To evaluate the effectiveness of exercise, ergonomic modification, and a combination of training exercise and ergonomic modification on the scores of pain in office workers with neck, shoulders, and lower back pain.
MethodsParticipants (N=142) in this randomized controlled trial were office workers aged 20–50 years old with neck, shoulders, and lower back pain. They were randomly assigned to either the ergonomic modification group, the exercise group, the combined exercise and ergonomic modification group, or the control group (no-treatment). The exercise training group performed a series of stretching exercises, while the ergonomic group received some modification in the working place. Outcome measures were assessed by the Cornell Musculoskeletal Disorders Questionnaire at baseline, after 2, 4, and 6 months of intervention.
ResultsThere was significant differences in pain scores for neck (MD −10.55; 95%CI −14.36 to −6.74), right shoulder (MD −12.17; 95%CI −16.87 to −7.47), left shoulder (MD −11.1; 95%CI −15.1 to −7.09) and lower back (MD −7.8; 95%CI −11.08 to −4.53) between the exercise and control groups. Also, significant differences were seen in pain scores for neck (MD −9.99; 95%CI −13.63 to −6.36), right shoulder (MD −11.12; 95%CI −15.59 to −6.65), left shoulder (MD −10.67; 95%CI −14.49 to −6.85) and lower back (MD −6.87; 95%CI −10 to −3.74) between the combined exercise and ergonomic modification and control groups. The significant improvement from month 4 to 6, was only seen in exercise group (p<0.05).
ConclusionTo have a long term effective on MSDs, physical therapists and occupational therapists should use stretching exercises in their treatment programs rather than solely rely on ergonomic modification.
Clinical trial IDNCT02874950 – https://www.clinicaltrials.gov/ct2/show/NCT02874950.
Musculoskeletal disorders (MSDs) are often associated with ergonomic risk factors,1 and there is an association between the socioeconomic positions of workers and musculoskeletal pain at various anatomical sites of pain.2 Evidence suggests ergonomic risk features including contact stress, awkward posture (positions of the body that deviate significantly from the neutral position while performing work activities), and repetition are the main cause of many ergonomic associated MSDs.3 Studies have demonstrated these ergonomic MSDs can lead to absenteeism and even disability,4 and also can lead to medical leave due to physical injuries/pain, and this can potentially have a negative influence on the financial productivity and efficiency of the employer.5 MSDs affect both the individuals’ quality life and also have negatively impact on the productivity of the organization they are working with.
The musculoskeletal problems are especially predominant in industrialized countries since they affect approximately 70–80% of adults at some point in their lives.6,7 Most MSDs affect areas such as the neck, shoulders, and low back. The World Health Organization (WHO) has reported physique and working environment of a person, along with other sociological and psychosocial risks, can help work-related MSDs.8 This recommends a relationship between MSDs and working situations among workers of office.
The interventions and treatments suggested by earlier studies9,10 are oftentimes too general and expensive, with many recommendations require the specialists’ consultation. A gap has also been identified in the literature since most studies11,12 only examine the short-term outcomes, such as a recent study which concluded that regular stretching exercises performed for four weeks can decrease neck and shoulder pain. However, it was not clear if the suggested exercise would result in long-term improvements.13 Therefore, the long-term effects of such treatments are often unknown. Some interventions have been used to treat ergonomic MSDs which includes, ergonomic modification, rest breaks, and workplace exercise.14 Though some of these interventions have been found to effectively reduce the symptoms of MSDs, the most effective intervention is the ergonomic modification, which can be effectively used for relief neck, shoulders, and lower back discomforts. To date, there is very limited information regarding the effects of a specific series of office training exercise on decreasing or preventing of MSDs in office workers, especially those with long time treatment. A recent review, concluded that there was moderate evidence of no benefit for job stress management training or office workstation adjustment for MSD and symptoms, and it demonstrated that there is a need for using exercise training in the office setting,15 but there is not a specific package of office/home-based exercise for this purpose specially with focus on neck, shoulder and lower back.
