed to perform a subgroup analysis of studies that used isocaloric exercise training protocols.
MethodsThis systematic review and meta-analysis (PROSPERO: CRD42023410056) was performed in accordance with the PRISMA guidelines.13
Eligibility criteriaStudies were eligible if they satisfied the following criteria: a) Participants: adults (≥18 years) with coronary artery disease (i.e., history of coronary artery disease with angina pectoris or myocardial infarction diagnosed based on the American Heart Association standard criteria,14 angiographically documented cases, percutaneous coronary intervention, or coronary artery bypass grafting); b) Intervention/comparison: studies comparing HIIT (i.e., performed at 70–85 % peak VO2, 75–90 % maximal heart rate, 70–85 % heart rate reserve, or 14–16 rating on the Borg scale) and MICT (i.e., performed at 40–69 % peak VO2, 55–74 % maximal heart rate, 40–69 % heart rate reserve, or 12–13 rating on the Borg scale) that were completed on a bike or on a treadmill and performed at least twice a week for at least four weeks; c) Outcomes: VO2peak (measured in mL/kg/min by cardiopulmonary exercise test) and HRQoL (measured by any standardized and validated scales or questionnaires); d) Study design: an RCT. Studies that enrolled patients with other cardiac or respiratory diseases were excluded.
Search methods for identification of studiesWe searched for publications in MEDLINE/PubMed, the Cochrane Library, EMBASE, and the PEDro databases up to December 2022 without language restrictions. We used a standardized search strategy and, whenever possible, the same search terms (e.g., MeSH term for PubMed and the Cochrane Library and EMTREE for EMBASE). Our search strategy included three groups of keywords and their synonyms: study design, participants, and interventions.
The strategy developed by Higgins et al.15 was used to identify the RCTs in MEDLINE/PubMed. To identify the RCTs in other databases, we adopted a search strategy using similar terms. The references of the articles included in this meta-analysis were checked to identify other potentially eligible studies. The search strategies for MEDLINE/PubMed, EMBASE, and the Cochrane Library are presented in Supplementary Material - S1. For ongoing studies, confirmation of any data, or additional information, the authors were contacted through e-mail.
Data collection and analysisTitles and abstracts were independently checked by two reviewers. If at least one of the reviewers considered a reference eligible, the full text was obtained for complete assessment. Two reviewers independently assessed the full texts of the selected articles to verify whether they met the eligibility criteria. Two authors independently extracted data from the published reports using standard data extraction forms adapted from Higgins et al.15 The study population, intervention performed, follow-up period, rates of missing data, outcome measures, and results were reviewed.
Methodological qualityThe analysis of the methodological quality of the included studies was carried out using the PEDro scale.16 This scale consists of 11 items (1: eligibility criteria and source of participants; 2: random allocation; 3: concealed allocation; 4: baseline comparability; 5: blinded participants; 6: blinded therapists; 7: blind assessors; 8: adequate follow-up; 9: intention-to-treat analysis; 10: between-group comparisons; and 11: point estimates and variability). However, one item (eligibility criterion) is related to external validity and is generally not used to calculate the score, resulting in a score range of 0–10.16 Initially, the classification already available in the database was used. If the study was not yet classified, two authors carried out the analysis and classified the studies.
Statistical assessmentEffect estimates were obtained by comparing the mean change from baseline to the endpoint for each group. Thus, change scores [i.e., post- minus pre-intervention scores] were extracted from each study and expressed as mean ± standard deviation (SD). When the outcome change score was not described in the study, we made the calculation. To calculate the standard deviation of change we used the statistics (confidence intervals, SEs, t statistics, P values, F statistics) presented in the study according to recommendations made in the Cochrane Handbook chapters 6 and 10 using revman.15 In cases where studies presented data as mean ± standard error of the mean (SEM), SEM was converted to SD.17
The conversion of nonparametric data (i.e., median and interquartile range) to means and SDs was performed using recently established methods.18 In cases where the SD of change was unavailable, but confidence interval (CI) was available, we converted the CI to SD using the method described by Higgins et al.15 If the required outcome data were not found in the full text but were presented graphically, an attempt was made to digitize the graph.19
We compared HIIT versus MICT and performed a sub-analysis of studies that compared isocaloric exercise training protocols. Isocaloric protocols aim to adjust the energy expenditure within aerobic exercise sessions performed with different intensities.11 We considered isocaloric protocols when reported in the studies.
