Our 2019 systematic review found that up to 63% of physical therapists provided recommended care for musculoskeletal conditions, up to 43% provided non-recommended care, and up to 81% provided care of unknown value. We included studies published as early as 1993 and as recent as 2017.
ObjectiveTo determine whether physical therapists’ treatment choices for musculoskeletal conditions have improved over time.
MethodsFor the original review, we included studies (until April 2018) that quantified physical therapy treatment choices for musculoskeletal conditions through surveys of physical therapists, audits of clinical notes, and other methods (e.g. clinical observation). Using medians and interquartile ranges, we summarised the percentage of physical therapists who provided treatments that were recommended, not recommended, and of unknown value. For this analysis, we stratified the findings from the above systematic review by decade (1990–1999, 2000–2009, 2010–2018).
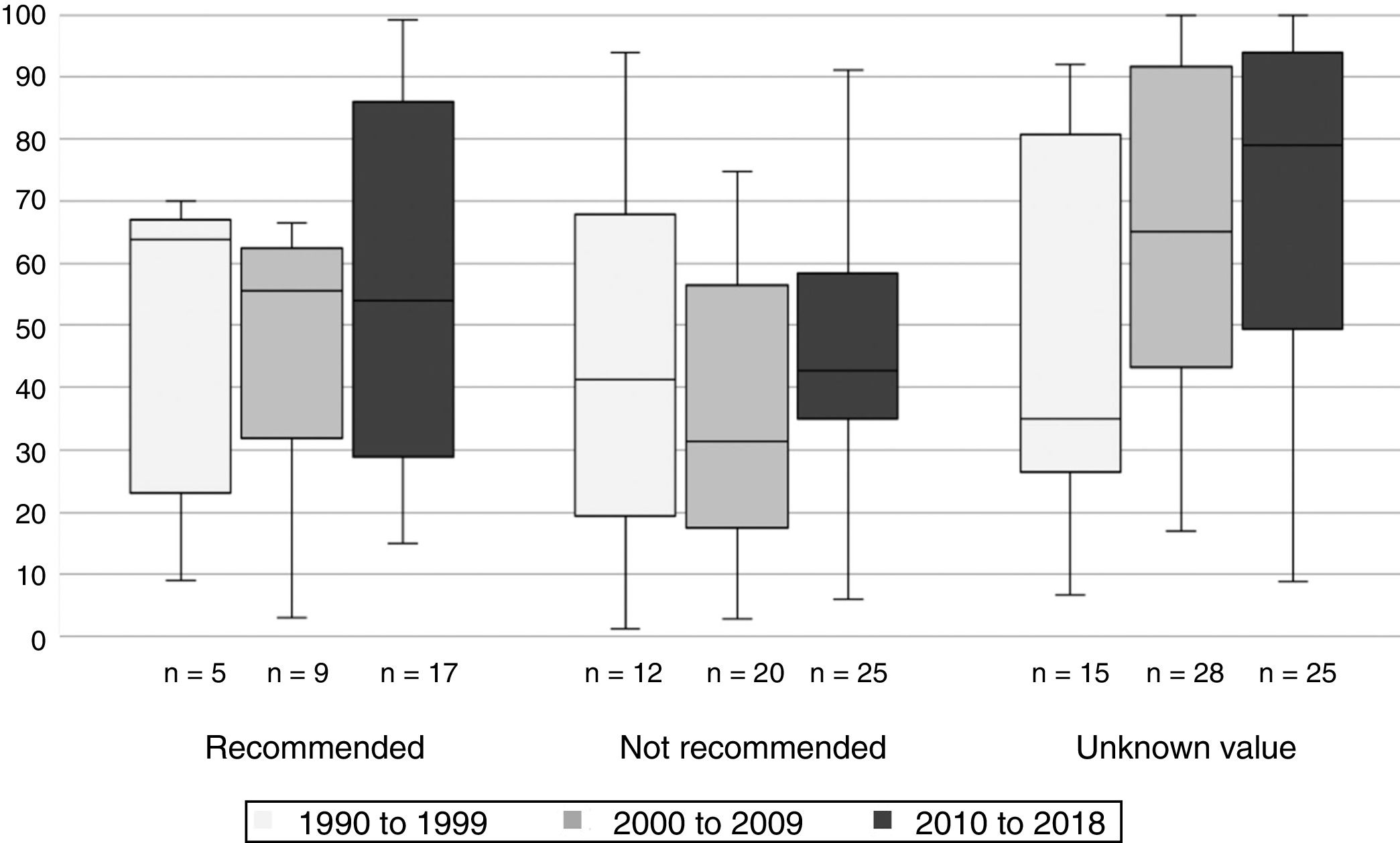
ResultsThe median percentage of physical therapists who provided recommended treatments (40% from 1990 to 1999, 50% from 2000 to 2009, and 35% from 2010 to 2018) and non-recommended treatments (41%, 28%, and 39% respectively) has not changed over time. However, more physical therapists seem to be providing treatments of unknown value (41% from 1990 to 1999, 55% from 2000 to 2009, and 70% from 2010 to 2018).
