Cardiopulmonary exercise testing (CPET) is the gold standard for functional capacity assessment, although it is costly and not easily accessible. The Glittre-ADL test may be a low-cost alternative for patients with heart failure.
ObjectiveTo establish a cutoff point for functional capacity of patients with heart failure using the Glittre-ADL test. We also assessed agreement, reliability, and minimal detectable change.
MethodsThis cross-sectional study was conducted with 78 patients (aged 21 to 65 years) with heart failure and reduced ejection fraction (functional classes II and III of the New York Heart Association). Test-retest reliability was measured using the intraclass correlation coefficient (ICC), while receiver operating characteristic (ROC) curves were used to determine whether ADL-time, could distinguish between patients with peak oxygen consumption (VO2peak) < 16 versus those ≥ 16 ml/kg/min.
ResultsA cutoff point of 255 s (76 % sensitivity [95 % CI 58, 89] and 72 % specificity [95 % CI 56, 85]) was established based on the total time spent on Glittre-ADL test; the area under the curve was 0.773 (95 % CI 0.663, 0.861; p < 0.0001). Regarding agreement, a significant correlation was found between test and retest (r = 0.83, r2 = 0.69, p < 0.001). Intraclass correlation coefficient, absolute reliability, and minimal detectable change were 0.84 (95 % CI 0.45, 0.94; p < 0.001), 3.2 %, and 8.8 % (23.1 s), respectively.
ConclusionGlittre-ADL test showed good reproducibility in repeated tests. Thus, the cutoff point established by our study can be used in clinical practice instead of CPET to identify patients with severe heart failure.
Heart failure (HF) is a chronic cardiovascular syndrome that causes progressive deterioration, fatigue, and dyspnea at rest and during exercise and may lead to reduced submaximal and maximal functional capacity (FC).1
Cardiopulmonary exercise testing (CPET) is the gold standard for assessing maximal FC.2 This non-invasive test assesses aerobic capacity, response to exercise, and cardiorespiratory and metabolic performance3–5 and provides information on prognosis and clinical decision-making, especially for patients with heart transplant.5 However, it has limited accessibility for the general population due to high costs and the need for trained evaluators. Functional tests assess submaximal exercise, characterized by complex interactions between lungs, heart, and muscle groups,6 and are widely used in clinical practice because they measure functional status, assess therapeutic responses, and establish potential diagnoses.7 In contrast, maximal exercise tests (e.g., CPET) do not reflect limitations in activities of daily living (ADLs); ADL performance is better predicted using functional tests than tests focused on isolated components.7,8
The Glittre-ADL test was developed to assess ADLs in patients with chronic obstructive pulmonary disease and provide additional information during FC assessment. Consequently, it emerges as an economical and practical instrument, facilitating the assessment of individuals in a more thorough manner when contrasted with other well-known assessments like the 6 min walk test. This assessment allows for the identification of functional status over time by replicating ADLs. Therefore, it is a new instrument that still lacks evidence, especially for assessing FC of patients with HF. Therefore, studies are needed to understand its applicability, results in this population, and correlation with standard tests.9
To our knowledge, the prognostic value of Glittre-ADL test and the cutoff point to distinguish FC are not established for patients with HF. Therefore, we aimed to determine a cutoff point for assessing FC of patients with HF and reduced ejection fraction (EF) using the Glittre-ADL test and comparing the results with the CPET. We also assessed its agreement, reliability, and minimal detectable change (MDC).
MethodsStudy designThis is a test retest study that followed the STARD guidelines.10
ParticipantsPatients with HF were randomly selected from the main referral centers of Recife (Brazil). Data were collected from January 2015 to February 2020. The study was approved by the research ethics committee of the Universidade Federal de Pernambuco, Brazil (number 38,572,614.1.0000.5208). All participants signed the informed consent form.