An α value of 0.05 was considered significant. Calculations were performed using a random-effects model. Statistical heterogeneity of the treatment effect among studies was assessed using Cochran's Q test and the I2 inconsistency test statistic. In these tests, values of 0 % to 40 % might not be important; 30 % to 60 % may represent moderate heterogeneity; 50 % to 90 % may represent substantial heterogeneity; and 75 % to 100 % may indicate considerable heterogeneity.15 All analyses were conducted using Review Manager version 5.4 (Cochrane Collaboration).20
The sensitivity analysis was performed by re-running the meta-analysis, excluding studies with a high risk of bias according to PEDro score (≤4 points), and then employing the leave-one-out method by removing one study at a time and repeating the analysis.
Certainty of evidenceThe certainty of evidence was assessed using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach. Quantitative data from Cochrane's review manager were imported into GRADEpro GDT 2015 to create a “Summary of findings table.” The assessment involved five items: risk of bias, imprecision, inconsistency, indirectness, and publication bias.15,21 The certainty of evidence was downgraded by one level for risk of bias if more than a quarter of the studies included in the meta-analysis were considered to have a high risk of bias (i.e., defined as RCTs with a PEDro score ≤4 points). Imprecision was evaluated by visually analyzing the confidence intervals. If necessary, imprecision was evaluated using absolute risk analysis, number needed to treat, or optimal information size calculation. Results were considered imprecise if the total sample size was <300 and <400 for dichotomous and continuous outcomes, respectively. We downgraded for inconsistency if there was clinical or statistical heterogeneity (i.e., I2>40 %) or if there were no overlapping confidence intervals. For indirectness, we initially observed the pre-established PICO criteria (Population, Intervention, Comparator, and outcome). We compared the