To study the adherence of an Early Inpatient Exercise Program in patients with acute hip fracture, identify variables associated with its performance, and its association to one-year survival.
MethodsObservational longitudinal study of a cohort of 509 patients, admitted consecutively with a hip fracture in La Paz University Hospital (Madrid, Spain). Data included sociodemographic variables, pre-fracture physical functioning, cognitive impairment, comorbidities, measure of exercise adherence (pre-surgery exercise, post-surgery exercise, and rehabilitation sessions) and vital status at follow-up. One year after the fracture, either patients or relatives were contacted by telephone to ascertain their vital status. Data were analyzed using logistic regressions and multivariate Cox proportional hazards regression.
ResultsThree quarters of patients (76.0%) were able to comply with the Early Inpatient Exercise Program. Factors associated with adherence were: living at home (Odds Ratio (OR)=3.39; 95% Confidence Interval (CI): 2.03, 5.64), absence of pre-fracture disability (OR=3.78; 95% CI: 2.21, 6.47), absence of pre-fracture cognitive impairment (OR=2.36; 95% CI: 1.36, 4.07) and comorbidities (OR=1.66; 95% CI: 1.03, 2.67). Early Inpatient Exercise Program adherence was associated with one-year survival (HR=1.62; 95% CI: 1.06, 2.49).
ConclusionsThe adherence with an Early Inpatient Exercise Program is high and is associated with 1-year survival. It is important to make a stronger effort to encourage participation in Early Inpatient Exercise Program in the 24% currently non-compliant, and in those with cognitive and physical impairments.
The observed increase in hip fractures among the elderly is inherently associated with the increase in longevity experienced worldwide. As a result of the changes in the population pyramid, projections have indicated that the number of people aged 80 or over will rise to 425 million by 2050.1
Currently, there is minimal data on the incidence of hip fracture in Latin America, but according to the International Osteoporosis Foundation, the hip fracture incidence in these regions is 178/100000 persons aged 50 years and older.2 It is expected that the number of older adults between 2017 and 2050 will increase by 161% in this region.1 The European Union comprises countries with some of the highest hip fracture rates, with an incidence around 200/100000.3
Hip fractures lead to significant mortality, morbidity and disability.4–6 As people age, the risk of sustaining a hip fracture increases5 and more people will require assistance with functionality and mobility through rehabilitation services and more precisely, physical therapy (PT).7 PT plays an important role in acute-care centers by helping plan patients discharge and ensuring that patients’ mobility is adequate at the time of discharge. In addition, PT reduces the negative impact of any period of inactivity during the acute part of the process that can lead to muscle atrophy, loss of movement range and fitness reduction.8 PT helps to restore function9 and decrease the mortality risk10 in older people who have suffered a hip fracture.
Presently, there is no standard PT protocol for hip fracture patients,5,6 however, clinical practice guidelines that have been designed for patients with hip fracture recommend that rehabilitation for these patients should be focused on carrying out early mobilization exercises after hospital admission.5,6,11 These exercises must centre on gradually improving strength/power in the knee extensor and hip flexor muscles,6,11 combined with balance exercises in order to maximize functional recovery9,11 and decrease the risk of future falls and fractures.6
In order to achieve the expected PT results, appropriate exercises must be performed correctly and consistently supported by the nursing team as they are more likely to be in contact with the patients and to offer essential help in the execution of the exercise program.12
It should be noted that the recovery process for patients who have suffered a hip fracture is a multifactorial process where knowledge of the patient's previous functional status is essential, but it is also important to have knowledge of all psychosocial factors such as family and caregiver support available for them during hospitalization and after discharge.12
In this paper, the authors examine the adherence of patients with a hip fracture to an Early Inpatient Exercise Program (EIEP) from the time of hospital admission and throughout the post-surgical period. The EIEP consisted of active and passive exercises in both supine and seated positions plus weight bearing exercises.
The aim of this paper was to study the adherence to EIEP in patients with acute hip fracture and to identify variables associated with patient's performance, and the association between adherence and one-year survival.