The novelty of this research is related to the link made between sport science and occupational health and introduce a treatment, which has minimal side effects compared to other interventions and can improve companies’ financial efficiency and productivity by decreasing MSDs-induced staff absence. Therefore, the purpose of this study was to evaluate the effects of a 6-month office training exercise, ergonomic modification, and a combination of the training exercise and ergonomic modification on the neck, shoulders, and lower back discomfort perception scores among office workers. It was hypothesized that 6 months intervention is able to reduce pain intensity among office workers.
MethodsStudy typeA prospectively registered, three-arm, parallel, randomized, controlled trial. This trial followed the CONSORT recommendations as well as the TIdieR checklist for describing the interventions.16
ParticipantsThe participants in this study (male=85, female=95) were office workers aged 20–50 years, working in Kuala Lumpur, Malaysia. Participants had to report an MSDs in at least one area of his/her body with medium/high severity of pain. Also, they had to participate in annual medical checkups performed by the company and their results were available. They voluntarily participated in this research (Table 1) from three various regions including the north, west, and east of the Selangor area, Malaysia (the manager of the south section did not agree to participate in this study). All participants had at least two years of experience working in offices and worked a typical shift (from 8:00a.m. to 5:00p.m.) with one hour of rest period from 1:00 to 2:00p.m. However, they worked and sat on a chair during their entire work shift (i.e., for eight hours).
Demographic and baseline characteristics of participants in each group (N=142) (male=47, female=95).
| Exercise training (n=43) | Ergonomic modification (n=37) | Combined exercise & modification (n=34) | Control (n=28) | |
|---|---|---|---|---|
| Age (years) | 29.41±1.16 | 28.31±0.92 | 29.64±0.90 | 28.74±0.82 |
| Height (cm) | 163.29±1.46 | 159.51±1.92 | 166.16±1.34 | 161.25±1.57 |
| Body mass (kg) | 73.26±3.75 | 71.02±3.22 | 74.07±3.60 | 72.61±2.60 |
| Working duration (hr) | 8.15±0.06 | 8.20±0.06 | 8.18±0.05 | 8.06±0.04 |
| Pain score in neck | 13.46±2.57 | 13.24±2.20 | 14.93±2.77 | 15.65±2.80 |
| Pain score in right shoulder | 15.34±2.45 | 16.76±2.80 | 17.33±2.64 | 18.24±3.42 |
| Pain score in left shoulder | 13.41±2.08 | 13.13±1.93 | 11.79±1.73 | 15.21±2.80 |
| Pain score in lower back | 11.91±2.12 | 13.13±2.01 | 14.00±2.06 | 8.76±1.76 |
Values are means±standard deviation.
Note: cm, centimeters; kg, kilograms; hr, hour.
This study was conducted from August 2015 to April 2016 in Malaysia. Prior to participation in the study, medical history was completed by all participants. An informed consent form was signed by the participants who were in line with the Helsinki Declaration's ethical guidelines referring to the use of human participants in medical studies. This research was confirmed by the Institutional Review Board of University Putra Malaysia (UPM), Malaysia (FPSK-EXP16-P046). The ClinicalTrial ID for this study is NCT02874950.
Patients were excluded who had carried out other physical activities throughout last 3 months, who had any psychiatric, pathological or neurological disorders and who had not been certified as being medically fit in their most recent annual checkup. Individuals with cardiovascular diseases medical history (e.g. heart failure, chest pain during physical exercise, stroke and myocardial infarction). Individuals with a severe or traumatic injury to the hand, back, shoulder, arm or neck regions for the past year. Individuals with a life-threatening disease. People with any new surgery (<3 months).
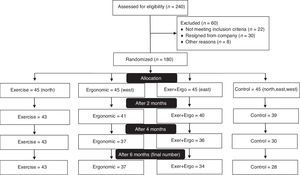
Randomization and allocationThe permuted block randomization method was used to randomly assign the participants to either the exercise training group (n=45, north area), ergonomic modification group (n=45, west area), both exercise training and ergonomic modification group (n=45, east area), or a control group (no-treatment) (n=45, north, east and west areas). The same intervention program was assigned to participants in each location in order to avoid group contamination. The control group (no-treatment) was chosen from all three locations (north=15, east=15, and west=15). The allocation was concealed by using opaque, sealed envelopes that were consecutively numbered and included each group's name. The four groups involved in the following activities: (a) the exercise training group, (b) the ergonomic modification group, (c) the exercise training and ergonomic modification group did both of those interventions mentioned in (a) and (b), and (d) the control group (no-treatment).