characteristics of the study populations to those of the population of interest outlined in our PICO criteria. Discrepancies such as age, disease severity, and comorbidities were recorded. We evaluated the interventions and comparators in each study for concordance with those defined in our review protocol. We examined whether the studies reported outcomes that were directly relevant to our research question and whether these outcomes were measured and reported in a way that allowed comparison across studies. Publication bias was assessed by visual inspection of funnel plots (i.e., scatterplots of the effect size from individual studies against its standard error) for meta-analyses with at least 10 trials.15,21-23 Reasons for downgrading were noted and attached to the summary of findings table.
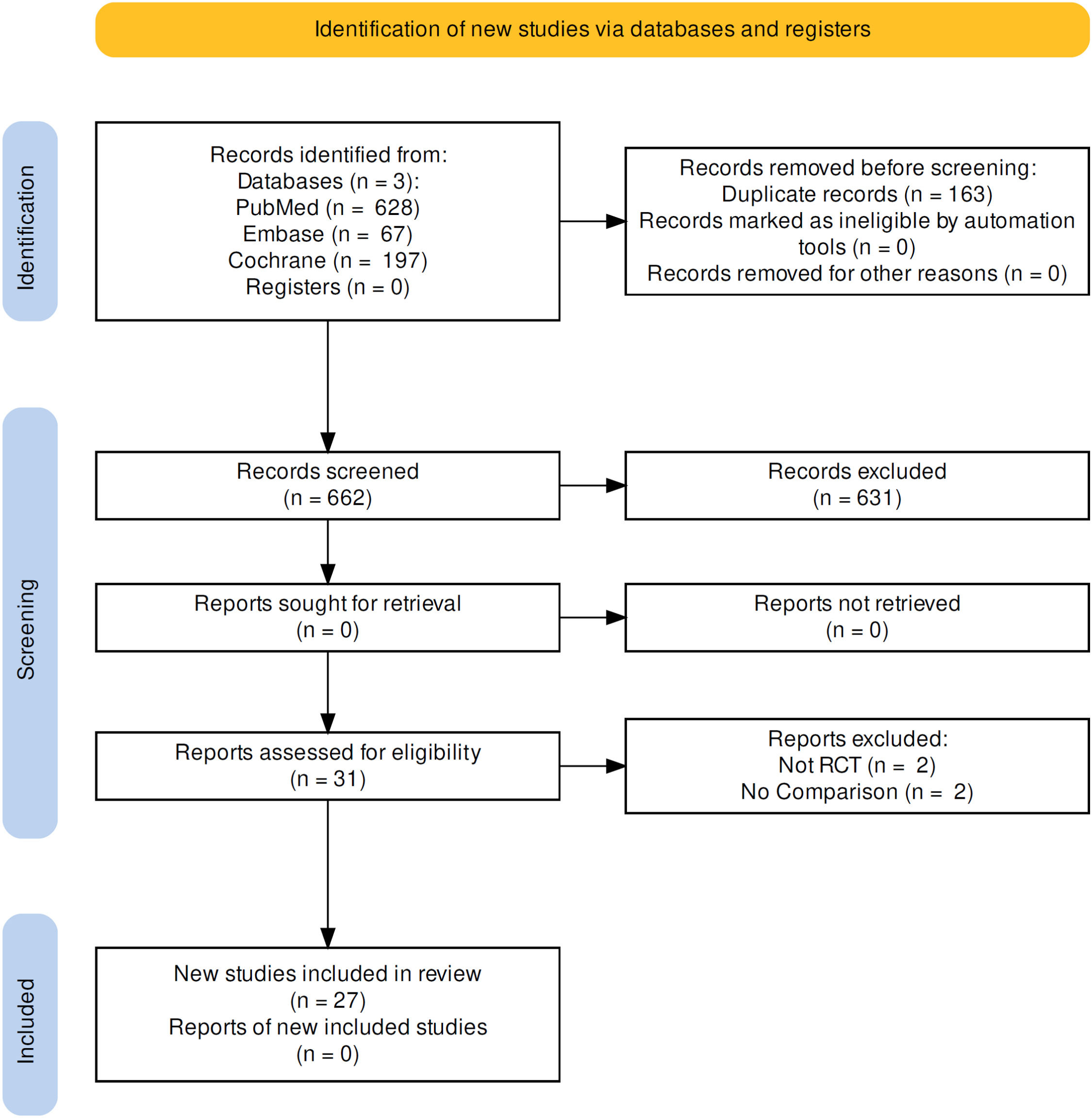
ResultsDescription of selected studiesThe initial search identified 892 titles and abstracts. Of these, 31 were considered potentially relevant and retrieved for full-text analysis. Finally, 27 studies24-50 involving 1454 patients met the eligibility criteria and were included in the systematic review. A flowchart depicting the selection process for each stage is shown in Fig. 1. PEdro scale scores of the included studies are presented in Supplementary Material - S2.
Study characteristicsThe mean age of the participants ranged from 50 to 70 years. Twenty-three studies included patients of both sexes and four studies included only men. The sample size, population characteristics, outcomes, and characteristics of the exercise programs of the included studies are summarized in Supplementary Material - S3. HIIT programs were generally performed 2 to 4 times per week, with 4 × 4-minute high-intensity intervals, with intensities ranging from 85 to 95 % of peak heart rate and The Borg rating of perceived exertion scale (Borg scale) rating >15. The MICT programs were generally performed 2 to 4 times per week, with intensities ranging from 60 % to 70 % of peak heart rate and Borg scale rating of 11–14.