MethodsStudy designA descriptive observational longitudinal study
MethodsThe study sample consists of a cohort of 509 patients with a diagnosis of hip fracture consecutively hospitalized in La Paz University Hospital (Madrid, Spain) between 25 January 2013 and 24 February 2014. More details can be found in previous studies on this cohort (FONDA cohort).13–15 Patients were assessed in the orthogeriatric unit by an interdisciplinary team (i.e. geriatrician, orthopedic surgeon, and a geriatric nurse), before surgery and within the first 72h of admission and again 24h before discharge. The average hospital length of stay among this population was 10.1 ± 5 days.13 At discharge, only 3.3% of patients could independently walk and 79.8% needed help to be able to walk.13 The rest did not walk at all (17%). One year after discharge, patients or their family members were contacted by telephone to ascertain their vital status.14
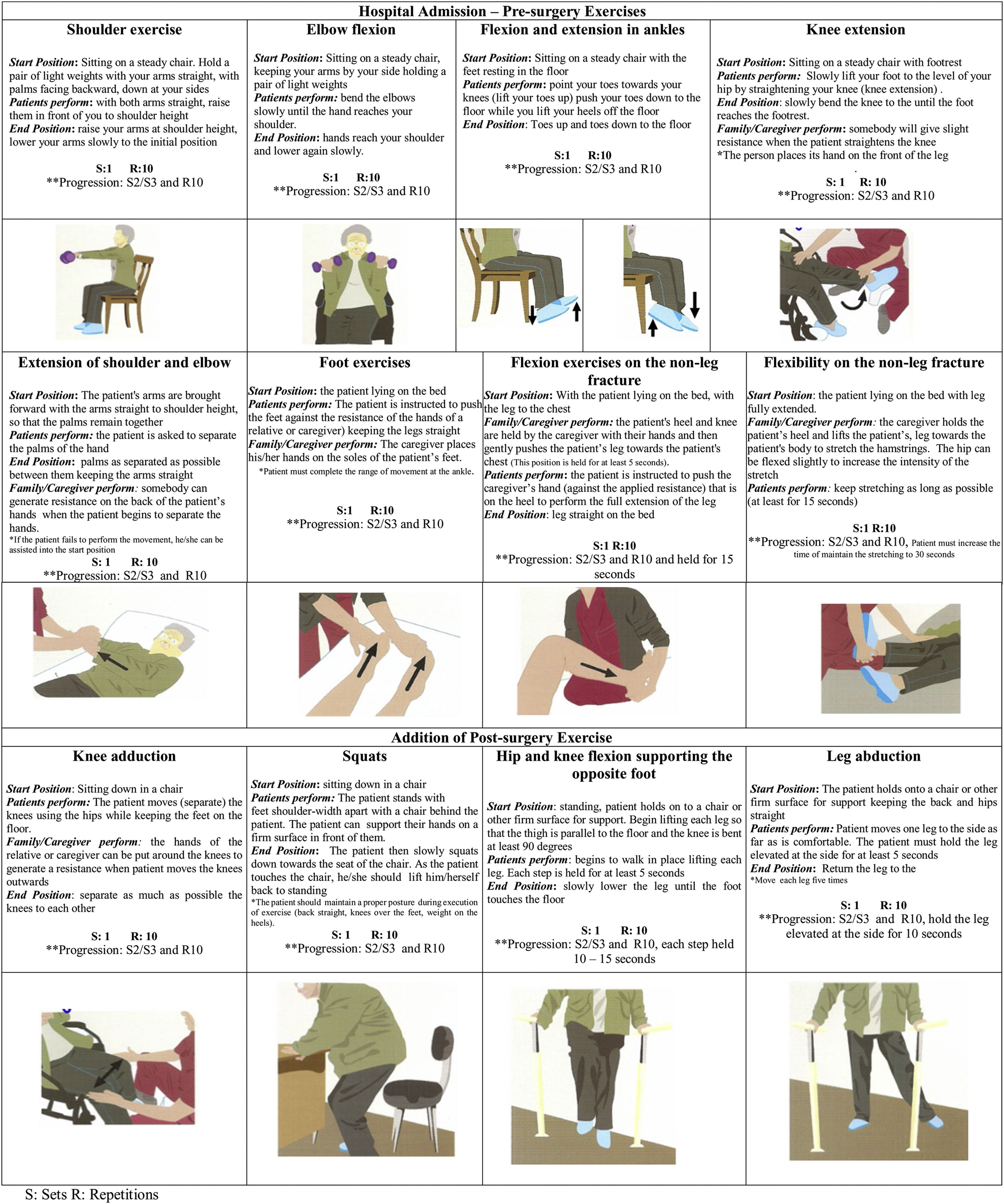
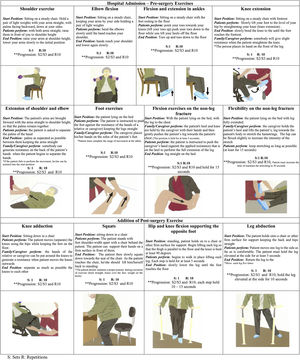
The Orthogeriatric Unit has developed an Early Inpatient Exercise Program (EIEP), consisting of six active and passive exercises for the upper limbs and the lower limb not affected by the fracture. These are performed pre-surgery once a day in bed or sitting on a chair and, in a standing position post-surgery. On the day of admission, both the patient and family members received an information sheet (Fig. 1) with the EIEP exercises, which are explained to them by a geriatric nurse. This exercise program contained the exercises the patient had to perform with the assistance of hospital staff, a family member, or a caregiver. Patients were told to start with 10 repetitions of each exercise and increase progressively until reaching 30 repetitions every day.