InterventionsThe first intervention was an exercise routine contained certain validated and standardized office-based stretching exercises mechanisms to rise the range and flexibility of motion in the muscles of the back (i.e. multifidus) as well as shoulders and neck joints,17 easy to learn and perform,17 with a particular order intended for office employers in response to shoulders, lower back, and neck pains. The exercise protocol contained thirteen exercises adopted from McKenzie's exercises,18 William's exercises,19 and guidelines of American College of Sports Medicine (ACSM).17 The stretching was to be performed constant, controlled, and slow, and tension is slowly applied to a muscle or group of muscle to the end of the joint's range of movement (ROM) until the mild discomfort point is touched.
To make sure the exercises were performed properly and correctly, an experienced Certified Specialist of Conditioning and Strength Training (CSCS) trained all participants who then monitored the participants’ techniques. The trainer was not aware which location was related to exercise group and which location was related to the combination of exercise and ergonomic modification group. This period of familiarization was vital for office workers since most of them did not have previous experience of performing such exercises. Each familiarization session involved one or two sets of 8–10 repetitions of the exercises. Each participant would receive an exercise training video with instructions. The set of exercises was designed to be performed once a day/3 times a week, with each session last approximately 10–15min. Each individual exercise includes 10 repetitions (or last for a period of 10–15s) and 3 sets (with a rest of 60–90s between sets) on alternate days under the supervision of the Certified Specialist.13 A pilot study was done for this package of exercise.20
The ergonomic modification group (second intervention) involved a “total workplace Occupational Safety and Health and ergonomic intervention” that contained the modification of the chair height and working desk, the sitting posture, the distance and level between the eyes and the monitor based on recommendations from the online rapid office strain assessment (ROSA).21 The ergonomic modification was performed with an Occupational Health expert, who was not aware which location was related to the ergonomic group and which location was related to the combination of exercise and ergonomic modification group. The third intervention involved both modifying ergonomics and exercises.
It was elaborated to the participants in the control group (no-treatment) that through the six months of the study period, they should continue their usual work day as they had previously. The control group (no-treatment) was also informed they could receive one of the interventions after the study was complete.
OutcomesThe primary outcome of this study was MSDs scores (the dependent variable) in response to three interventions (the independent variables) among office workers. After randomization, neck, shoulders, and lower back discomfort scores were assessed by the Cornell Musculoskeletal Disorders Questionnaire (CMDQ)6 at baseline and after 2, 4, and 6 months of the intervention. The changes in mean scores after the intervention were compared to each group and among four different groups. The validity and reliability of Cornell Questionnaire was measured in a pilot study in Malaysia among office workers and examination of psychometric properties of CMDQ yielded satisfactory results.6 The Cornell Questionnaire's results were scored according to the method developed by Erdinc et al.22
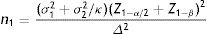
Sample sizeWith following formula, the sample size of this trial was calculated.23 The researcher considered each objective independently, and then the largest sample size was selected. The required sample size included 30 staff and, to manage predicted drop-outs, 60 respondents were selected for each of the four groups.
wheren1 is sample size of Group 1=30
n2 is sample size of Group 2=30
σ1 is standard deviation of Group 1=20.2
σ2 is standard deviation of Group 2=21.1
Δ is difference in group means=−15
κ is ratio n2/n1=1
Z1−α/2=two-sided Z value (e.g. Z=1.96 for 95% confidence interval).
Z1−β=power=80%
(Group 1=Control, Group 2=Intervention group)
Statistical analyses were conducted by IBM SPSS (Statistical Package for Social Sciences (SPSS), Version 22, Chicago, IL). Prior to data analysis, the normality test was performed for all variables. Descriptive statistics of the variables was presented in means and standard deviations (±SDs). The variables were analyzed at four points throughout the process (baseline, 2, 4, and 6 months after the intervention). Factorial two-way repeated measures analysis of covariance (RM-ANCOVA) was used for data analysis. The hypothesis of interest was the interaction between time (baseline, 2-month, 4-month, 6-month) and group. Because of a significant relationship between BMI at pre-test and all variables, this variable was used as a covariate in the analysis. For within-group comparisons, Bonferroni post hoc test was employed. We also performed an intention to treat analysis (ITTA) using an imputation method, “last observation carried forward” (LOCF) in order to deal with any missing data at follow up.24 A priori α significant level was set at p<0.05.