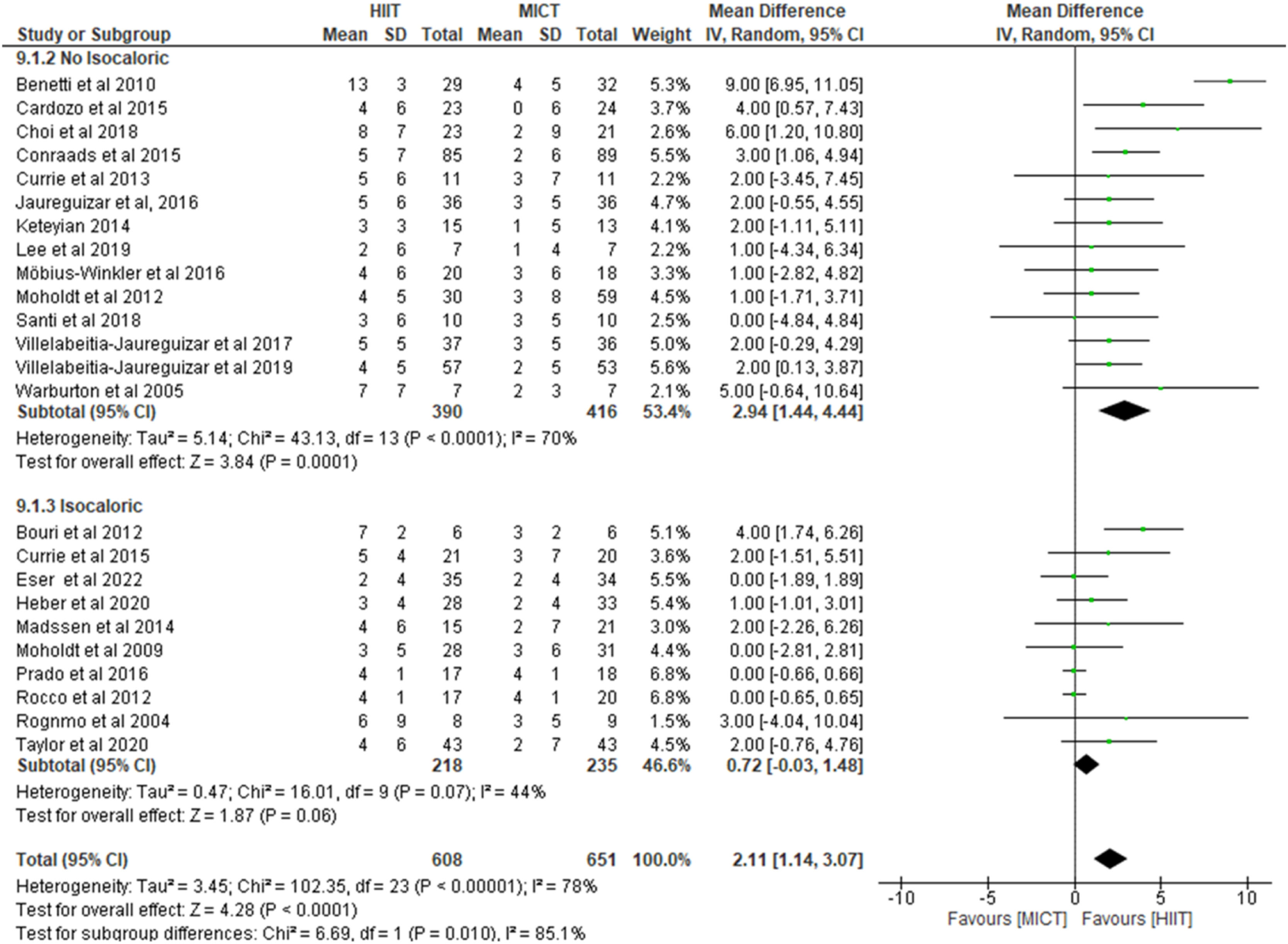
VO2peakTwenty-four studies with 1259 patients assessed VO2peak as an outcome. The studies showed mean VO2peak at baseline and post-intervention of 24 mL/kg/min and 28 mL/kg/min, respectively. The meta-analysis showed that the HIIT group improved VO2peak by 2.11 mL/kg/min (95 % confidence interval [CI]: 1.14, 3.07, I2 = 78 %, N = 1259, low certainty of evidence) greater than the MICT group (Fig. 2).