In addition, the patients received additional sessions with a physical therapist after surgery. The PT sessions focused on gait rehabilitation exercises using a walker. Each session lasted 15min every day except for weekends (i.e. 5 days/week) and were always under a physical therapist's supervision. Ninety five percent of the patients were able to participate in the physical therapy weight-bearing exercises. In all cases, they exercised with a walker until they were discharged. By the time they were discharged from the hospital, the same information sheet was given to them to continue practicing the same exercises they were practicing in the hospital. Patients were asked and encouraged to continue performing all exercises after they were discharged.
An informed consent form was obtained from all patients or relatives before they were included in the study. The study was approved by the Clinical Research Ethics Committee of La Paz University Hospital, Madrid, Spain (Reference HULP-PI-1334).13
Study variablesDependent variablesTo address the objectives of the study, two main variables were defined: (a) EIEP adherence and (b) 1-year survival
- a)
Adherence was viewed not only as a prescription requirement made by a healthcare professional but as a variable based on the collaborative, active and ongoing patient participation and his immediate support group (i.e. family and caregivers).16,17 It was defined as meeting at least two of the three following criteria: (1) Pre-surgery exercise program adherence; (2) Post-surgery exercise program adherence; and (3) having had two or more PT sessions with a physical therapist after surgery.
- b)
The outcome of primary interest was overall survival after one year, which was defined as the time from fracture until death from any cause within the 1-year period. Vital status and date of death (if deceased) were collected by telephone one year after the fracture from patients or their relatives.14
During the hospital stay, data on factors potentially relevant to recovery were collected: (1) Living arrangements before the hip fracture (i.e. patient living in a nursing home or in his/her own home); (2) Pre-fracture or previous disability was assessed using the Barthel-100 Index with a score of over 60 as the cut-off point for disability15; (3) Comorbidities were assessed using the Charlson Comorbidity Index with a cut-off point of 2 that indicates the presence of comorbidities14; (4) Cognitive impairment at time of admission was assessed using the Pfeiffer questionnaire, which defined the presence of cognitive impairment as a score >3.14
Statistical analysisCategorical variables were described with absolute and relative frequencies. For quantitative variables, the mean, standard deviation and range were calculated. The statistical association of each variable with EIEP adherence was calculated using the chi-squared test for categorical variables and with Student's test for quantitative variable. To identify variables associated with adherence to the EIEP, bivariate logistic regression analyses was run. In these models, age was included as a continuous variable whereas the rest of the factors were entered as dichotomies. Variables showing an association with EIEP adherence were included in a multivariate logistic regression.
The quality of adjustment of the final models was assessed using the Hosmer–Lemeshow statistic and the Nagelkerke coefficient of determination. The final model included those variables with p-value <0.05.
The association between adherence in the EIEP and survival was evaluated using a multivariate Cox proportional hazards regression, including age and sex and all variables associated with EIEP adherence. In a preliminary analysis, the type of living arrangement was observed to not be associated with survival in bivariate analyses, but it became a strong predictor of survival in multivariate analyses. This suggested a possible interaction effect between the type of living arrangement and some of the variables in the model. Next, all product terms between types of living arrangement and each covariable in the model was tested. The type of living arrangement was then hypothesized as a modifier of the effect of adherence to the exercise program. The association between adherence to the EIEP and survival was assessed by fitting two multivariate Cox proportional hazards regressions, stratifying by type of living arrangement and including age, sex, disability, cognition and comorbidity.
Statistical significance was set at two-sided p<0.05. Graphic and model-based techniques confirmed that the proportional hazards assumption was not violated. Analyses were performed using IBM SPSS Statistics for Windows 23 (IBM Corp. 2014, Armonk, NY: IBM Corp).