ConclusionPossible explanations for this trend include the growing need for clinical innovation, challenge of keeping up to date with evidence, increased exposure to treatments of unknown value, belief that evidence is not relevant to practice, and possible limitations of the data. Strategies to help physical therapists replace non-recommended care with recommended care are discussed.
Our 2019 systematic review of 94 studies across 19 countries was, to our knowledge, the first study to summarise physical therapy treatment choices for musculoskeletal conditions. In this study, we determined that up to 63% of physical therapists provide recommended care for musculoskeletal conditions (i.e. care recommended in guidelines or systematic reviews).1 This result appears a little better than the overall rates of recommended care provided by various health professionals in the United States (55%, assessed in 2003)2 and Australia (57%, assessed in 2012).3 So, in terms of providing evidence-based care, physical therapists do as well or better than their medical peers.
A separate issue is to what extent practitioners provide care that is not recommended, either because it is ineffective or is yet to be appropriately evaluated. Our review1 found that up to 43% of physical therapists provide treatments not recommended in guidelines (i.e. treatments that guidelines recommend against), while up to 81% provide treatments of unknown value (i.e. treatments not mentioned in guidelines because they are yet to be appropriately evaluated). Because this issue has not been explored in previous studies, we have no benchmarks to compare physical therapy to and it may be premature to be critical. It is likely more productive to explore the data further.
Our review included studies published between 1993 and 2017. Evidence-based physical therapy emerged in 1990s, and since then, more physical therapists are attending scientific conferences and becoming involved in research. It is possible physical therapists’ treatment choices have become better aligned with guidelines over time and that the overall estimates do not reflect practice in 2019. Because no study has explored this issue, there is need for data to test this hypothesis. The aim of this secondary analysis was to determine whether physical therapy treatment choices have changed over time. To answer this question, we stratified data from the original review by decade (1990–1999, 2000–2009 and 2010–2018).
MethodsMethods used in this paper have been described in detail in the original review.1 In brief, we conducted a comprehensive search in several electronic databases combining terms relating to “practice patterns” and “physical therapy”. Additional studies were identified by citation tracking and hand searching. Two independent reviewers performed the selection of studies and resolved disagreements through discussion. We included studies that reported physical therapy treatment choices for musculoskeletal conditions through surveys of physical therapists, audits of clinical notes, and other methods (e.g. surveys of patients). Data were extracted by one reviewer and independently checked by a second. Methodological quality was assessed independently by two reviewers using a modified version of the Downs and Black checklist.4
Classification of physical therapy-delivered treatments as recommended and non-recommended was based on recommendations from well-recognised evidence-based clinical practice guidelines or conclusions from recent systematic reviews. Treatments were classified as being of unknown value when guideline recommendations and evidence from systematic reviews was inconclusive. We used medians and interquartile ranges (IQR) to summarise the percentage of physical therapy treatment choices that involved treatments that were recommended, non-recommended, and of unknown value. To determine whether physical therapy practice has changed over time, we stratified the findings of our review by decade (1990–1999, 2000–2009 and 2010–2018). Assessment of change was qualitative and based on comparing median percentages between decades.