Inclusion criteria were sedentary adults (21 to 60 years) of both sexes; former smokers for greater than five years; diagnosed with HF, systolic dysfunction, and reduced or borderline left ventricular EF (simple echocardiography within a month using Simpson's method); functional classes II or III (New York Heart Association [NYHA]); clinically stable; and with no medication changes within three months before the study.
Participants were excluded if they presented unstable angina; myocardial infarction or previous cardiac surgery up to three months before the study; obstructive pulmonary diseases (assessed using spirometry); chronic respiratory diseases; hemodynamic instability; recent facial trauma; acute nausea; vomiting; or orthopedic, neurological, or psychological diseases hindering test performance.
AssessmentsAssessments occurred on three occasions with an interval between 1 and 7 days: on the first day, participants performed anthropometric, respiratory, and CPET assessments; on the second day, they performed the first Glittre-ADL test; and within 7 days (mean of 3 days), the second Glittre-ADL test was conducted. The CPET was performed one hour after the respiratory assessment. The maximum interval of seven days between CPET and Glittre-ADL tests aimed to limit the influence of changes in clinical status and symptom severity on results. Moreover, a minimum interval was chosen to avoid overload because the study population was functionally compromised.
Respiratory muscle strength and pulmonary function were assessed using a digital manovacuometer (MVD-300, Globalmed) and a portable spirometer (Micro Medical Microloop MK8, England), respectively, according to the American Thoracic Society.11 Spirometry values were expressed as percentage of predicted for the Brazilian population.12
Tests were performed at the same time of the day to minimize the circadian influence on the studied variables. Medication use was kept constant during the assessment period, and participants were instructed not to perform strenuous activities one day before assessments.
The total time spent on Glittre-ADL test (ADL-time) and peak oxygen consumption (VO2peak) during CPET were used to compare test results because these variables assess FC.1 The cutoff point used for VO2peak was 16 ml/kg/min5,13 values below this cutoff point represented a low FC and worse prognosis.14
Cardiopulmonary exercise testingCPET was performed using the treadmill ramp protocol15,16 (Centurium 300, Micromed, Brazil) and the ErgoPC Elite® software associated with a 12-lead electrocardiogram (Micromed, Brazil). The following respiratory variables were assessed breath-by-breath using a gas analyzer under standard temperature, pressure, and humidity (Cortex – Metalyzer II, Germany) and with the patient wearing a leak-free face mask: VO2peak, VO2 at the first ventilatory threshold (VO2AT), ventilatory equivalent of carbon dioxide (VE/VCO2), slope of increase of ventilation relative to carbon dioxide production (VE/VCO2 slope), time to reach the first ventilatory threshold (TVO2 AT), time to reach VO2peak (TVO2 peak), and recovery time of 50 % of VO2peak (T1/2).
An experienced cardiologist and a trained staff performed the test in an environment equipped for emergencies. The cardiologist responsible for the CPET did not perform the Glittre-ADL test to avoid performance bias.
Glittre-ADL testThe Glittre-ADL test was performed according to Skumlien et al.9 and consisted of carrying a weighted backpack (2.5 kg for females and 5 kg for males) and performing the following sequence of activities: stand from a sitting position, walk 5 m, go up and down two-steps (steps were 17 cm tall and 27 cm wide), walk 5 m, move three 1 kg-objects positioned on a shelf (from the top to the bottom shelf, from the bottom shelf to the floor, then to the bottom shelf, and back to the top shelf), return to the chair, and sit in the chair (Fig. 1).
Patients were instructed to perform five laps as fast as possible without running. Verbal stimulus was not given during the test to avoid the influence of the evaluator on results. Respiratory rate, blood pressure, and dyspnea and fatigue perception (Borg scale) were assessed before and after the test. HR and peripheral oxygen saturation were assessed during the test using a heart rate monitor (Polar/FT1/Finland) and a portable pulse oximeter (Mindray/PM 50/USA), respectively. The time of each lap and ADL-time were also recorded.
Statistical analysisSample characterization was described using mean ± standard deviation and relative frequency (%).