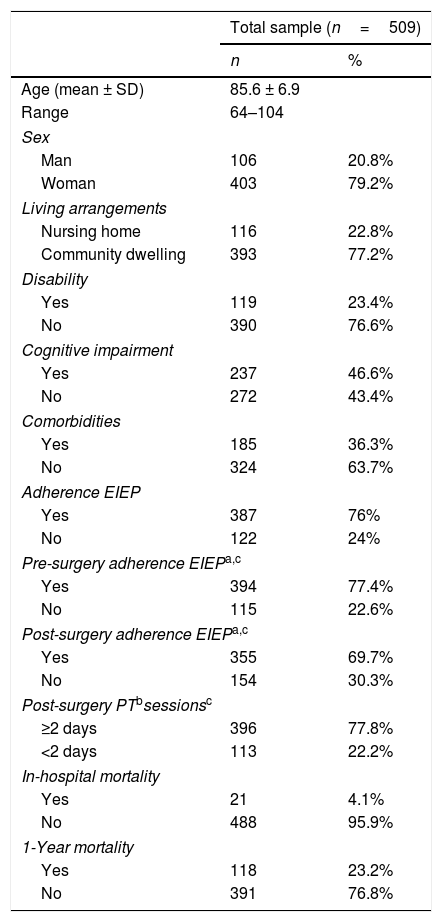
ResultsThe mean age for the cohort was 85.6 years (range: 64–104 years) and most patients were women (79.2%). Three quarters of patients (76.0%) were able to adhere to the EIEP according to the criteria described in the methods section. Table 1 shows the characteristics of the 509 hip fracture patients.
Main characteristics of the patients with hip fracture in a study looking at factors affecting exercise program adherence.
| Total sample (n=509) | ||
|---|---|---|
| n | % | |
| Age (mean ± SD) | 85.6 ± 6.9 | |
| Range | 64–104 | |
| Sex | ||
| Man | 106 | 20.8% |
| Woman | 403 | 79.2% |
| Living arrangements | ||
| Nursing home | 116 | 22.8% |
| Community dwelling | 393 | 77.2% |
| Disability | ||
| Yes | 119 | 23.4% |
| No | 390 | 76.6% |
| Cognitive impairment | ||
| Yes | 237 | 46.6% |
| No | 272 | 43.4% |
| Comorbidities | ||
| Yes | 185 | 36.3% |
| No | 324 | 63.7% |
| Adherence EIEP | ||
| Yes | 387 | 76% |
| No | 122 | 24% |
| Pre-surgery adherence EIEPa,c | ||
| Yes | 394 | 77.4% |
| No | 115 | 22.6% |
| Post-surgery adherence EIEPa,c | ||
| Yes | 355 | 69.7% |
| No | 154 | 30.3% |
| Post-surgery PTbsessionsc | ||
| ≥2 days | 396 | 77.8% |
| <2 days | 113 | 22.2% |
| In-hospital mortality | ||
| Yes | 21 | 4.1% |
| No | 488 | 95.9% |
| 1-Year mortality | ||
| Yes | 118 | 23.2% |
| No | 391 | 76.8% |
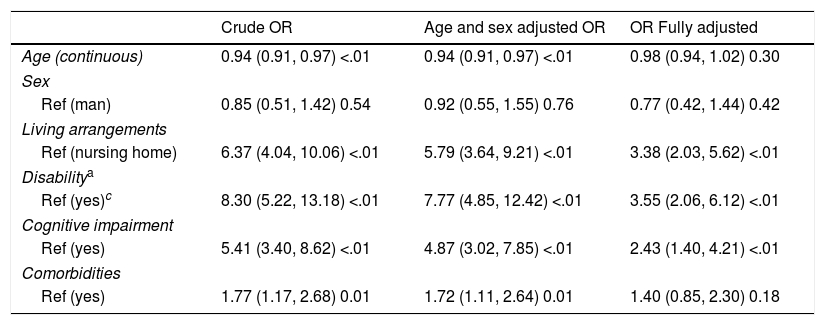
Table 2 displays the multivariate logistic regression results. In this cohort, EIEP adherence was independently associated with living at home before the fracture (OR=3.39; p<0.001), absence of pre-fracture disability (OR=3.78; p<0.001), absence of pre-fracture cognitive impairment (OR=2.36; p=0.002), and no comorbidities (OR=1.66; p=0.03). EIEP adherence was unrelated to patient age or sex.
