Facial palsy (FP) is defined as an injury of the seventh cranial nerve pair, partial or total, which can be classified as central or peripheral. Proprioceptive neuromuscular facilitation (PNF) is primarily used in the functional recovery of upper and lower limb conditions, however the technique has also been used for FP.
ObjectiveTo analyze the effect of PNF in the treatment of dysfunctions in FP.
MethodsTen databases including BVS, CENTRAL Cochrane, CINAHL, PEDro, PubMed, Scielo, ScienceDirect, SCOPUS, Web of Science, and Google Scholar were comprehensively searched for dates prior to April 2021. Randomized controlled trials of PNF in individuals with dysfunctions caused by facial paralysis were eligible. Outcomes measures were recovery rate and clinical recovery, both measured by using the House Brackmann Scale. Recovery time was measured in days and synkinesis assessed with the Synkinesis Assessment Questionnaire.
ResultsA total of 184 patients were included. In general, the included studies have low methodological quality. None of the five studies used PNF as the sole intervention. In all of the included studies PNF was used in combination with other interventions. Our findings show very low evidence that PNF is more effective than minimal intervention for treating FP.
ConclusionWe conclude that given the limited number of studies included and the low methodological quality presented, recommendations based on these studies should be interpreted with caution. The effects of PNF on facial paralysis are not clear.
Facial palsy (FP) is defined as an injury of the seventh cranial nerve pair, partial or total, which can be classified as central FP or peripheral FP, depending on the location on the nervous injury.1 Given that the facial nerve has both sensory and motor functions, sequelae of FP may include sensory and motor dysfunctions. However, motor deficits have greater relevance due to the inability to produce facial expressions, leading to emotional sequelae.1–3
Evidence from systematic reviews and meta-analyses points to the cautious use of steroid and antiviral drugs,4–7 techniques such as electrotherapy,1,8,9 and acupuncture,10–12 as well as massages and facial exercises due to the low quality of existing studies. Proprioceptive neuromuscular facilitation (PNF) techniques are included among facial exercises.8,9,13–15
PNF is a technique commonly used to treat FP. Recently, trials16 investigating the efficacy of PNF for FP have been published. To our knowledge, there are no previous systematic reviews that have summarized the evidence regarding PNF for the treatment of FP. Therefore, the aim of this systematic review was to investigate the effect of PNF exercises as a treatment for FP.
MethodsThis review adhered to the recommendations proposed by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)17 and was previously registered at the International Prospective Register of Systematic Review (PROSPERO) – CRD42017068744.
Identification and selection of trialsWe performed electronic searches in 10 databases: PubMed, CENTRAL Cochrane, Science Direct, SciELO, Web of Science, PEDro, CINAHL, BVS, Scopus, and Google Scholar. In addition, we conducted a hand search on the reference lists of relevant studies. The search was performed in April 2021. No limit of date was used as filters on databases. We did not limit the search to a specific language or publication date. Our search strategy included the following terms, “proprioceptive neuromuscular facilitation”, “proprioceptive neuromuscular facilitation pattern”, “Kabat”, “facial paralysis”, “Bell palsy”, grouped with Boolean operators OR and AND. The search strategy for the majority of the database was “((((proprioceptive neuromuscular facilitation) OR (proprioceptive neuromuscular facilitation pattern)) OR (kabat)) AND (facial paralysis)) OR (Bell palsy)”. The only exception was the search on the PEDro database for which we used the following "(proprioceptive neuromuscular facilitation AND facial paralysis), (proprioceptive neuromuscular facilitation pattern AND facial paralysis), (Kabat AND facial paralysis), (proprioceptive neuromuscular facilitation AND Bell Palsy), (proprioceptive neuromuscular facilitation pattern AND Bell Palsy), (Kabat AND Bell Palsy)”.
Study selection and eligibility criteriaIn this systematic review, we included randomized controlled trials (RCTs) involving PNF exercises in the treatment of FP. We did not limit this review to a specific cause for FP. Systematic reviews, literature reviews, book chapters, conference abstracts, clinical trials that did not use PNF as treatment, preclinical studies, as well as duplicate studies were not considered to be included in the review. The inclusion criteria were RCTs that assessed individuals with dysfunctions caused by FP treated with PNF as a single treatment or in combination with other treatments compared to no treatment, placebo, or any other treatment.