Glittre-ADL test - cutoff pointIntra-group analyzes of the Glittre-ADL test (rest vs. final vs. recovery) were performed using Friedman's test (Dunn's post hoc) or repeated measures one-way ANOVA (Tukey's post hoc). Inter-group analyzes (VO2peak < 16 vs ≥ 16 ml/kg/min) were performed using the Mann-Whitney test or unpaired t-test. Cohen's r (non-parametric data) and Cohen's d (parametric data) effect sizes were calculated and interpreted as large (0.5), moderate (0.3), or small (0.1).17 Correlations between test and retest regarding ADL-time were performed using Pearson's correlation coefficient; coefficients of determination (r2) were also computed to assess effect sizes.
Receiver operating characteristic (ROC) curves were constructed to determine whether ADL-time, heart rate recovery in the first minute, and ventilatory equivalent for carbon dioxide (VE/VCO2slope) could distinguish between patients with VO2peak < 16 and ≥ 16 ml/kg/min. The optimal cutoff point (Youden Index), the area under the curve (AUC), sensitivity, specificity, and likelihood ratios were calculated using Medcalc software® 16.4.3 (Ostend, Belgium) and SigmaPlot® 12.0 statistical package (Systat Software Inc., California, USA).
Reproducibility and MDCTest-retest reliability was measured using the intraclass correlation coefficient (ICC), (two-way mixed effect- absolute agreement model) graphically represented by the Bland-Altman method,18 and interpreted as low (< 0.5), moderate (between 0.5 and 0.75), good (between 0.75 and 0.90), or excellent (> 0.90).19 For the Bland-Altman, a T Test for one sample was performed to compare the Bias against 0.
For absolute reliability, we calculated the standard error of the mean (SEM = SD √[1 – ICC]) followed by SEM% (SEM% = [SEM / mean] x 100).20 MDC and MDC% (MDC% = [MDC95/mean] x 100) were also calculated and considered acceptable (< 30%) or excellent (< 10 %).21 The Spearman rank correlation coefficient (rho) was used to evaluate the concurrent validity between CPET and Glittre-ADL test.
ICC analyses and the Bland-Altman plot were performed using GraphPad Prism 8.01 (LaJolla, USA) and SigmaPlot® 12.0 statistical package (Systat Software Inc., California, USA), respectively.
Sample size calculationSample size was calculated from a pilot study with 30 patients with HF aged between 21 and 65 years. Initially, a ROC curve was constructed to obtain the best cutoff point for ADL-time, followed by sensitivity and specificity. A cutoff point of 258 s was selected, considering the best Youden index (0.58) and the highest AUC (0.80). Participants with ADL-time equal to or above this cutoff point were included in the low FC group.
For sample size, two calculations (sensitivity and specificity) were performed using the simple proportion formula:22 N = Z2 x P (1-P) / e2; in which N = sample size, Z = z value corresponding to the confidence interval (1.96), P = sensitivity (91 %) or specificity (66 %), and e = percentage error (15 %). The estimated sample size was 13 participants for sensitivity and 38 for specificity.
The sample size for reliability and reproducibility was estimated based on ICC values.23,24 A total sample size of 40 participants was estimated considering an acceptable reliability (minimum acceptable ICC) of p0 = 0.60, expected reliability (expected ICC) of p1 = 0.80, power of 80 %, and significance level of 5 %. Calculations were performed using the G*Power software, version 3.1.9.2 (Kiel, Germany).
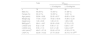
ResultsThe study included 78 participants. Sample characteristics are presented in Table 1 and in the Supplementary material-Table S1.