Logistic regression results regarding variables associated with Adherence of Early Inpatient Exercise Program for hip fracture patients.
| Crude OR | Age and sex adjusted OR | OR Fully adjusted | |
|---|---|---|---|
| Age (continuous) | 0.94 (0.91, 0.97) <.01 | 0.94 (0.91, 0.97) <.01 | 0.98 (0.94, 1.02) 0.30 |
| Sex | |||
| Ref (man) | 0.85 (0.51, 1.42) 0.54 | 0.92 (0.55, 1.55) 0.76 | 0.77 (0.42, 1.44) 0.42 |
| Living arrangements | |||
| Ref (nursing home) | 6.37 (4.04, 10.06) <.01 | 5.79 (3.64, 9.21) <.01 | 3.38 (2.03, 5.62) <.01 |
| Disabilitya | |||
| Ref (yes)c | 8.30 (5.22, 13.18) <.01 | 7.77 (4.85, 12.42) <.01 | 3.55 (2.06, 6.12) <.01 |
| Cognitive impairment | |||
| Ref (yes) | 5.41 (3.40, 8.62) <.01 | 4.87 (3.02, 7.85) <.01 | 2.43 (1.40, 4.21) <.01 |
| Comorbidities | |||
| Ref (yes) | 1.77 (1.17, 2.68) 0.01 | 1.72 (1.11, 2.64) 0.01 | 1.40 (0.85, 2.30) 0.18 |
OR, Odds Ratio and 95% confidence interval, with associated p-value.
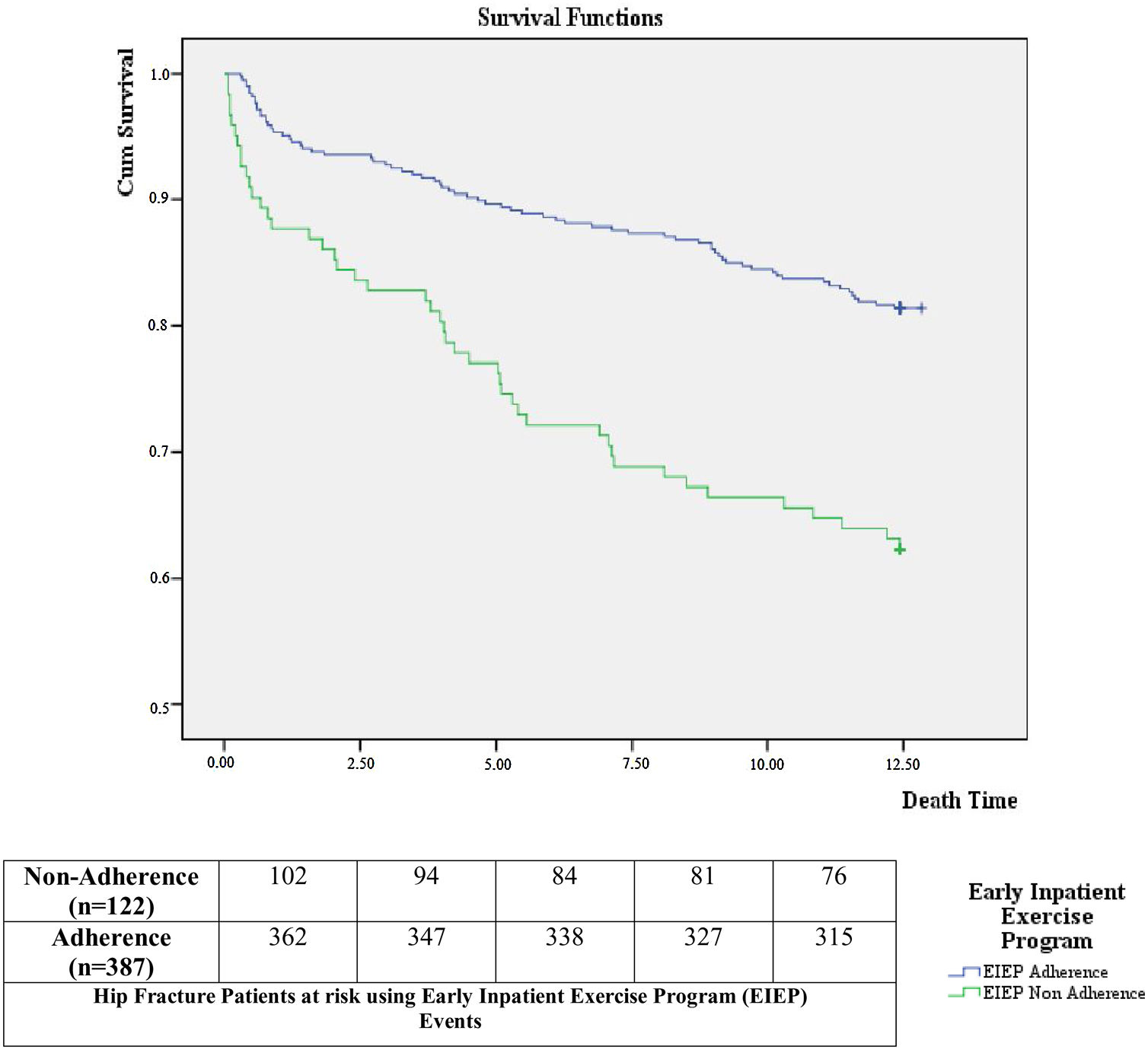
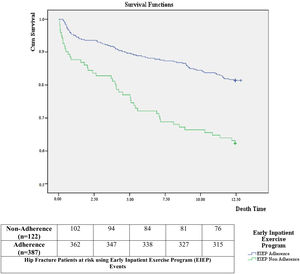
The 1-year mortality rate among patients who complied with the EIEP was 18.6%, while mortality rate reached 37.7% among those who did not adhere to the EIEP.