Two reviewers (MCS and MTO) independently selected the trials to be considered in the review by screening the titles, abstracts, and full text, according to preestablished criteria. These reviewers were blinded to the journal and authors in which the studies were published. A third reviewer (IAFS) was consulted to resolve disagreements between reviewers during the selection of studies.
Data extractionData were extracted in a standardized manner. The information extracted included characteristics of the population, type of FP, interventions used in the control and treatment arms based on TIDieR checklist,18 and outcome measures. Primary outcomes evaluated in this review were recovery rate and clinical recovery, recovery time, and synkinesis. With regard to secondary outcomes, facial disability, symmetry, severity of paresis, and nerve conduction velocity were evaluated.
Risk of bias assessmentAssessment of risk of bias was performed using the Cochrane Collaboration tool (RevMan version 5.3™, London, UK).19 Eight domains were evaluated in this review: selection bias (randomization sequence generation, allocation concealment), performance bias (blinding of participants), detection bias (blinding of outcomes assessor), attrition bias (incomplete outcome data), and reporting bias (source of funding). One other bias was added, in view of the need for some information considered important for clinical practice to be reported, such as use of combined therapy (association of PNF with conventional physical therapy or other techniques).
For each study, each item was classified according to three categories: low risk, high risk, and unclear risk of bias (insufficient information for judgment).
Data analysisAlthough pooling of data via meta-analysis was pre-planned, we did not perform meta-analysis because included trials were not sufficiently homogeneous. Trials were grouped according to the intervention and comparator. Trial results for individual studies were extracted and differences between groups were expressed, when possible, as mean difference (MD) and 95% confidence interval (95%CI) or mean ± standard deviation. There was an attempt to synthesize the evidence using the Grading of Recommendation, Assessment, Development and Evaluation (GRADE) approach, however, due to the lack of trials investigating the same type of intervention and comparators, single randomized trials were considered inconsistent and imprecise (that is, sparse data) and provided “very low quality" evidence.
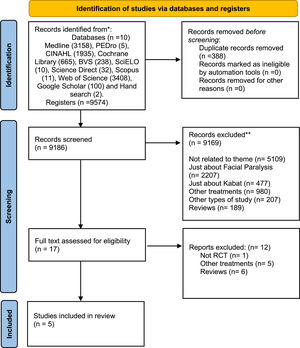
ResultsFlow of studies through the reviewThe database search yielded 9574 including duplicates. A total of 9169 records were excluded during the title and abstract screening. Thus, 16 records advanced for full text analysis. Finally, five trials were included (Fig. 1).20–24
Characteristics of included studiesDetailed information about the 5 included trials are provided in Table 1.
Characteristics of the included studies.
| Authors/Data | Sample | Type | Intervention Protocol | Control | Outcomes | Results |
|---|---|---|---|---|---|---|
| Barbara et al., 201020 | Total (n = 20): PNF + drugs group (n = 9)Men (n = 5) Women (n = 4)Control group (n = 11)Men (n = 5)Women (n = 6) | Peripheral facial paralysis of viral origin | PNF exercises were performed in 3 regions: upper, intermediate, and lower. (Upper region –traction downwards or upwards, always vertical plan. Intermediate region – traction movements opposite to the normal direction, in vertical line. Lower region – horizontal plane and in a vertical plane depending on muscle activation.) | Drugs:Antiviral drugs (Aciclovir 400 mg, 3 times per day) administered for 15 days and a full dosage of steroids (prednisolone 40 mg per day) for 10 days and tapered within the next 5 days. | - Nerve conduction speed (CMAP)- Clinical recovery (HBS) | - CMAP: No significant difference between groups- HBS: Significant difference between PNF + drugs compared to drugs alone (p = 0.028). |
| Ghous et al., 201821 | Total (n = 20):Men (n = 11), Women (n = 9)PNF group (n = 10)Taping group (n = 10) | Peripheral facial paralysis of non-traumatic origin (acute and sub-acute) | PNF exercises with conventional physical therapy treatment* | Facial expression exercises combined with kinesiology tape and conventional physical therapy treatment* | - Synkinesis (SAQ)- Facial disability (FDI)- Severity of paresis (HBS) | - SAQ: Significant difference in PNF group (p = 0.03)- FDI - Physical function: Significant difference in PNF group compared to taping group (p = 0.01)- FDI – social function: No significant difference between groups- HBS: No significant difference between groups |