Anthropometric and echographic characteristics of the sample (total and classified according to VO2peak).
| Total | VO2peak | ||
|---|---|---|---|
| < 16 ml/kg/min | ≥ 16 ml/kg/min | ||
| n | 78 | 33 | 45 |
| Male (%) | 46 (59 %) | 15 (45 %) | 31 (69 %) |
| Female (%) | 32 (41 %) | 18 (55 %) | 14 (31 %) |
| Age (years) | 50.84 ± 9.96 | 52.45 ± 8.57 | 49.60 ± 10.84 |
| Weight (kg) | 77.64 ± 15.27 | 79.92 ± 18.44 | 75.89 ± 12.24 |
| Height (cm) | 1.65 ± 0.09 | 1.65 ± 0.10 | 1.65 ± 0.08 |
| BMI (kg/m2) | 28.41 ± 4.67 | 29.35 ± 5.60 | 27.70 ± 3.70 |
| LVEDD (cm) | 6.52 ± 1.09 | 6.90 ± 1.12 | 6.26 ± 1.01# |
| LVESD (cm) | 5.55 ± 1.13 | 6.01 ± 1.28 | 5.24 ± 0.91# |
| LAVI (ml/m2)† | 49.47 ± 37.19 | 53.22 ± 37.01 | 47.02 ± 37.76 |
| LVEF (%) | 32.00 ± 10.32 | 27.14 ± 8.50 | 35.73 ± 10.12### |
Fig. 2 shows the ROC curve for ADL-time to distinguish between patients with VO2peak < 16 and those ≥ 16 ml/kg/min, with the best sensitivity (76 %, 95 % CI 58, 89) and specificity (72 %, 95 % CI 56, 85), determined by the cutoff point of 255 s and AUC of 0.773 (95 % CI 0.663, 0.861; p < 0.0001); data referring to HRR1 and VE/VCO2slope are also provided. The positive and negative likelihood ratios for the cutoff point were 2.7 (95 % CI 1.6, 4.6) and 0.3 (95 % CI 0.2, 0.6), respectively.
Table 2 shows that an ADL-time of 255 s can differentiate pulmonary function, respiratory muscle strength, FC, and quality of life of patients with HF.
Pulmonary function, respiratory muscle strength, functional capacity, and quality of life according to the cutoff point of Glittre-ADL test.
| Total | < 255 s | ≥ 255 s | Effect size | |
|---|---|---|---|---|
| n | 78 | 35 | 43 | |
| Pulmonary function | ||||
| FEV1 (L) † | 2.29 ± 0.72 | 2.53 ± 0.59 | 2.03 ± 0.75### | 0.77 |
| FEV1 (%pred) | 71.88 ± 16.13 | 77.31 ± 14.25 | 66.16 ± 16.22## | |
| FVC (L) † | 2.90 ± 0.88 | 3.21 ± 0.68 | 2.53 ± 0.93### | 0.25 |
| FVC (%pred) | 73.33 ± 16.45 | 79.90 ± 14.66 | 66.41 ± 15.53### | |
| FEV1/ FVC | 80.15 ± 7.34 | 79.13 ± 6.06 | 81.25 ± 8.47 | |
| FEV1/ FVC (%pred) | 98.59 ± 8.62 | 97.10 ± 6.90 | 100.2 ± 9.97 | |
| Respiratory muscle strength | ||||
| MIP (cmH2O) | 81.66 ± 26.94 | 86.63 ± 26.85 | 76.57 ± 26.43 | 0.60 |
| MEP (cmH2O) | 100.04 ± 29.87 | 107.83 ± 31.07 | 91.85 ± 26.56# | |
| CPET | ||||
| HRR1′† | 17.55 ± 12.36 | 21.30 ± 12.93 | 14.11 ± 10.88# | 0.84 |
| HRR2′† | 31.99 ± 16.21 | 36.94 ± 18.14 | 27.58 ± 13.02## | 0.75 |
| VO2peak (ml/Kg/min) † | 52.45 ± 8.57 | 20.74 ± 7.54 | 15.49 ± 3.44### | |
| VO2VT1 (L) † | 14.56 ± 4.46 | 16.15 ± 5.10 | 12.94 ± 2.95### | 1.63 |
| VE/VCO2 | 33.30 ± 6.46 | 32.23 ± 5.08 | 34.39 ± 7.53 | 0.93 |
| VE/VCO2slope | 38.01 ± 8.14 | 37.63 ± 7.10 | 38.40 ± 9.19 | 0.85 |
| VO2peak time (s) | 440.85 ± 129.23 | 484.50 ± 108.90 | 397.20 ± 134.50## | 1.22 |
| VT1 time (s) | 284.08 ± 103.90 | 302.70 ± 88.56 | 265.00 ± 115.70 | 1.07 |
| Power (W) † | 2.85 ± 1.56 | 3.40 ± 1.85 | 2.26 ± 0.86### | 1.10 |
| T1/2 50 % (s) | 164.29 ± 36.86 | 153.20 ± 35.46 | 175.60 ± 35.20## | 1.00 |
| MLHFQ | 26.48 ± 14.22 | 38.21 ± 24.90 | 46.20 ± 24.45 |
Non-parametric distribution.