The meta-analyses of the 14 studies that did not use isocaloric exercise training showed that the HIIT group improved VO2peak by 2.94 mL/kg/min (95 % CI: 1.44, 4.44, I2 = 70 %, N = 806, low certainty evidence) compared to the MICT group (Fig. 2). When we removed one study at a time, the study by Benetti et al.47 had the most impact in reducing heterogeneity, which decreased from 70 to 0 %. The MD decreased from 2.94 to 2.26 mL/kg/min (95 % CI: 1.43, 3.08). When we also removed studies of low methodological quality (PEDro score of ≤4 points), heterogeneity was also reduced to 0 % and the MD decreased to 2.33 mL/kg/min (95 % CI: 1.38, 3.28, I2=0 %, N = 601).
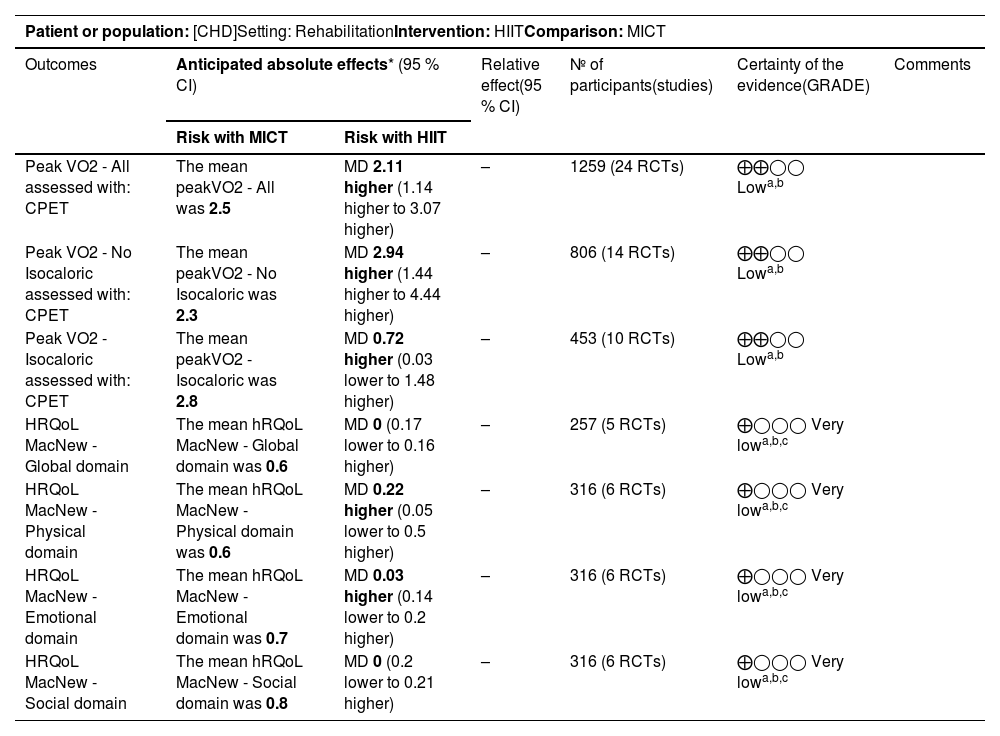
Ten studies used isocaloric exercise training protocols. This subgroup analysis showed that HIIT may have little or no effect on VO2peak (MD= 0.72 mL/kg/min, 95 % CI: −0.03, 1.48, I2 = 44 %, N = 453, low certainty evidence) compared to the MICT group (Fig. 2). When we removed one study at a time, the study by Bouri et al.44 had the most impact in reducing heterogeneity, which decreased from 44 to 0 %. The MD decreased from 0.72 mL/kg/min to 0.15 mL/kg/min (95 % CI: −0.27, 0.57). When we also removed studies of low methodological quality (PEDro score ≤4 points), heterogeneity was also reduced to 0 % and the MD decreased to 0.21 mL/kg/min (95 % CI: −0.35, 0.76, I2=0 %, N = 365). Certainty of evidence is presented in Table 1.
