Contradictory evidence exists regarding the clinical course of frozen shoulder (FS).
ObjectivesTo explore the clinical course of FS regarding disabilities, pain, range of motion (ROM), muscle strength, scapular upward rotation, and proprioception and to establish longitudinal correlations between these variables.
MethodsPatients with FS were prospectively followed for 9 months at 3-month intervals. Assessment included the Disabilities of the Arm, Shoulder and Hand questionnaire; visual analogue scale for pain; an inclinometer for shoulder external rotation (ER), internal rotation (IR), flexion, and abduction ROM, and scapular upward rotation and proprioception, as well as handheld dynamometry for muscle strength in shoulder abduction, ER, and IR.
ResultsInitially, 149 patients (98 females; mean (SD) age 53 (9) years) were included, with 88 completing all follow-up assessments. Most variables showed early improvement in the clinical course of FS, particularly ER and IR at 90° abduction, which continued to improve from 6 to 9 months of follow-up. Associations were observed between disabilities and pain (r = 0.61), disabilities/pain and ROM (r=-0.62 to -0.59 and r=-0.47 to -0.39, respectively), disabilities/pain and muscle strength (r=-0.24 to -0.35 and r=-0.36 to -0.17, respectively), and between disabilities/pain and scapular upward rotation below shoulder level (r = 0.23 to 0.38 and r = 0.24 to 0.30, respectively). ROM correlated with muscle strength (r = 0.14 to 0.44), while both ROM and ER muscle strength correlated with scapular upward rotation below shoulder level (r=-0.37 to -0.23 and r=-0.17 to -0.12, respectively). Muscle strength correlated with scapular upward rotation above shoulder level (r = 0.28 to 0.38) and lift-off muscle strength correlated with joint repositioning (r=-0.17 to -0.15).
ConclusionAlmost all factors improved in the early phase (3–6 months) after baseline assessment, while ER and IR ROM at shoulder level continued to improve long term.
Frozen shoulder (FS) is a condition characterized by severe shoulder pain and functional restriction of both active and passive shoulder motion.1 The prevalence of primary FS in the general population is 2–5%.2 Frozen shoulder usually develops between the age of 40 and 60 years3 and affects more women.3,4 Multiple factors might contribute to the clinical picture of FS and explain its variable prognosis.5
Formerly, the clinical course of FS was often described as self-limiting, with recovery within 1 to 3 years, with most recovery in the later stages.6 In contrast, Wong et al.,7 in their systematic literature review, found moderate evidence for an improvement in range of motion (ROM) and shoulder disability in the early stages, which slows with time.7 Unfortunately, this review used a non-validated risk of bias tool and only included studies with small cohorts (<60 patients), reducing the certainty of the results.
When considering the multiple clinical factors in patients with FS, ROM restriction has been related to higher levels of perceived pain and increased disability,8,9 while perceived pain has been related to disability.9,10 Additionally, patients with FS try to compensate for glenohumeral joint ROM restriction with increased scapular upward rotation.11 Although contractile tissue is not expected to be impaired in patients with FS,12 a decrease in muscle strength may be associated with other factors. Only one study assessed the association between muscle strength and disabilities in patients with FS after treatment and did not find a meaningful correlation.10 Proprioceptive function may be affected by high pain intensity and potentially improve as pain decreases.13 It is clear that different functional impairments are associated, but inconsistent findings and the lack of knowledge regarding correlations over time, pose a challenge.8-11 Understanding how change in one factor (e.g., ROM) leads to change in another factor (e.g., scapular upward rotation) could provide important information to explain the clinical course of the condition.
The primary aim of the current study was to explore the clinical course of FS over a 9-month period after baseline assessment regarding self-reported shoulder disabilities, pain intensity, ROM, muscle strength, scapular upward rotation, and proprioception. The secondary aim was to establish direct longitudinal (i.e., over time) correlations between these functional outcomes measured at multiple time points.
MethodsStudy designA multicenter prospective longitudinal observational study was performed in the research laboratories of the authors’ affiliations and was reported following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)-checklist.14 The study was approved by the Human/Clinical Research Ethics Committees of the University of Valencia (H1432625002427), Hospital Costa del Sol (001_abr17_PI2), and University Hospital Antwerp (B300201422072). Data were prospectively collected between November 2014 and October 2020. The current study adhered to the Declaration of Helsinki. Written informed consent was obtained by all participants prior to making all measurements.