Abbreviations: %pred, percentage of predicted; cmH2O, centimeters of water; FEV1, forced expiratory volume in the first second; FVC, forced vital capacity; HRR, heart rate recovery in the first and second minutes; MEP, maximum expiratory pressure; MIP, maximum inspiratory pressure; MLHFQ, The Minnesota Living with Heart Failure Questionnaire; T1/2 50 %, recovery time to reach 50 % of VO2peak; VE/VCO2, ventilatory equivalent for carbon dioxide; VE/VCO2slope, ventilatory equivalent for carbon dioxide slope; VO2peak, peak oxygen consumption; VO2VT1, maximal oxygen uptake at the first ventilatory threshold; VT1, first ventilatory threshold; W, watts.
The Supplementary material (Table S2) shows the differences in Glittre-ADL variables between groups. Overall, 33 participants presented low FC.
The effect size was calculated for variables that were significantly different between groups: PBF of 0.85, LVEDD of 0.59, LVESD of 0.70, and LVEF of 0.85.
Reproducibility and MDCThe Bland-Altman method (Fig. 3) demonstrated a bias of 9.1 (95 % CI 7.4, 10.8), lower limit of −12.4 (95 % CI −15.3, −9.5), upper limit of 30.6 (95 % CI 33.9, 27.3), and possible learning effect of 9.2 % in some patients. The analysis showed that the bias between the two repeated measurements of Glittre is different from zero: t (41) = 5.385; p-value <0.0001. The correlation coefficient of ADL-time between test and retest was 0.83 (p < 0.001) with an effect size (r2) of 0.69.
The relative reliability (ICC between two scores) was 0.841 (95 % CI 0.454, 0.936; p < 0.001), while absolute reliability (intra-subject variability) was 3.2 % (calculated from SEM of 8.35). MDC95% was 8.8 % (23.1 s), reflecting the magnitude of the change that was not due to a random variation or measurement error. The following result was found for concurrent validity, rho = −0.484 (95 % CI: −0.642 to −0.287; p < 0.0001).
DiscussionThis study is the first to establish the MDC95% and a cutoff point for FC assessment in patients with HF using the Glittre-ADL test. The Glittre-ADL test showed good reproducibility and was useful in assessing FC in patients with HF and reduced EF.
Glittre-ADL test - cutoff pointThe Glittre–ADL test is easy to apply and well-accepted by patients because it directly reflects daily activities and limitations. Limitations in ADLs may impact the economic, sexual, and psychosocial domains of patients with HF and contribute to physical inactivity and high hospitalization rates.25
Our data allowed establishing a cutoff point of 255 s using the Glittre-ADL test and based on VO2peak. We highlight that the cutoff point of 16 ml/kg/min was chosen because patients with HF using beta-blockers and presenting VO2peak below this value are considered very severe and with worse mid-term prognosis, regardless of etiology and cardiac function. This information was confirmed in a five-year survival analysis study conducted with 391 patients.14
Three studies applied the Glittre-ADL test to patients with heart disease. Valadares et al.26 observed a moderate association between ADL-time of 10 patients with HF and left ventricular function, and their distance covered in the 6 min walk test, dyspnea, and quality of life. In another study, Olímpio Júnior et al.27 assessed eight patients with HF and found an association between ADL-time and VE/VCO2slope; the latter provides an important prognosis of mortality in patients with HF.2
Our group recently observed that patients with advanced HF had a poor performance in the Glittre-ADL test.28 These results and the cutoff point determined in the current study suggest that the Glittre-ADL test is feasible for patients with HF.