| Kumar and Bagga, 2015 22 | Total (n = 40):PNF with conventional physical therapy treatment (n = 20)NRM with conventional physical therapy treatment (n = 20) | Peripheral facial paralysis of non-traumatic origin | PNF exercises combined with conventional treatment (electrotherapy – interrupted galvanic stimulation with rectangular waveform with 100 ms, 3 sets and 30 contractions in each set – and manual facial massage) | NRM exercises combined with conventional treatment (electrotherapy – interrupted galvanic stimulation with rectangular waveform with 100 ms, 3 sets and 30 contractions in each set – and manual facial massage)* | - Resting symmetry, symmetry of voluntary movement and synkinesis (SFGS)- Physical disability and psychosocial factors (FDI)- Synkinesis (SAQ) | - SFGS: Significant difference in PNF group compared to NRM group (p = 0.005)- FDI: Significant difference in PNF group compared to NRM group (p < 0.001);- SAQ: Significant difference in NRM compared to PNF group (p = 0.013) |
| Monini et al., 201723 | Total (n = 104):Group A: medical treatmentGroup B: medical treatment combined with PNF.Both groups were subdivided according to the age of the patients (≤65 years and >65 years) totaling 4 groups investigated. | Peripheral facial paralysis | PNF exercises combined with medical treatment (steroids, dosage of 60 mg per day, for 10 consecutive days, and tapered off by 10 mg until suspension) | Medical treatment (steroids, dosage of 60 mg per day, for 10 consecutive days, and tapered off by 10 mg until suspension) | - Rate of recovery (HBS)- Recovery time (Days)- Movement, facial comfort, oral function, eye comfort, tear control and social function (Beta FACE Scale) | - HBS: PNF was more effective compared to drugs alone with degrees of recovery- Days: Significant difference in PNF group compared to drugs alone (p = 0.003)- Beta FACE: No significant difference between groups. |
| Khanzada et al., 2018 | Total (n = 52):PNF plus nerve stimulation (n = 26)Facial exercise plus nerve stimulation (n = 26) | Peripheral facial paralysis | PNF combined with nerve stimulation | Facial exercises combined with nerve stimulation | - Symmetry (SFGS)- Facial disability (FDI) | - SFGS: Significant improvement (p < 0.01) in both groups- FDI: Significant improvement (p < 0.01) in both groups |
CMAP, compound motor action potential; FDI, Facial Disability Index; HBS, House Brackman Scale; NRM, Neuromuscular Re-Education; PNF, proprioceptive neuromuscular facilitation; SAQ, Synkinesis Assessment Questionnaire; SFGS, Sunny Brook Facial Grading Scale.
The five trials included in this review involved 236 participants with non-traumatic peripheral FP.20–24 Participants were from both sexes and were between 16 and 90 years old.
Intervention and comparatorsIn all five included studies PNF was used in combination with other interventions. Barbara et al.20 and Monini et al.23 investigated PNF together with the use of medications. Kumar and Bagga22 and Ghous et al.21 investigated the effect of PNF combined with conventional treatment which was defined by Kumar and Bagga22 as the use of galvanic current stimulation (100 ms, 3 series, and 30 contractions) with manual facial massage. Ghous et al.21 did not provide a clear description of their conventional treatment. Khanzada et al.24 investigated the effect of PNF associated with nerve stimulation. From the five studies included, only one described the region in which PNF was administered.20
In two studies the comparator group received drug therapy consisting of antivirals and corticosteroids, with only one study describing the complete dosage.20 Barbara et al.20 used antiviral drugs (Aciclovir 400 mg, three times per day) administered for 15 days and a full dosage of steroids (prednisolone 40 mg per day) for 10 days and tapered within the next 5 days and Monini et al.23 used steroids, at the dosage of 60 mg per day, for 10 consecutive days and tapered off by 10 mg until suspension. Although Monini et al.23 described the dosage used, the type of steroid administrated was not specified. Kumar and Bagga22 compared PNF with neuromuscular re-education (NRM) and conventional treatment, however, detailed description of this intervention was not provided. Ghous et al.21 used kinesiology tape and conventional physical therapy in the control group, but details about the conventional physical therapy was not provided. Khanzada et al.24 compared PNF with facial exercises associated nerve stimulation, however, like Kumar and Bagga22 and Ghous et al.21 details of the protocol performed were not described.