ParticipantsPatients with FS were recruited at the orthopedic departments of different hospitals and through general practitioner practices in cities of the authors’ affiliations. Patients were included if: a) they had FS at stage 1 or 2 according to Hannafin and Chiaia4 (duration of symptoms <9 months, pain with active and passive ROM, and significant limitation of ROM for shoulder flexion, abduction, internal rotation (IR), and external rotation (ER)); b) they had passive ROM restriction of at least 25% in at least two movement planes and 50% in glenohumeral ER compared to the unaffected shoulder (in total three movement planes)15; c) pain and movement restriction were present for at least one month that reached a plateau or were deteriorating15; d) they were able to understand Spanish or Dutch language.
Patients were excluded if: a) the complaints improved during the last month15; b) they were pregnant or breastfeeding; c) they had any shoulder surgery prior to the development of FS; d) FS occurred because of humerus fractures, dislocation, or cerebrovascular accident.
Outcome measuresFor the determination of the clinical course (primary aim), shoulder disabilities (Disabilities of the Arm Shoulder and Hand (DASH) questionnaire) was the primary outcome measure, while pain intensity (visual analogue scale (VAS)), ROM (shoulder ER, IR, flexion, and abduction), muscle strength (shoulder abduction and ER and IR), scapular upward rotation at different shoulder abduction angles, and shoulder proprioception were secondary outcome measures.
All measurements were repeated at 3-, 6- and 9-months follow-up after baseline assessment. There were two assessors at each center and all assessments of each patient were performed by the same assessor. Assessors were physical therapists with multiple years experience and were trained by a physical therapist with more than 10-years of experience in the examination of shoulder disorders.
Disabilities of the arm, shoulder, and hand (DASH)This questionnaire aims to assess symptoms and functional status (disability) in populations with upper extremity musculoskeletal conditions.16 It consists of 30 items that addresses difficulty in performing physical activities that require upper extremity function, symptoms of pain, activity-related pain, tingling, weakness, and stiffness. These items are scored on 5-item Likert scales, with a total score ranging from 0 (no disability) to 100 (most severe disability). The DASH has been found valid and reliable in Spanish and Dutch.17,18
Visual analogue scale (VAS)Patients were asked to rate their pain on a 10 cm line by drawing a vertical mark. The left end of the line represents ‘No pain’ (0 cm) and the right end ‘Most severe pain’ (10 cm). The scoring is the distance in mm from the left end of the line to the vertical mark of the patient.19 Patients had to rate the average pain of the shoulder during the last week. The VAS has been found valid and reliable.20
Shoulder range of motion (ROM)Shoulder ROM was measured with an analogue inclinometer. An inclinometer has been shown to have a minimal detectable change of 12° to 28° in patients with FS and is a valid tool for assessing shoulder ROM.21 Both active and passive ROM were measured, with active measurements always preceding passive ones. Shoulder ROM was measured for ER (at 0° and 90° shoulder abduction), IR (at 90° shoulder abduction), flexion, and abduction. At baseline both shoulders were measured, and the testing order was randomized. At follow-up measurement, only the affected shoulder was measured. For ER and IR, patients laid supine, and the inclinometer was attached to the dorsal or volar side of the distal forearm.21 In each of the abduction positions, shoulder ER and IR was measured. The 90° shoulder abduction angle was previously determined with the help of a goniometer. Flexion and abduction were measured with patients in a sitting position, with the hips and knees flexed 90° and the feet flat on the floor for stability. The inclinometer was attached to the upper arm, just below the insertion of the deltoid muscle.21 Flexion and abduction movements were performed in the sagittal and frontal plane, respectively, with the thumb pointing upwards.