ResultsThe 94 included studies explored physical therapists’ treatment choices for low back pain (n=48 studies), knee pain (n=10), neck pain or whiplash (n=11), foot or ankle pain (n=5), shoulder pain (n=7), pre or post knee arthroplasty (n=6), and others (n=18). A summary of study characteristics can be found in the original review.1 To summarise the main findings of the original review, up to 63% of physical therapists provided recommended care for musculoskeletal conditions, up to 43% provided non-recommended care, and up to 81% provided care of unknown value. But have physical therapists’ treatment choices improved overtime?
Physical therapists’ use of recommended and non-recommended treatments has remained largely unchanged since 1990s (Fig. 1). The median percentage of physical therapists who provide recommended treatments was 40% from 1990 to 1999, 50% from 2000 to 2009, and 35% from 2010 to 2018. For non-recommended treatments, these percentages were 41%, 28%, and 39%, respectively. Examples of recommended treatments (based on the studies included in the review) include advice to stay active and reassurance for low back pain and strengthening exercises for knee osteoarthritis. Examples of non-recommended treatments include electrotherapy for neck pain and joint mobilisations for acute lateral ankle sprains. In contrast to the above findings, the median percentage of physical therapists providing treatments of unknown value appears to be increasing (41% from 1990 to 1999, 55% from 2000 to 2009, and 70% from 2010 to 2018) (Fig. 1). Examples of treatments that are of unknown value for low back pain include workplace interventions, myofascial release, cold therapy, relaxation therapy, and laser therapy. Examples for neck pain include acupuncture, McKenzie, and advice on posture.
DiscussionSo why are more physical therapists embracing treatments of unknown value? We discuss several possible explanations below and conclude with potential strategies to replace non-recommended care with recommended care.
The need for clinical innovationPhysical therapists are managing a greater range of conditions than ever before and for some conditions, innovation is required before science ‘catches up’ to practice. For example, there is far less research to guide the management of conditions like temporomandibular joint disorder (n=184 trials relevant to physical therapy) and cuboid syndrome (n=0) compared to low back pain (n=1609).5 Experimenting with treatments of unknown value might be necessary for conditions with a relatively weak evidence-base and for complex patient presentations; especially if patients have not responded to the few evidence-based treatment options available. Innovation might also be driven by the rapidly expanding physical therapy workforce which may force clinicians to be ‘innovative’ to secure market share.
The challenge of keeping up to date with evidenceAcquiring evidence and interpreting research findings is time consuming. This likely explains why lack of time is the most frequently reported barrier to keeping up to date with evidence among physical therapists6 and why studies of evidence practice gaps commonly report that the delay in research translation is around 17 years.7 Lack of time may be an even greater barrier for physical therapists that do not have skills in formulating research questions (30–41% of physical therapists), searching research databases (16–73%), and critically appraise research (30–52%)6. Given that the number of physical therapy trials doubles every 3.5 years5 and evidence is rapidly evolving, the challenge of keeping up to date with evidence will only increase in the future.
Increased exposure to treatments of unknown valueSocial media and continuing education courses provide a platform to increase exposure to innovative, evidence-based treatments in physical therapy. Information delivered through blog posts, infographics, and videos, as well as popular courses, is easier to digest compared to traditional research articles and can help physical therapists keep up to date with evidence. An unintended consequence is the increased exposure to claims about treatments of unknown value. Physical therapists that do not have the time nor skills to explore the validity of claims made on social media and courses are particularly vulnerable to misleading information. The danger is that physical therapists take these claims at face value and start experimenting with treatments where the benefits and harms are poorly understood.