Based on TIDieR checklist, none of the trials described all items.18 Only 40% of the studies described a justification for the intervention used.21,22 The description of the place where the intervention took place was mentioned in 80% of the studies.21–24 Considering the description of the parameters related to the intervention, only one article described the region in which PNF was administered,20 and details regarding sets, repetitions, and intensity were not reported in any of the studies. The other items evaluated by TIDieR were not met, except for the description of the name of the technique.
Three of the included trials used the House Brackmann Scale20,21,23 for evaluating clinical recovery, severity of paresis, and recovery rate. Two trials21,22 used the Synkinesis Assessment Questionnaire (SAQ) to assess synkinesis. Facial Disability Index (FDI) was used as an instrument for the assessment of facial disability in three trials.21,22,24 One trial23 quantified the recovery time in days and another two22,24 used the Sunny brook Facial Grading Scale (SFGS) to measure facial symmetry. Compound Motor Action Potential was used in an article for assessing nerve conduction velocity.20 Movement, facial comfort, oral function, eye comfort, tear control, and social function were assessed through Beta FACE Scale in only one article.23
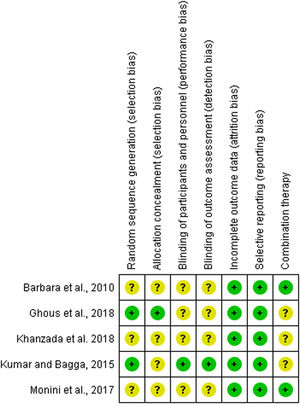
Risk of bias assessmentRisk of bias assessment is presented in Fig. 2. Two studies showed a low risk of bias for randomization sequence generation, while the other three were considered as unclear risk. For allocation concealment, only one study showed low risk of bias and the other studies showed unclear risk. For blinding of participants and blinding of outcomes assessor, only one article showed low risk for both items. For the incomplete outcome data and selective reporting bias, all five had a low risk of bias. The evaluator included the bias of using combined therapy, because some studies used manual therapy or other physical therapy resources, such as electrotherapy, in association with PNF, therefore two trials were classified as low risk of bias.
Effect of interventionNone of the five studies used PNF as the sole intervention. The included trials were substantially heterogeneous in terms of intervention, comparators and outcomes, so we presented the trial results separately for each study.
PNF plus drug treatment versus drug treatmentTwo trials investigated the combination of PNF with drug treatment compared to drug treatment. Monini et al.23 compared PNF plus steroids with steroids only. Patients who received PNF with steroids (n = 38; mean time to recover= 70 days) showed a faster clinical recovery than those patients receiving steroids alone (n = 66; mean time to recover= 124 days). Barbara et al.20 compared PNF with antiviral plus steroids with antiviral plus steroids. Patients who received PNF with drug treatment (n = 9; median score at day 15= 2) showed lower median scores on the House Brackmann Scale compared to the drug treatment group (n = 11; median score at day 15= 4). Lower score in the House Brackmann Scale indicates normal function. Based on the results of these two trials, there is very low quality of evidence that PNF combined with any drug treatment may be more effective than drug treatment alone.
PNF plus conventional physical therapy versus facial exercises and taping with conventional physical therapyGhous et al.21 investigated the effect of PNF with conventional physical therapy (n = 10) on physical function, social function, and synkinesis compared to facial exercise and taping with conventional physical therapy (n = 10). PNF combined with conventional physical therapy resulted in lower score in the physical function (92.7±14.1 versus 106.7±8.7) and social function (43.7±10.7 versus 45.2±13.6) subscales of the Facial Disability Index but higher score in the Synkinesis Assessment Questionnaire (27.8±8.3 versus 21.7±1.9) compared to facial exercise and taping with conventional physical therapy after a course of 5 weeks of treatment. However, because only one single trial with a very small sample size were found, the evidence is very uncertain (i.e. very low quality) about the effect of PNF with conventional physical therapy compared to facial exercise and taping with conventional physical therapy.