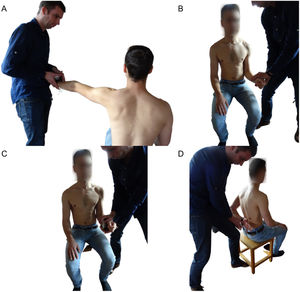
Shoulder muscle strengthShoulder muscle strength was measured using a handheld dynamometer (Microfet 2.0, Hoggan Health Industries Inc., USA). All patients were asked to perform an isometric contraction in three directions (abduction, ER, and IR). During all measurements, patients were sitting with their hips and knees flexed 90° and their feet flat on the floor for stability. Handheld dynamometry has been found reliable and valid for measuring shoulder muscle strength.22 Shoulder muscle strength was measured for both sides at all measurement times. Measurement order for side was randomized. For abduction muscle strength, patients positioned their arm in 90° abduction in the scapular plane with an extended elbow and the thumb pointing upwards.23 The dynamometer was placed at the radial side of the wrist and patients were asked to push against the dynamometer (i.e., make test24). When patients were unable to reach the full can position the test was performed 10° below their maximal shoulder abduction position in the scapular plane. For ER and IR, patients were asked to position their arm at the side with the elbow flexed 90° and the forearm in neutral position (thumb pointing upwards).22 The dynamometer was placed on the dorsal or volar side of the wrist and patients were asked to push (i.e., make test24) the hand outward (ER) or inward (IR). A second shoulder IR measurement was done in the lift-off position (hand-behind-the-back) in those patients who were able to reach this position. Patients placed their hand on the lower back, with the elbow flexed 90° and the forearm in a neutral position (thumb pointing upward).23 The dynamometer was placed on the volar side of the wrist and patients were asked to push against it as trying to move the hand away from the back (i.e., make test24). See Fig. 1 for test positions.
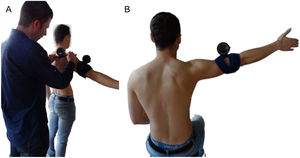
Scapular upward rotationThe measurement of scapular upward rotation was performed by using two inclinometers as previously described by Watson et al.25 One inclinometer was attached to the upper arm, just below the insertion of the deltoid muscle, while the second inclinometer was aligned to the scapular spine. Patients were asked to perform shoulder abduction in the frontal plane with the thumb pointing upward and full extension of the elbow, stopping at 30°, 60°, 90°, 120°, and 150° humerothoracic elevation or their maximal achievable range (Fig. 2A). The scapular upward rotation was measured at each angle of shoulder abduction. This method for measuring scapular upward rotation has been found reliable.25
Shoulder joint proprioceptionShoulder joint proprioception was measured by using a joint repositioning test by means of an inclinometer.26 During this test, patients were sitting with the knees and hips flexed 90° and the feet flat on the floor. They were first asked to move their arm, with the thumb pointing upwards, to a target defined as half of the previously measured maximal flexion and abduction ROM, with the eyes open. An inclinometer attached to the upper arm, just below the insertion of the deltoid muscle allowed the examiner to check whether this target position was correctly reached and provided feedback to the patients. Next, patients tried to actively reposition their arm in the target position of shoulder flexion and abduction with their eyes closed. The difference in degrees between the achieved positions and the target positions of shoulder flexion and abduction ROM were taken as the active joint position error and used for analysis (Fig. 2B).
StatisticsMeans and standard deviations (SD) are presented for continuous variables and number and percentage are presented for categorical variables for patient characteristics and clinical measurements.
For the primary aim, determination of the clinical course, negative binomial regression (for disabilities, pain intensity, and muscle strength) and linear mixed models (for ROM, scapular upward rotation, and joint proprioception) were fitted using restricted maximum likelihood to account for repeated measurements over time (at baseline and at 3- and 6-months follow-up), missing values, and dropouts. To account for the dependence between measurements from the same individual, an individual identifier was entered as random effect. Treatment received during the 9-month follow-up period was added as a covariate. Disabilities (DASH), pain intensity (VAS), active and passive ROM (all directions and angles), muscle strength (all four measurements), scapular upward rotation at different abduction angles, and proprioception (two movement planes) at 9-month follow-up were entered as dependent variables. Tukey post-hoc analysis was performed when appropriate. All linear mixed models (LMM) were checked for normality, linearity, and heteroskedasticity with a QQ-plot and fitted-residuals plot, respectively. In case of negative binomial regression, geometric means were calculated.
For the secondary aim, the direct longitudinal correlations between different variables, correlations were analyzed with multiple regression within subjects, to remove differences between subjects.27 Strength of the correlation was determined as follows28: very strong (r>0.8), moderately strong (0.6<r<0.8), fair (0.3<r<0.6), and poor (r<0.3).