ResultsOf the 240 patients initially considered eligible to perform one of the interventions or just be as a control with MSDs with medium/high severity of pain, 180 were randomized and 142 completed the study, as presented in the CONSORT flowchart (Fig. 1). At 6-month follow-up 18 participants had resigned from the company, five participants did not receive the intervention, and 15 participants in control group decided to drop out from the study and do the treatments at home by themselves.
Table 1 shows baseline data is similar for the variables including age, height, body mass and working duration.
Descriptive statistics of the discomfort scores among the four groups is presented in Table 2.
Scores of pain, based on Cornell questionnaire in baseline and follow-up (N=142).
| Exercise training (n=43) | Ergonomic modification (n=37) | Combined exercise & modification (n=34) | Control (n=28) | |
|---|---|---|---|---|
| Neck | ||||
| Baseline | 13.46 | 13.24 | 14.93 | 15.65 |
| 2 months | 4.01 | 4.79 | 4.70 | 15.47 |
| 4 months | 2.22 | 2.23 | 2.45 | 14.77 |
| 6 months | 1.88 | 2.10 | 2.62 | 12.55 |
| Right shoulder | ||||
| Baseline | 15.34 | 16.76 | 17.33 | 18.24 |
| 2 months | 4.84 | 4.31 | 4.96 | 13.74 |
| 4 months | 2.44 | 2.27 | 17.33 | 11.26 |
| 6 months | 1.41 | 2.10 | 2.23 | 13.05 |
| Left shoulder | ||||
| Baseline | 13.41 | 13.13 | 11.79 | 15.21 |
| 2 months | 3.99 | 3.77 | 3.82 | 12.27 |
| 4 months | 1.82 | 2.04 | 2.15 | 13.19 |
| 6 months | 1.65 | 1.89 | 2.07 | 12.74 |
| Lower back | ||||
| Baseline | 11.91 | 13.13 | 14.00 | 8.76 |
| 2 months | 4.28 | 4.23 | 4.96 | 8.65 |
| 4 months | 2.01 | 2.87 | 2.79 | 9.03 |
| 6 months | 1.29 | 2.69 | 2.07 | 8.63 |
Note: Higher numbers show the sever level of pain.
The results of the RM-ANCOVA indicating the intervention had a significant (p<0.05) effect on the neck, shoulders and lower back, discomfort scores. Pairwise comparisons across time for all control (no-treatment) and intervention groups are shown in Table 3.
Pairwise comparisons across time for all control and intervention groups (within group comparison).
| Intervention | (I) time | (J) time | Neck Mean difference (95% CI) | Right shoulder Mean difference (95% CI) | Left shoulder Mean difference (95% CI) | Lower back Mean difference (95% CI) |
|---|---|---|---|---|---|---|
| Exercise | Baseline | 2 months | 9.16(4.86 to 13.46)** | 10.23(4.55 to 15.92)** | 9.42(5.13 to 13.72)** | 7.55(4.08 to 11.02)** |
| Baseline | 4 months | 10.99(5.75 to 16.23)** | 12.46(5.32 to 19.61)** | 11.58(6.62 to 16.56)** | 9.73(5.32 to 14.15)** | |
| Baseline | 6 months | 11.29(5.85 to 16.72)** | 13.6(6.64 to 20.58)** | 11.76(6.78 to 16.75)** | 10.45(5.87 to 15.04)** | |
| 2 months | 4 months | 1.83(−0.12 to 3.77) | 2.23(−0.39 to 4.85) | 2.16(0.66 to 3.66)** | 2.18(0.82 to 3.54)** | |
| 2 months | 6months | 2.13(0.11 to 4.14)** | 3.37(0.95 to 5.8)** | 2.33(0.78 to 3.9)** | 2.9(1.3 to 4.5)** | |