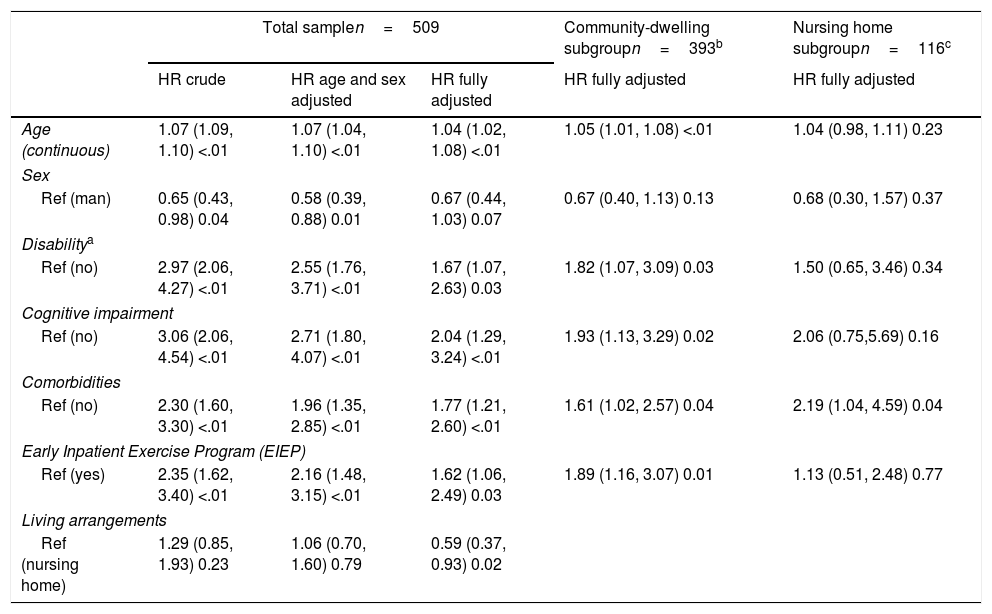
Table 3 shows the crude hazard ratios (HR), age and sex adjusted HR and fully adjusted HR (with 95% confidence intervals (CI) for the variables associated with survival. In the crude HR and age and sex adjusted data, all independent variables but living arrangement (i.e. community or nursing home) were associated with 1-year mortality. In the fully adjusted model, all variables (including living arrangement) except sex were associated with 1-year mortality in the total sample. After stratifying by type of living arrangement, the association of the different independent variables with mortality was maintained in the community-dwelling group of people. Adherence to the EIEP was associated with survival only in the community-dwelling patients. In patients living in a nursing home, the coefficient of adherence was not statistically significant although adherence remained positively associated with survival. The results of this additional sensitivity analysis were incorporated in Table 3 (columns 4 and 5).
Cox proportional-hazards regression. Variables associated to survival at 1-year for hip fracture patients.