Statistical analysis was performed in R (version 4.1.2, Vienna Austria). Linear mixed models were fitted using add-on packages lme4,29 pbkrtest,30 and emmeans.31 Longitudinal correlation was determined using add-on package rmcorr.32
ResultsPatient characteristicsInitially, 149 patients with FS were included and 88 (59%) completed all follow-up measurements. The number of patients, their characteristics, and outcomes at the different follow-up measurements are presented in Tables 1 and 2.
Patient characteristics at the different follow-up time points. Values presented as mean (standard deviation) or frequency (percentage). Baseline is moment of inclusion.
NA, not applicable; BMI, body mass index; CSI, corticosteroid injection.
Mean difference indicates the difference between all patients included at baseline (n = 149) and all patients who completed all follow-up measurements (n = 88).
Result of outcome measurements at the different follow-up time points. Values presented as mean (standard deviation) or frequency (percentage). Baseline is moment of inclusion.
DASH, disabilities of the arm, shoulder, and hand; VAS, visual analogue scale; ROM, range of motion.
DASH/VAS, high scores indicate more disabilities/pain.
Mean difference indicates the difference between all patients included at baseline (n = 149) and all patients who completed all follow-up measurements (n = 88).
Table 3 shows the results of the time analyses for all the measurements at each follow-up time.
Analysis for the disability, pain intensity, range of motion measurements, muscle strength, scapular kinematics, and proprioception over time.
Linear mixed model shows an improvement from baseline (moment of inclusion) to all other follow-up measurements for shoulder disabilities (DASH), pain intensity (VAS), active (0° and 90° abduction) and passive ER (0° abduction), active and passive flexion and abduction, muscle strength (abduction, ER, and lift-off), and scapular upward rotation (30° and 60° abduction). An improvement from baseline to 6- and 9-months follow-up was found for passive ER (90° abduction), active and passive IR, and scapular upward rotation at 90° abduction, while for IR muscle strength an improvement was found from baseline to 9-months follow-up. From baseline to 6-months follow-up, an improvement for abduction joint repositioning was found.
From 3-months follow-up to 6- and 9-months follow-up an improvement was found for shoulder disabilities (DASH), pain intensity (VAS), active and passive ER (both abduction positions), active and passive IR, active abduction, passive flexion and abduction, and scapular upward rotation (at 30° abduction). Furthermore, improvements were found from 3-months follow-up to 9-months follow-up for active flexion and scapular upward rotation (60° and 90° abduction).
Finally, there was an improvement from 6- to 9-months follow-up for active and passive ER (90° abduction) and active and passive IR (90° abduction).
Direct longitudinal correlationsTable 4 shows the longitudinal correlation coefficients and their 95% confidence intervals for all correlations analyzed. Shoulder disabilities were moderate negatively correlated with pain intensity and active ER (0° abduction). Fair negative correlations were found between shoulder disabilities and active flexion and abduction ROM and abduction muscle strength, while scapular upward rotation (30°, 60°, and 150° abduction) was positively correlated with shoulder disabilities. Pain intensity was negatively correlated with active ROM (all directions) and abduction muscle strength. Active ER and flexion ROM were fair negatively correlated with scapular upward rotation (30° and 60° abduction), this was also found for active abduction ROM and scapular upward rotation (60° and 90° abduction). Fairly positive correlations were found between active flexion ROM and muscle strength (all directions), between active abduction ROM and muscle strength (abduction and lift-off), and between muscle strength (abduction, ER, and IR) and scapular upward rotation (150° abduction). Poor negative correlations were found between shoulder disabilities and muscle strength (all directions except abduction) and between pain intensity and muscle strength (all directions except abduction). Active ER and flexion ROM had poor negative correlations with scapular upward rotation (90° abduction), as did active abduction ROM and scapular upward rotation (30° abduction). Additionally, poor negative correlations were observed between abduction muscle strength and scapular upward rotation (60° abduction), between ER muscle strength and scapular upward rotation (0°, 30°, and 60° abduction), and between lift-off muscle strength and joint repositioning (both directions). Poor positive correlations were found between shoulder disabilities and scapular upward rotation (90° abduction), between pain intensity and scapular upward rotation (30° and 60° abduction), between active ER ROM and muscle strength (all directions, except lift-off), and between active abduction ROM and ER and IR muscle strength. Abduction and IR muscle strength had poor positive correlations with scapular upward rotation (120° abduction).