Testing for the cutoff point found may be a fast and low-cost option to help adjust treatments and determine prognosis, considering future incorporation of ADLs assessment for managing patients with HF.29 Moreover, most ADLs are performed at submaximal FC, and evidence showed that the results obtained in these tests might better reflect limitations in ADLs than maximal tests.30 A cohort study with 1128 patients with HF reported that patients with moderate to severe difficulty performing ADLs presented a 57 % risk of hospitalization.31
Regarding ADL-time, Valadares et al.26 reported an average time of 390 s, which is higher than observed in our study. This difference may be due to the study population because those authors only included patients aged > 40 years and with NYHA functional classes III and IV. In contrast, recent evidence showed an average time of 279 s on the Glittre-ADL test for patients with HF (NYHA functional class II and III) and reduced or preserved EF.27
Studies with healthy individuals found an average ADL-time of 200 (adults)32 and 210 (older adults) seconds.30 Considering a cutoff point of ≥ 255 s for low FC, we infer that the Glittre-ADL test can differentiate FC between patients with HF and healthy individuals. This cutoff point may also indicate individuals with worse lung function and respiratory muscle strength.
Reproducibility and MDC95 %Measurement instruments should be reliable and report accurate, consistent, and reproducible results. Good test-retest reliability was found in our study, similar to that in patients with obstructive sleep apnea (ICC = 0.865),33 cystic fibrosis (ICC = 0.849),34 and chronic obstructive pulmonary disease (ICC = 0.95).35 Despite producing discordant measurements (bias of 9.1 % different from zero), reproducibility must be understood through its various measurements, and the test presents excellent reliability. However, the difference between test-retest must be considered in clinical relevance, if we consider the MDC of 23 s, future studies may clarify this point.
The reproducibility of Glittre-ADL test was also studied in patients with chronic obstructive pulmonary disease, and a decrease of 22 s in ADL-time of the retest was observed due to a 7 % learning effect.9 In another study, Reis et al.32 reported a 6 % learning effect in healthy individuals, similar to our study. Hospitalized patients with exacerbated acute and chronic pulmonary disease (ICC = 0.91) also presented a better performance in the retest (42-second difference) due to the learning effect.36
Based on MDC95 % (23.1 s), the Glittre-ADL test is applicable for patients with HF. However, we recommend at least two tests due to the possible learning effect.
The concurrent validity result showed that there is a negative/inverse and moderate correlation between the total Glittre time and VO2peak; that is, as VO2peak decreases, total Glittre time increases. Therefore, it is possible to state that Glittre is a valid test for patients with HF, as the total time to complete it is an adequate reflection of the gold standard, a fact already demonstrated in a previous study by our group.28
The Glittre-ADL test is an easy, fast, and low-cost test that requires little physical space. In addition, it comprises ADLs and includes all the main muscle groups of limbs and trunk. Therefore, it may be reproducible and used in patients with HF. The study's limitation is the absence of elderly people and NYHA functional class IV patients, therefore future studies are needed to confirm our findings in this population.
ConclusionThe cutoff point established for the Glittre-ADL test can be used in clinical practice to identify patients with severe HF when CPET is not available, while the MDC95 % can help identify the effectiveness of treatments to improve FC. Also, we recommend performing two Glittre-ADL tests due to the possible learning effect. Although the Glittre-ADL test proved to be another reproducible submaximal test capable of predicting the prognosis of patients with HF, we observed a systematic error possibly related to the learning effect.
The authors thank Provatis Academy for providing scientific language translation, revision, and editing.