Summary of findings: HIIT compared to MICT for [CHD].
| Patient or population: [CHD]Setting: RehabilitationIntervention: HIITComparison: MICT | ||||||
|---|---|---|---|---|---|---|
| Outcomes | Anticipated absolute effects* (95 % CI) | Relative effect(95 % CI) | № of participants(studies) | Certainty of the evidence(GRADE) | Comments | |
| Risk with MICT | Risk with HIIT | |||||
| Peak VO2 - All assessed with: CPET | The mean peakVO2 - All was 2.5 | MD 2.11 higher (1.14 higher to 3.07 higher) | – | 1259 (24 RCTs) | ⨁⨁◯◯ Lowa,b | |
| Peak VO2 - No Isocaloric assessed with: CPET | The mean peakVO2 - No Isocaloric was 2.3 | MD 2.94 higher (1.44 higher to 4.44 higher) | – | 806 (14 RCTs) | ⨁⨁◯◯ Lowa,b | |
| Peak VO2 - Isocaloric assessed with: CPET | The mean peakVO2 - Isocaloric was 2.8 | MD 0.72 higher (0.03 lower to 1.48 higher) | – | 453 (10 RCTs) | ⨁⨁◯◯ Lowa,b | |
| HRQoL MacNew - Global domain | The mean hRQoL MacNew - Global domain was 0.6 | MD 0 (0.17 lower to 0.16 higher) | – | 257 (5 RCTs) | ⨁◯◯◯ Very lowa,b,c | |
| HRQoL MacNew - Physical domain | The mean hRQoL MacNew - Physical domain was 0.6 | MD 0.22 higher (0.05 lower to 0.5 higher) | – | 316 (6 RCTs) | ⨁◯◯◯ Very lowa,b,c | |
| HRQoL MacNew - Emotional domain | The mean hRQoL MacNew - Emotional domain was 0.7 | MD 0.03 higher (0.14 lower to 0.2 higher) | – | 316 (6 RCTs) | ⨁◯◯◯ Very lowa,b,c | |
| HRQoL MacNew - Social domain | The mean hRQoL MacNew - Social domain was 0.8 | MD 0 (0.2 lower to 0.21 higher) | – | 316 (6 RCTs) | ⨁◯◯◯ Very lowa,b,c | |
The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: confidence interval; MD: mean difference
GRADE Working Group grades of evidence
High certainty: we are very confident that the true effect lies close to that of the estimate of the effect.
Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect.
Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect.
Explanations.
Studies without allocation concealment, blinding, intention-to-treat analysis, and/or sample size calculation.