| Total samplen=509 | Community-dwelling subgroupn=393b | Nursing home subgroupn=116c | |||
|---|---|---|---|---|---|
| HR crude | HR age and sex adjusted | HR fully adjusted | HR fully adjusted | HR fully adjusted | |
| Age (continuous) | 1.07 (1.09, 1.10) <.01 | 1.07 (1.04, 1.10) <.01 | 1.04 (1.02, 1.08) <.01 | 1.05 (1.01, 1.08) <.01 | 1.04 (0.98, 1.11) 0.23 |
| Sex | |||||
| Ref (man) | 0.65 (0.43, 0.98) 0.04 | 0.58 (0.39, 0.88) 0.01 | 0.67 (0.44, 1.03) 0.07 | 0.67 (0.40, 1.13) 0.13 | 0.68 (0.30, 1.57) 0.37 |
| Disabilitya | |||||
| Ref (no) | 2.97 (2.06, 4.27) <.01 | 2.55 (1.76, 3.71) <.01 | 1.67 (1.07, 2.63) 0.03 | 1.82 (1.07, 3.09) 0.03 | 1.50 (0.65, 3.46) 0.34 |
| Cognitive impairment | |||||
| Ref (no) | 3.06 (2.06, 4.54) <.01 | 2.71 (1.80, 4.07) <.01 | 2.04 (1.29, 3.24) <.01 | 1.93 (1.13, 3.29) 0.02 | 2.06 (0.75,5.69) 0.16 |
| Comorbidities | |||||
| Ref (no) | 2.30 (1.60, 3.30) <.01 | 1.96 (1.35, 2.85) <.01 | 1.77 (1.21, 2.60) <.01 | 1.61 (1.02, 2.57) 0.04 | 2.19 (1.04, 4.59) 0.04 |
| Early Inpatient Exercise Program (EIEP) | |||||
| Ref (yes) | 2.35 (1.62, 3.40) <.01 | 2.16 (1.48, 3.15) <.01 | 1.62 (1.06, 2.49) 0.03 | 1.89 (1.16, 3.07) 0.01 | 1.13 (0.51, 2.48) 0.77 |
| Living arrangements | |||||
| Ref (nursing home) | 1.29 (0.85, 1.93) 0.23 | 1.06 (0.70, 1.60) 0.79 | 0.59 (0.37, 0.93) 0.02 | ||
Disability – Barthel-100 Index score >60 HR: hazard ratio.
In this table, the HR (95% confidence interval) and associated p-value of the total sample (n=509) is shown in the first three columns. The last two columns show the final adjusted model HR when the stratification by living arrangements was used. The analysis was performed with this stratification because living arrangement was a cofounder variable to disability, cognitive impairment and comorbidities.
Fig. 2 shows the survival curves comparing patients with and without EIEP adherence in the fully adjusted Cox regression model. Patients with EIEP adherence had better survival outcomes than those who failed to meet the adherence criteria (p<0.001).
DiscussionBased on the results, three quarters of acute hip fracture patients were able to fully adhere to the early inpatient exercise program (EIEP).
The results support previous studies examining potential predictors of favorable recovering after having suffered a hip fracture. Previous work identified that pre-fracture functional physical and cognitive status,18,19 as well as age, comorbidities, and pre-fracture living arrangements were key variables to maximizing results. Hulsbæk et al.19 mentioned that patients with low pre-fracture function and who were older, as well as having several comorbidities and low cognitive status were not able to complete physical therapy on the first postoperative day.19 Additionally, Vochteloo et al.20 found that residing at home versus living in a nursing home before the fracture predicted a better rehabilitation outcome, due in part to the fact that healthier and more active older individuals were more likely to live at home.20
Factors mentioned in the previous section were relevant to the physical therapist at the start of the rehabilitation process because they provide an important point of reference on the degree of adherence that can be achieved with the patients. Adherence is a multifactorial concept widely used in medicine.21 It is also a major part of any recommended treatment, where there is an active and dynamic relationship between the professional and the patient and his/her environment.16,17 In our research, the health professionals, and patients (including family and caregivers) were encouraged to explain and perform the exercises during the acute phase to decrease the impact of physical deconditioning generated by prolonged periods of inactivity.22
The exercises proposed in the EIEP were focused on (a) lower limb and upper limb movements, to decrease the impact of immobility,22 (b) weight bearing exercises for the operated leg, to be started the day after the surgery according to the patient's tolerance,5,11 (c) progressive strength training for the lower limbs to increase resistance and strength in the hip flexion muscles, which are involved during walking activity,6,11 (d) balance training to improve balance and prevent falls.11
The pre-surgical exercises, which were part of the adherence of the EIEP has shown a participation rate in 2/3 of our patients. According to the literature, the importance of early mobilization has been discussed, but following surgery,5,6,11 not before.23 There were no papers that mentioned exercise or some type of specific mobilization before surgery. We regard it to be vitally important to have patient's exercising before the surgery to decrease the homeostatic balance generated by prolonged immobilization due to the fracture and the pain. This kind of exercises could help to optimize the intervention of the physical therapist and improve the functional outcomes for these patients at the start of the rehabilitation process.22 It should be emphasized that patients who performed PT were more likely to regain physical function and quality of life faster than those who did not adhere to a physical therapy program.24
Our results show that adherence to a post-surgery exercise program was a little less than adherence to a pre-surgery exercise program (69.7% vs 77.4% respectively). It appeared that the situation of patient being in bed after surgery reduced his/her participation. From the family perspective, the family may not have realized the importance of the exercise information sheet. On the other hand, the third criterion that involved the PT sessions, where the daily activity of walking with a walker was performed in the patient's room for 15min was performed as required by the study. The importance of the physical therapy session where emphasis was placed on early ambulation with the use of external aids to encourage the patient to return to his/her environment and recover his/her previous functional status as soon as possible was also an important component of recovery. With respect to this item within the variable dependent on adherence, it was met in a similar proportion to the presurgical program.