| 4 months | 6 months | 0.3(−0.86 to 1.46)* | 1.14(−0.52 to 2.81)* | 0.18(−0.94 to 1.29)* | 0.72(0.08 to 1.36)* | |
| Ergonomic | Baseline | 2 months | 8.5(4.28 to 12.73)** | 12.49(6.9 to 18.08)** | 9.35(5.12 to 13.59)** | 8.9(5.5 to 12.32)** |
| Baseline | 4 months | 11.06(5.9 to 16.21)** | 14.56(7.55 to 21.59)** | 11.08(6.18 to 15.99)** | 10.27(5.94 to 14.62)** | |
| Baseline | 6 months | 11.19(5.85 to 16.53)** | 14.71(7.87 to 21.57)** | 11.24(6.33 to 16.16)** | 10.46(5.96 to 14.97)** | |
| 2 months | 4 months | 2.55(0.64 to 4.46)** | 2.07(−0.5 to 4.65) | 1.72(0.25 to 3.21)** | 1.36(0.03 to 2.71)* | |
| 2 months | 6months | 2.69(0.71 to 4.67)** | 2.22(−0.16 to 4.61) | 1.88(0.35 to 3.43)** | 1.55(−0.02 to 3.12) | |
| 4 months | 6 months | 0.14(−1 to 1.28) | 0.15(−1.49 to 1.79) | 0.16(−0.94 to 1.26) | 0.19(−0.45 to 0.82) | |
| Exer+Ergo | Baseline | 2 months | 8.29(4.39 to 12.2)** | 12.25(7.15 to 17.36)** | 7.96(4.1 to 11.83)** | 9.01(5.87 to 12.17)** |
| Baseline | 4 months | 10.55(5.79 to 15.32)** | 14.63(8.22 to 21.05)** | 9.63(5.16 to 14.11)** | 11.16(7.16 to 15.18)** | |
| Baseline | 6 months | 10.62(5.69 to 15.56)** | 14.86(8.61 to 21.12)** | 9.71(5.23 to 14.2)** | 11.88(7.72 to 16.05)** | |
| 2 months | 4 months | 2.26(0.49 to 4.02)** | 2.38(0.03 to 4.74) | 1.66(0.32 to 3.02)** | 2.15(0.91 to 3.39)** | |
| 2 months | 6months | 2.33(0.5 to 4.16)** | 2.6(0.43 to 4.78) ** | 1.75(0.35 to 3.16)** | 2.86(1.42 to 4.32)** | |
| 4 months | 6 months | 0.07(−0.98 to 1.12) | 0.23(−1.27 to 1.72) | 0.08(−0.92 to 1.09) | 0.71(0.14 to 1.3) | |
| Control | Baseline | 2 months | 0.57(−3.94 to 5.09) | 4.89(−1.08 to 10.86) | 2.94(−1.57 to 7.44) | 0.22(−3.42 to 3.86) |
| Baseline | 4 months | 1.22(−4.29 to 6.73) | 7.61(0.12 to 15.12)* | 2.02(−3.19 to 7.22) | −0.06(−4.7 to 4.57) | |
| Baseline | 6 months | 3.91(−1.8 to 9.61)* | 5.66(−1.66 to 12.98) | 2.47(−2.76 to 7.69) | 0.34(−4.47 to 5.15) | |
| 2 months | 4 months | 0.65(−1.39 to 2.69) | 2.73(−0.02 to 5.48) | −0.92(−2.49 to 0.65) | −0.28(−1.71 to 1.15) | |
| 2 months | 6 months | 3.33(1.22 to 5.45)** | 0.77(−1.77 to 3.32) | −0.47(−2.1 to 1.17) | 0.13(−1.55 to 1.8) | |
| 4 months | 6 months | 2.69(1.47 to 3.9)** | −1.95(−3.7 to −0.21)** | 0.45(−0.72 to 1.62) | 0.4(−0.27 to 1.08) | |
After 6 months, there were significant differences in pain scores for neck (MD −10.55; 95%CI −14.36 to −6.74), right shoulder (MD −12.17; 95%CI −16.87 to −7.47), left shoulder (MD −11.1; 95%CI −15.1 to −7.09) and lower back (MD −7.8; 95%CI −11.08 to −4.53) between the exercise and control groups. Also, significant differences were seen in pain scores for neck (MD −9.99; 95%CI −13.63 to −6.36), right shoulder (MD −11.12; 95%CI −15.59 to −6.65), left shoulder (MD −10.67; 95%CI −14.49 to −6.85) and lower back (MD −6.87; 95%CI −10 to −3.74) between the combined exercise and ergonomic modification and control groups (Table 4).