PNF plus conventional physical therapy versus facial neuromuscular re-education technique plus conventional physical therapyKumar and Baga22 investigated the effect of PNF combined with conventional physical therapy on physical function, social function, and synkinesis (n = 20) compared to facial neuromuscular re-education technique combined with conventional physical therapy (n = 20) after a course of 4 weeks of treatment. PNF combined with conventional treatment was not superior than facial neuromuscular re-education technique combined with conventional physical therapy in physical (MD= 0.5; 95%CI: -1.7, 2.7) and social (MD= 0.3; 95%CI: -2.4, 2.9) function subscales of the Facial Disability Index. Regarding synkinesis a greater reduction was reported in the facial neuromuscular re-education technique and conventional physical therapy group compared to PNF and conventional physical therapy (MD= 14.0; 95%CI: 11.0, 17.0). Similar to the very low quality of evidence reported for previous comparisons, the evidence is very uncertain about the effect of PNF with conventional physical therapy compared to facial neuromuscular re-education technique with conventional physical therapy.
PNF combined with nerve stimulation versus facial exercise with nerve stimulationKhanzada et al.24 compared PNF combined with nerve stimulation (n = 26) with facial exercises combined with nerve stimulation (n = 26) over a course of 3-week of treatment. PNF combined with nerve stimulation resulted in higher score for facial disability index and the Sunnybrook facial grading scale than facial exercise combined with nerve stimulation. However, as this is a single study, the evidence is very uncertain about the effect of PNF with nerve stimulation compared to facial exercise with nerve stimulation.
DiscussionThe literature search did not identify any study that dealt with central FP, therefore the results of this review are limited to peripheral FP. Based on the available evidence, we were unable to determine the real effect of PNF for treating FP because none of the included studies used PNF as an isolated therapy. Given the small number of studies and the high risk of bias among included studies, the available evidence do not support the use of PNF as an isolated therapy or as an adjuvant therapy to treat FP.
FP has a high rate of spontaneous recovery, even in the absence of treatment, therefore, the probability of recovering from FP is very high.25 When compared to facial exercises or conventional treatment it was not possible to observe better results in the groups treated with PNF.21,22,24 It is important to notice that control groups were composed of exercises and, considering the available evidence, facial exercises may be beneficial in treating FP.26
In view of the lack of information regarding the intervention protocols among included studies, and because this information is extremely relevant for understanding the trial results, replicating the existing studies, and using the intervention in clinical practice, we recommend future studies in this area to provide a detailed description of the interventions. This information should ideally follow the TiDIER checklist, including how the treatment was performed, detailed description of the treatment protocols (i.e., components and exercise), and duration/frequency/amount of treatment.
In addition, the risk of bias assessment in this review revealed that nearly half of the items were judged as unclear. The unclear information about the trial methodology reinforce the need of future high quality trials in this area.
We, therefore, recommend future high-quality trials to investigate the effect of PNF as a single intervention compared to placebo or no intervention or to investigate the effect of PNF in combination with other intervention only if the control arm include this other intervention with no PNF or sham PNF. This trial designs would allow us to determine, respectively, the real effect of PNF or the effect of PNF as adjunct therapy for FP. The available evidence was rated as very low quality of evidence which suggest that, at present, we are uncertain about the effect of PNF in treating FP.
LimitationsThis available evidence is limited by the number of studies available for inclusion. In addition, the small sample size in most of the included studies and the lack of detailed description of the intervention protocols make it difficult to draw definitive conclusions about the utility of PNF. Given the heterogeneity of the included studies we were unable to conduct meta-analyses.
ConclusionGiven the limited number of studies included and low methodological quality found in the available literature, we are uncertain about the effect of PNF in treating FP.
Protocol Registration (PROSPERO)CRD42017068744.