Longitudinal correlation analysis between the different variables.
DASH, disabilities of the arm, shoulder, and hand; ROM, range of motion; ER, external rotation; IR, internal rotation.
Our primary aim was to determine the clinical course of FS regarding shoulder disabilities, pain intensity, ROM, muscle strength, scapular upward rotation, and proprioception. In general, our results show a decrease in shoulder disability, pain intensity, and scapular upward rotation at 30°, 60°, and 90°, mainly in the early stages of the disease. Moreover, we observed a general increase in active and passive ROM and muscle strength, again primarily in the early stages of the disease. Overall, no significant change in joint repositioning and scapular upward rotation at 0°, 120°, and 150° abduction was found.
The secondary aim was to determine longitudinal correlations between these outcomes. In general, our results indicate correlations between shoulder disability and active ROM (fair to moderate), muscle strength, and scapular upward rotation (poor to fair). Furthermore, correlations were found between active ROM and both scapular upward rotation and muscle strength (both poor to fair) as well as between muscle strength and both scapular upward rotation and joint repositioning (both poor to fair).
Clinical courseWong et al.,7 in their systematic review, summarized the clinical course of FS and found faster early improvement and slower late improvement in ROM and functionality. This result is similar to our findings, including pain intensity. This result might be related to patients transitioning across the different stages of FS, from inflammation to fibrosis.33-35 The initial phases of FS have shown an overexpression of inflammatory mediators (e.g., cytokines),33,35 which are considered to play a central role in high patient-reported pain during the early stages of the disorder. As the condition progresses over time, inflammation gives way to other cellular processes responsible for the stiffening and thickening of the capsule, which are characteristic of the later stages of FS and associated with less pain.33,36,37 This thickening may contribute to the slowing in observed improvements, as Lee et al.38 found a negative correlation between shoulder ROM and capsular stiffness. Improvements in the later phases may be restricted by a ceiling effect, and early significant improvements may limit further progress. These small functional limitations may persist and can even last for multiple years; however, patients appear to adapt to their physical condition despite incomplete and/or delayed recovery.39 Additionally, previous findings have shown that nearly 40% of satisfied patients had abnormal shoulder function.40
There is a lack of studies reporting results on the clinical course of muscle strength, scapular upward rotation, and proprioception in patients with FS. We hypothesize that the improvement in muscle strength can be explained by the improvement in function. If patients are better able to perform daily tasks and work-related activities more frequently, there will be an increase in muscle strength (and load ability) due to the increased load placed on the muscles.
The decreased scapular upward rotation is likely a consequence of improved ROM. It was hypothesized that increased scapular upward rotation is a result of restricted ROM, and patients compensate for this restriction by increasing scapular upward rotation.11 With improved ROM, scapular upward rotation is likely normalized, and therefore, focusing on scapular upward rotation during the rehabilitation of patients with FS may not be the most important target. The increase in ROM and decrease in scapular upward rotation are supported by the longitudinal correlation for scapular upward rotation at 30°, 60°, and 90° abduction. However, above shoulder level, there is no longer a longitudinal correlation for ROM and scapular upward rotation.
Overall, no change in proprioception were observed, indicating that it may not impact the clinical course of FS. The sole change observed for abduction at 6-month follow-up could be due to measurement error or statistical uncertainties. Capsule mechanoreceptors, known to influence proprioception,41 appear unaffected during the inflammatory and fibrotic process and the pain experienced by patients with FS.
Longitudinal correlation of functional outcomesA repeated measures correlation was used to determine correlations between different variables within each patient. Hereby, differences between patients were removed.27 This means that an improvement in, for example, ER ROM will also result in an improvement of shoulder disabilities (correlation r = −0.62), i.e., as ER ROM increases, shoulder disabilities will decrease, meaning that function will improve. Only Griggs et al.40 examined the association between ROM and disabilities (or functional score) without intervention and did not find any association. No association was found between improvement or final ROM and final function score (Simple Shoulder Test or DASH). However, the possible association between improvement in function and ROM was not considered in their analysis. Furthermore, Van Meeteren et al.10 examined the association between ROM and isokinetic muscle strength on the one hand and disabilities on the other hand after multiple corticosteroid injections. They did not find associations between these variables.