Between-group differences and 95% CI for the effects of interventions.
| Time | (I) Intervention | (J) Intervention | Neck Mean difference (95% CI) | Right shoulder Mean difference (95% CI) | Left shoulder Mean difference (95% CI) | Lower back Mean difference (95% CI) |
|---|---|---|---|---|---|---|
| Baseline | Exercise | Ergonomic | −0.26(−9.36 to 8.84) | −2.06(−13.7 to 9.58) | 0.28(−7.84 to 8.4) | −1.63(−9.33 to 6.08) |
| Exercise | Exer+Ergo | 0.11(−8.65 to 8.87) | −2.3(−13.44 to 8.83) | 1.63(−6.15 to 9.4) | −2.36(−9.78 to 5.05) | |
| Exercise | Control | −3.17(−12.61 to 6.27) | −4.22(−16.3 to 7.85) | −1.8(−10.17 to 6.58) | 2.31(−5.68 to 10.3) | |
| Ergonomic | Exer+Ergo | 0.37(−8.32 to 9.06) | −0.25(−11.29 to 10.8) | 1.34(−6.37 to 9.06) | −0.74(−8.09 to 6.61) | |
| Ergonomic | Control | −2.91(−12.23 to 6.42) | −2.17(−14.09 to 9.76) | −2.08(−10.4 to 6.23) | 3.93(−3.96 to −11.82) | |
| Exer+Ergo | Control | −3.28(−12.3 to 5.74) | −1.92(−13.4 to 9.56) | −3.42(−11.41 to 4.56) | 4.67(−2.96 to 12.3) | |
| After 2 months | Exercise | Ergonomic | −0.92(−6.03 to 4.19) | 0.2(−4.94 to 5.35) | 0.21(−4.15 to −4.58) | −0.27(−4.35 to 3.81) |
| Exercise | Exer+Ergo | −0.76(−5.68 to 4.16) | −0.28(−5.2 to 4.64) | 0.16(−4.02 to 4.34) | −0.9(−4.83 to 3.03) | |
| Exercise | Control | −11.76(−17.06 to −6.45)** | −9.57(−14.91 to −4.23)** | −8.29(−12.79 to −3.79)** | −5.03(−9.26 to −0.8)** | |
| Ergonomic | Exer+Ergo | 0.16(−4.72 to 5.04) | −0.48(−5.37 to 4.4) | −0.05(−4.2 to 4.1) | −0.63(−4.52 to 3.26) | |
| Ergonomic | Control | −10.84(−16.08 to −5.6)** | −9.77(−15.04 to −4.5)** | −8.5(−12.97 to −4.03)** | −4.76(−8.94 to −0.58)* | |
| Exer+Ergo | Control | −11(−16.07 to −5.93)** | −9.29(−14.36 to −4.21)** | −8.45(−12.74 to −4.16)** | −4.13(−8.17 to −0.09)* | |
| After 4 months | Exercise | Ergonomic | −0.2(−4.41 to 4.02) | 0.05(−3.93 to 4.02) | −0.22(−4.25 to 3.82) | −1.08(−4.32 to 2.15) |
| Exercise | Exer+Ergo | −0.33(−4.39 to 3.73) | −0.13(−3.93 to 3.67) | −0.33(−4.2 to 3.53) | −0.93(−4.04 to 2.18) | |
| Exercise | Control | −12.94(−17.32 to −8.56)** | −9.07(−13.19 to −4.95)** | −11.37(−15.53 to 7.21)** | −7.49(−10.84 to −4.13)** | |
| Ergonomic | Exer+Ergo | −0.13(−4.16 to 3.89) | −0.18(−3.95 to 3.6) | −0.11(−3.95 to 3.72) | 0.15(−2.93 to 3.24) | |
| Ergonomic | Control | −12.75(−17.07 to −8.43)** | −9.12(−13.19 to −5.05)** | −11.15(−15.28 to −7.02)** | −6.4(−9.72 to −3.09)** | |
| Exer+Ergo | Control | −12.61(−16.79 to −8.43)** | −8.94(−12.86 to −5.02)** | −11.04(−15.01 to −7.07)** | −6.56(−9.76 to −3.35)** | |
| After 6 months | Exercise | Ergonomic | −0.36(−4.03 to 3.31) | −0.95(−5.48 to 3.59) | −0.24(−4.12 to 3.64) | −1.62(−4.78 to 1.54) |
| Exercise | Exer+Ergo | −0.56(−4.09 to 2.97) | −1.05(−5.38 to 3.29) | −0.42(−4.14 to 3.3) | −0.93(−3.97 to 2.11) | |
| Exercise | Control | −10.55(−14.36 to −6.74)** | −12.17(−16.87 to −7.47)** | −11.1(−15.1 to −7.09)** | −7.8(−11.08 to −4.53)** | |
| Ergonomic | Exer+Ergo | −0.2(−3.7 to 3.3) | −0.1(−4.4 to 4.2) | −0.19(−3.88 to 3.51) | 0.69(−2.33 to 3.7) | |
| Ergonomic | Control | 0.2(−3.3 to 3.7) | 0.1(−4.2 to 4.4) | 0.19(−3.51 to 3.88) | −0.69(−3.7 to 2.33) | |
| Exer+Ergo | Control | −9.99(−13.63 to −6.36)** | −11.12(−15.59 to −6.65)** | −10.67(−14.49 to −6.85)** | −6.87(−10 to −3.74)** | |
The significant improvement from month 4 to 6 for neck (MD −0.3; 95%CI −0.86 to 1.46), right shoulder (MD 1.14; 95%CI −0.52 to 2.81), left shoulder (MD 0.18; 95%CI −0.94 to 1.29) and lower back (MD 0.72; 95%CI 0.08–1.36), were only seen in exercise group (p<0.05).
However, there were no significant differences (p>0.01) among treatment groups after 2 and 4 months of intervention.