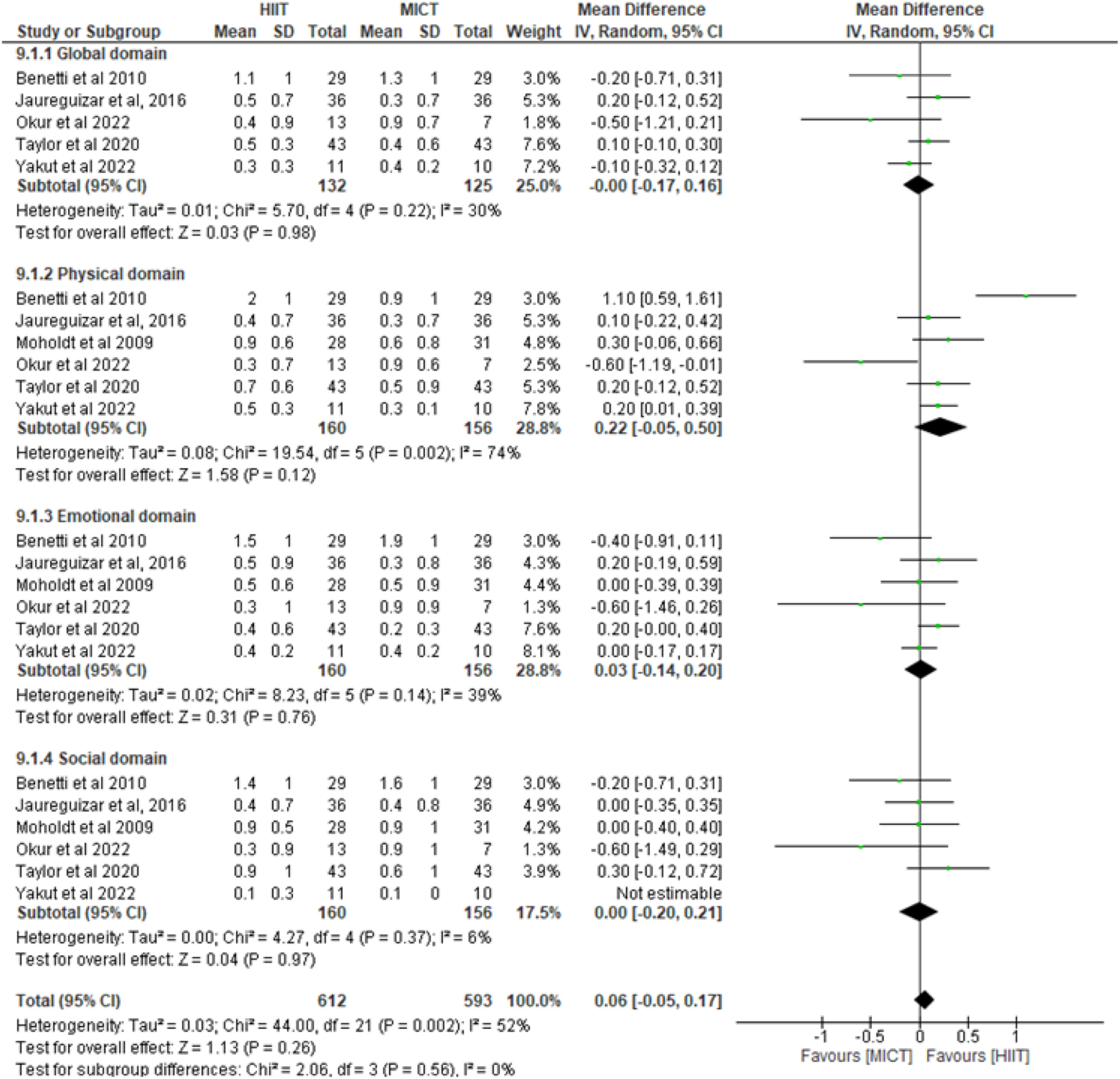
Six studies involving 316 patients assessed the HRQoL using the MacNew questionnaire (global, physical, emotional, and social domains). No difference were found in all domains between participants in the HIIT group and those in the MICT group (Fig. 3). The certainty of the evidence was rated as very low (Table 1).
DiscussionOur meta-analysis revealed low certainty evidence that HIIT may better improve VO2peak compared to MICT in patients with coronary artery disease. However, when we analyzed studies that reported an isocaloric exercise training protocol, HIIT was no longer more effective than MICT. In addition, we found very low certainty evidence of no difference in improvement in HRQoL, including physical, emotional, and social domains between groups.
Systematic reviews comparing HIIT and MICT in other cardiovascular diseases suggested that HIIT is more effective in improving VO2peak than MICT.51-53 In contrast, our review showed that, when restricting the analysis to studies using isocaloric protocols in patients with heart failure and reduced ejection fraction, HIIT was no longer more effective than MICT.