The negative correlations between disabilities and both active ROM and muscle strength suggest that an improvement in ROM and muscle strength will result in fewer disabilities. Although we did not intervene on one variable and cannot determine how these factors influence each other, it makes more sense that an improvement in body functions will lead to an improvement in activities as inventoried by the DASH. Active ROM is more strongly correlated with disabilities than muscle strength and therefore appears to be an important variable in treatment. The positive correlation between disabilities and scapular upward rotation below shoulder level suggests that less upward rotation results in fewer disabilities, and patients are better capable of optimizing shoulder function with less upward rotation. In contrast, less disability is experienced with more upward rotation when the arm is moved beyond shoulder level. Apparently, more upward rotation is necessary beyond shoulder level to optimize shoulder function.
The positive correlations between active ROM and muscle strength emphasize the importance of a mutual relationship and suggest that treatment should focus on one of these variables to improve the other as well. In this relationship, flexion and abduction ROM appear to be more important than ER ROM. An explanation for this correlation might be the fact that reaching a certain active ROM requires a minimum level of strength. This also applies to the correlation of muscle strength with disabilities42 and there might no longer be a correlation with increasing muscle strength. As strength increases, it becomes easier for the patient to move the arm to a certain level. Increased scapular upward rotation with restricted ROM can be seen as a compensatory strategy to optimize shoulder function11 and can explain the correlation between active ROM and scapular upward rotation below shoulder level. To compensate for restricted ROM, patients will increase their scapular upward rotation, enabling them to achieve more ROM despite glenohumeral restrictions.
We do not have an explanation for the variable correlations found between muscle strength and scapular upward rotation, as well as the remarkable correlation found between lift-off muscle strength and proprioception.
Clinical implicationsThe results indicate stronger recovery in the early phases but then slows down in the later phases, potentially leading to incomplete recovery as stated by some authors.43
The longitudinal correlation analyses indicated mainly poor to moderate correlations, suggesting that there are also other variables that need to be considered during assessment and treatment besides the physical variables. Psychological variables, such as depression and anxiety, should be considered alongside physical assessment because they have been found to be associated with pain and function, even more than ROM restriction.8,44
Strengths of the studyThe multicenter design with different geographic locations provides multiple benefits over a single center design, such as a large sample size, decreased personal bias, and larger generalizability of the results. Therefore, we consider this as the major strength of our study. The longitudinal design is another strength of the current study. By assessing outcomes at multiple time points, we obtain an overview of the development of the clinical course of FS. The assessment protocol, which is easy to apply and convenient for use in clinical practice, is the third strength of the current study. Lastly, the standardized stage of the FS condition with strict eligibility criteria minimizes the influence of disease duration, despite the lack of a gold standard for diagnosing FS.
LimitationsDuring the conduct of our study, several limitations need to be acknowledged. One of them is the low adherence rate to the research protocol. Only 59% of the sample completed all measurements, although this still included 88 patients. None of the characteristics showed a significant difference between the total sample and the sample that completed all follow-up measurements, making it unlikely that the presented results have been biased due to attrition. A long data-collection period was necessary due to a slow recruitment rate. Furthermore, the lack of a gold standard for diagnosing FS may have led to the inclusion of patients with potential other disorders, such as osteoarthritis. However, the diagnosis of FS was based on generally accepted diagnostic criteria, and we expect this to have only a minor influence. Finally, it is challenging to determine the disease duration because establishing the exact start of the FS is not easy. FS may be preceded by subacromial shoulder pain and transition to a secondary FS condition.
ConclusionWe observed early improvements in disabilities, pain, ROM (ER at 0° abduction, flexion, and abduction), muscle strength, and scapular upward rotation (below shoulder level). However, the improvement in ROM with ER and IR at shoulder level was delayed. There were no changes in proprioception and scapular upward rotation beyond shoulder level. Longitudinal correlations, both positive and negative were identified, indicating relationships between disabilities, ROM, muscle strength, and scapular upward rotation. However, the nature of these correlations remains unclear and requires further investigation in future studies to identify potential treatment targets.
We thank all participants to volunteer in our longitudinal study.