Even though the adherence to EIEP was high, our research showed that 24% of patients did not participate in the exercise program, most of these patients had cognitive or physical impairments. It must be kept in mind that patients who have physical or cognitive limitation often need significant support to increase their adherence to EIEP. This implies that rehabilitation services must be able to adapt to the needs of all patients to achieve a common goal that is to improve mobility and quality of life.25
The orthogeriatric units play an important role in the treatment and recovery of these types of patients. Due to patients’ characteristics that are related to age, such as, comorbidities, frailty, and polypharmacy, a multidisciplinary team of geriatricians, orthopedic surgeons, physical therapists and specialized nurses are needed to get these goals.26 The high percentage of EIEP adherence in this study was related to the study being done in an orthogeriatric unit.
Previous research has supported the view that exercise in rehabilitation can reduce mortality as much as medical complications and health-related costs.27 Additionally, Kronborg et al.24 stated that early mobilization following hip fracture surgery reduced medical complications including mortality.24 Our results reinforced the idea that an early exercise program in a hospital before discharge improves 1-year survival in community dwelling patients. This association between an early exercise program and survival was also observed in nursing home patients but the association did not reach statistical significance. The probability of death was 53% lower in community dwelling patients who had completed the early exercise program compared with those who had not completed it.
Several clinical guidelines and previous research on hip fracture management showed that all the following variables impacted on recovery and mortality risk: age, sex, time between hospital admission and surgery, degree of surgical risk, pre-fracture functional status, cognitive impairment, pre-surgery complications, PT plan, and home support.26–28 In the case of patients with cognitive impairment, Resnick et al. mentioned that this type of patient was not exposed to the same amount and kind of treatment compared to patients with no cognitive impairment.25
In line with literature, our result should be interpreted in the context of the study's limitations. First, there was no control group available to test the effect of the exercise intervention. Literature has demonstrated that early exercise is beneficial for recovery,7,22 it would be unethical to withhold the program from a group of patients. Second, another limitation that our study presented is that statistical models did not take into consideration factors such as the nutritional status, frailty, depression or psychosocial support at the time of the event, nor the functional status of the patient at discharge. Instead, the group of patients who did not adhere to the exercise program served as the comparison group after adjusting for their pre-fracture physical status, cognitive impairment, or previous living accommodation status, within de Cox multivariate regression methodology.
This study also had some important strengths. First, given that the data were collected from the only major public hospital serving an area of 500000 individuals, our sample could be considered a population-based sample since they were likely to closely mirror all hip fracture patients in a large area of Madrid. In Spain, a country with a well-regarded and functioning universal health care system, most people choose major public hospitals for major surgeries even if they have additional private health insurance. Thus, the results might be applicable to other areas of Spain. In addition, the study shared many of the strengths found in studies showing that exercise performed in a hospital not only after surgery8,29 but also before surgery resulted in a positive outcome. However, it is worth mentioning that our literature review did not uncover any other study assessing the effects of pre-surgery exercises involving mobilization, isometric exercises or flexibility exercises on this specific type of patient. Our patients received visual aids (Fig. 1) for these exercises and were instructed to perform them before as well as after surgery. Thus, we may be the first to report on the effects of this type of pre-surgery exercise program for patients with hip fracture
ConclusionsThe adherence to the EIEP among patients with acute hip fracture was significantly higher in patients admitted from the community and with no impairment. Only 24% of the patients admitted in our orthogeriatric unit did not adhere with the proposed exercise program, most of whom had cognitive and/or physical impairments. The adherence to the EIEP was associated with 1-year survival. Therefore, measures to ensure that patients with some physical and/or cognitive impairment should be implemented because these types of patients could benefit in the same way as patients who do not have these limitations.
Conflicts of interestThe authors declare no conflicts of interest.
We thank Juan José de la Cruz Troca (Preventive Medicine Department, Universidad Autónoma de Madrid, Madrid, Spain) for his invaluable help with the statistics.