The belief that evidence is not relevant to practiceA systematic review of 12 studies6 found that many physical therapists believe evidence-based practice is not important (7–52%), does not improve the quality of care (16–49%), and does not aid clinical decision making (17–34%). A survey of 274 physical therapists in Canada found that only 46% agree that guidelines should inform the management of low back pain.8 A survey of 543 Australian physical therapists9 found that only 52% agreed that physical therapists should not use electrotherapy for low back pain, and that was driven by the belief that clinical experience is more informative than research evidence (i.e. belief in non-recommended care due to confirmation bias). Another view that emerged from this survey was that blanket recommendations against non-evidence-based care is inappropriate because some patients believe non-evidence-based care is effective (due to prior beliefs and experiences) and request such care.9 Ignoring these requests can be difficult for physical therapists trying to build a strong therapeutic alliance with their patients or physical therapists who work in settings where they profit from providing more care.
A separate but related issue is where guidelines are developed. Even among physical therapists who believe evidence is relevant to pratice, implemeting guideline recommendations can be difficult when existing guidelines have been developed in countries with different cultures, health systems, and levels of resources.
Limitations of the dataAlthough the above factors could explain the increase in physical therapists’ use of treatments of unknown value (Fig. 1), it is possible the effect of time is an artefact of the number of included studies across analyses, different methods of assessing treatment choices, and different conditions included. It is also important to acknowledge that the original review1 did not consider factors such as patient presentation and clinical reasoning when determining the percentage of physical therapists that follow evidence-based guidelines. Some may argue that treatments of unknown value may be appropriate if it aligns with patients’ values and preferences or helps build a strong alliance between physical therapists and their patients. This is supported by several studies demonstrating that therapeutic alliance improves treatment satisfaction and may even improve outcomes – by maximising non-specific treatment effects – in patients with musculoskeletal conditions.13
How to replace non-recommended care with recommended careSeveral strategies appear effective at increasing physical therapists’ use of recommended care for musculoskeletal conditions. These include the distribution of clinical practice guidelines,10 local opinion leader-led education seminars,11 and peer assessment.12 What we do not know, due to lack of research, is what can help physical therapists reduce their use of treatments that are not recommended. We therefore propose two important starting points to address the problem of non-evidence-based physical therapy.
Increasing access to trustworthy informationEmail services that notify users when new research in their field has been published makes evidence more accessible for busy clinicians (e.g. ‘PEDro Evidence in your inbox’5). However, these services do not solve the problem of access (as most papers are behind paywalls) nor the time burden of reading and interpreting research. Although government support to disseminate evidence could help reduce the issue of access (e.g. funders mandating publication in open access), it is vital that researchers find ways to increase the visibility and impact of their work beyond traditional academic channels. Researchers should harness social media to maximise their reach to busy clinicians by communicating their work, in accessible language, through podcasts, infographics, and blog posts. However, because researchers are not exempt from providing misleading information, clinicians must have the skills to decipher between evidence-based and non-evidence-based claims.
Improving physical therapists’ ability to think critically about treatment claimsTo ensure clinicians are equipped with the skills to critically evaluate treatment claims, physical therapy education must dedicate sufficient time to developing, mastering, and updating skills in evidence-based practice. All physical therapists should be able to efficiently find research, critically appraise research, and most importantly, determine how research findings may or may not be applied to practice. This will reduce the time burden of keeping up to date with evidence and help physical therapists think critically about claims they hear regarding new tests or treatments. Professional associations have an important role to play in promoting (and perhaps mandating) continuing education courses on evidence-based practice. The current emphasis seems to be on courses promoting treatment approaches. Upskilling the physical therapy profession to better critically appraise treatment claims will make it much harder for untested treatments to creep into routine practice and compete with recommended care.
ConclusionPhysical therapists’ use of recommended care has not changed since 1990s yet use of treatments of unknown value appears to be increasing. Possible explanations for this trend include the growing need for clinical innovation, challenge of keeping up to date with evidence, increased exposure to treatments of unknown value, belief that evidence is not relevant to practice, and possible limitations of the data. Key strategies to help physical therapists replace non-recommended care with recommended care including increasing access to trustworthy information and improving physical therapists’ ability to think critically about treatment claims.
Funding sourcesNone received.
Conflicts of interestThe authors declare no conflicts of interest.