DiscussionThis study examined the effects of exercise training, ergonomic modification, and the combination of exercise training and ergonomic modification on reducing shoulders, neck, and lower back discomfort among workers of office. To increase the validity of the measurement (e.g., isolating confounding variables and bias), a series of interventions and a control group (no-treatment) were used. It should be noted that, most of the drop outs in this study were in the control group. We promised participants in the control group that they would receive the same intervention after the study (6 months) however some of them decided to leave the study and do their exercises at home. It is interesting to note that, after 4 months all three interventions had some effect on discomfort of lower back, shoulders, and neck scores. However, after 6 months, only exercise and the combination of exercise and ergonomic modification were effective on pain scores in comparison with the control group, but significant improvement from month 4 to 6, was only seen in the exercise group. Managers should consider implementing at least one intervention to their offices, and the type of intervention can be based on the working environment of their organizations and the convenience of the office workers. The results of the current study are consistent with previous findings.8,25,26 For example, Machado-Matos et al.27 demonstrated that core stability exercises is more effective than the general exercises.27 However, Robertson et al.28 showed that significant improvement in low back pain was based on chair adjustment rather than strength exercise and stretching.28 Nevertheless, by participating in exercise training, office workers can enjoy sound sleep as well as a reduced level of fatigue related to their pains.10
Pain in the neck, lower back and shoulder are normally intensified by static loading of the spine (e.g., prolonged standing or sitting), long lever activities (e.g., working with the arms raised and away from the body or vacuuming), or levered postures (e.g., bending forward).17 Pain can be decreased if the spine can be balanced via multi-directional forces (e.g., physical activity or continuously changing positions or walking) or when they unload the spine (e.g., resting).29
Considering the theory supporting the efficiency of particular exercises, it must be stated that these exercises can reduce the pressure which is forced on the nerves running through the spinal via progresses the range of muscles’ flexibility and motion, especially the hips’ extensors and flexors together with the piriformis muscle, since stretching the muscles in these areas will usually decrease the pain of the multifidus muscles significantly. In this context, the neuromuscular mechanisms’ response can be promoted by stretching, via the proprioceptors stimulation in an attempt to achieve back muscles flexibility.29
The prevalence of MSDs has wide implications on the economy of a country since MSDs affects office workers productivity negatively, and it also leads to a longer period of sick leave.30 This high rate of MSDs in the workplace urges the needs for identifying the most optimal methods of prevention. A considerable amount of study has been devoted to this subject in developing countries, but most of the studies has merely emphasized the occurrence of these problems among office employers. Some researchers have recommended a simple and general training protocol for the whole body or recommended some ways to adjust the ergonomics situations of their working condition.25,31,32
Physical ergonomics deals with the reduction of the physiological and physical stress of the body. Therefore it is essential to consider ergonomics of the workplace as part of the prevention and treatment of MSDs.28 This study postulated that changes made to the desk placement, computer workstation and the keyboard and computer monitor placement could improve neck, shoulder, and lower back postures. Logically, when employers are exposed to the risk factors of MSDs, they start to experience exhaustion. Which said, when fatigue overtakes recovery system of their bodies, they will also suffer from musculoskeletal imbalance. Consequently, when exhaustion continued to put on recovery and said musculoskeletal imbalance continues, this results in musculoskeletal disorders development.33,34 Gradually, habits from daily activities including cradling a cell phone, prolonged standing, to carry a purse on the same shoulder, staring at the computer, and even sitting in office chairs may result in poor posture.21 Following a modified version of the workplace, ergonomics can help to improve body postures by positively affecting overactive muscles including external and internal obliques as along with quadratus lumborum, erector spine and hip abductors.