HIIT is purported to be more effective in improving VO2peak in patients with coronary artery disease; however, the comparison of all studies without considering caloric expenditure seems to be weak.8-12 HIIT is a less time-consuming method of exercise compared with MICT; that is, patients can achieve the same energy expenditure in a shorter duration.7 Hence, testing the superiority of 30 min of HIIT exercise sessions with 30 min of MICT can imply a methodological error. Pairing exercise protocols based on expenditure should provide a more realistic comparison of HIIT and MICT.
Our meta-analyses showed that the superiority of HIIT over MICT disappeared when isocaloric protocols were compared. This report is important for guiding exercise prescriptions in clinical practice and research. Future studies should examine energy expenditure during exercise training and compare isocaloric protocols. A meta-regression by Vromen et al.54 showed that an increase in exercise capacity is primarily determined by total energy expenditure in patients with heart failure.54 Kraal et al.55 also conducted a meta-regression to assess the effect of total energy expenditure and its constituent training characteristics on exercise capacity in patients with coronary artery disease. They suggested that total energy expenditure is significantly related to improvements in exercise capacity and concluded that the design of an exercise program should primarily be aimed at optimizing total energy expenditure rather than one specific training characteristic.55
The strength of the present study lies in providing an update of the previous meta-analysis and conducting a subgroup analysis of the studies that reported an isocaloric exercise training protocol.11 Comparing with a previous systematic review11 that carried out a subgroup analysis of the studies reporting isocaloric exercise training protocol, the number of published RCTs increased from 12 to 27 and the number of enrolled patients increased from 609 to 1425. Interestingly, the number of patients enrolled in isocaloric protocol studies increased from 137 to 453, underscoring the impact of our previous meta-analysis on shaping the design of new studies. Another important aspect of this update is that 19 of the 24 studies included in the VO2peak analysis showed no differences between HIIT and MICT.
Another strength of our systematic review is the inclusion of VO2peak and HRQoL as outcomes. These outcomes are relevant because VO2peak is the gold standard method for assessing aerobic exercise capacity and is related to quality of life and prognosis in patients with chronic conditions.56,57 In addition, we incorporated the analysis of the certainty of the evidence in the present review and observed a low to very low certainty of the evidence, alerting to the uncertainties in the results presented. Moreover, the results of this meta-analysis are limited by the lack of high-quality studies.
Given the significant heterogeneity found in the primary analyses due to variance in exercise protocols (variable intensities and different durations of the exercise programs), caution is warranted when interpreting our results. Despite this, our results ultimately reflect the body of evidence regarding HIIT compared with MICT and the relevant outcomes for patients with coronary artery disease. Further investigations into the prescription of exercise training variables (e.g., intensity, energy expenditure, bouts, frequency, and duration) are recommended to enhance our understanding of the real superiority of HIIT over MICT on VO2peak and HRQol.
ConclusionThis systematic review with meta-analysis showed low certainty evidence that HIIT may be more effective than MICT in improving VO2peak in patients with coronary artery disease. However, when we adjusted our analysis to include studies reporting similar energetic expenditure, HIIT showed little or no difference in improving VO2peak compared to MICT. Moreover, we found very low certainty evidence of no difference in quality of life between HIIT and MICT.
Authors' contributionsMGN: Conception and design of the study, Analysis and interpretation of data, Drafting the article, and Final approval of the version to be submitted ARD: Conception and design of the study, Analysis and interpretation of data, and Final approval of the version to be submitted; LSC: Conception and design of the study, Analysis and interpretation of data, Final approval of the version to be submitted; CMS: Conception and design of the study, Acquisition of data, Drafting the article, Final approval of the version to be submitted; BPM: Conception and design of the study, Acquisition of data, Analysis and interpretation of data, Drafting the article, and Final approval of the version to be submitted. VOC: Conception and design of the study, Analysis and interpretation of data, Drafting the article, and Final approval of the version to be submitted.
The authors declare no competing interest.
All authors declare no specific funding for this contribution. The study received support from the Conselho Nacional de Desenvolvimento Científico e Tecnológico – Brasil (CNPq). "Bolsista do CNPq – Brasil”.