The findings of this trial demonstrated that there were significant improvements in the discomfort scores as soon as two months after the intervention, but the effectiveness diminished over time. Specifically, there was no significant improvement for the ergonomic modification group after two months of intervention and there was no significant improvement for all the experimental groups after four months. This implies that a basic arrangement of office equipment (e.g., desk placement, seat height, the position of the keyboard, mouse, and monitor) is effective in reducing MSDs, but further improvement requires the long-term commitment of the organizations (e.g., replacing the chair and desk entirely). Perhaps this could be enhanced if the routine of exercises were changed every few months progressing to resistance exercise.
Surprisingly, it was expected these results to be different. It was hypothesized that the combination of interventions would result in superior outcomes, but this was not observed. It is possible that each individual has inherent value but that combining the 2 interventions does not produce a treatment effect that exceeds that of one intervention alone. It is possible that the physiological responses associated with each intervention are the same. Hence, the combination would not and did not provide any additional benefit. Future studies should continue to examine multimodal treatment approaches as this is representative of common clinical practice.
LimitationsThere are a number of limitations to this study that should be considered. The ergonomic modification in our study was limited to adjusting the equipment (e.g., desks, chairs, keyboard, mouse, and monitor) and not replacing the desks and chairs entirely. The workouts introduced in this study are stretching exercises without loading. Therefore, the effect of stretching exercises on MSDs cannot be fully extrapolated. Additionally there was a lack of blinding of those assessing outcomes and there was a fairly moderate dropout rate in the control group (no-treatment).
ConclusionThis study provides preliminary evidence for the use of ergonomic modification and exercise to improve discomfort for office workers with MSDs. Based on the results of this study there was not a significant difference among treatment groups after 4 months intervention, but all the groups showed a significant improvement in comparison with the control group (no-treatment) and comparison with their baseline scores. It should be noted that there was not a significant improvement in the ergonomic modification group and exercise and ergonomic modification group from 4th month to the 6th month. However, this improvement was significant in the exercise group related to shoulders and lower back. This demonstrates that exercise modification was more effective in comparison with ergonomic modification after 4 months. It should be suggested that for the physical therapist and occupation therapist to use the exercise training for long-term treatment rather than only ergonomic modification. It is suggested that future studies should examine different exercise protocols among white-collar and blue-collar workers in various occupations.
FundingThere was no grant or funding for this research and it was done by the personal budget of researchers.
Conflicts of interestThe authors declare no conflicts of interest.
We would like to express our sincere gratitude to Professor David Pyne, Australian Institute of Sport, Canberra, Australia, for his assistance with the manuscript.