The Star Excursion Balance Test (SEBT) is commonly used for testing dynamic balance in chronic ankle instability (CAI) in both clinical and research settings. However, the effect of verbal encouragement (VE) on the SEBT performance is not known.
ObjectiveTo investigate the effects of VE on maximum reach distance performance between CAI and healthy participants on the SEBT.
MethodThirty-four college-aged adults, 17 with CAI and 17 healthy controls, performed the SEBT in the anterior, posteromedial, and posterolateral reach directions. Independent variables (VE versus No-VE) and group (CAI versus healthy) were analyzed using Analysis of Variance (ANOVA) to determine whether VE and group affected reach performance.
ResultsThere was a significant group-by-condition interaction (p = 0.02) for the anterior as well as for the posteromedial reach (p = 0.04). There was no statistically significant interaction (p = 0.48) for the posterolateral reach. There were moderate to large effect sizes in the reach distances found in the No-VE condition between the CAI and healthy controls, but with VE, the range of effect sizes from No-VE to VE were diminished.
ConclusionThere was a significant group by condition interaction for anterior and posteromedial reaches which shows that providing VE resulted in a greater increase in performance for participants with CAI compared to healthy controls. Psychological constraints need to be considered while performing and interpreting the results of the SEBT.
Ankle sprains are the most common injury in sport,1 with an annual health care cost of $4.2 billion per year in the United States.2 Lateral ankle sprains, which result from an inversion and/or plantar flexion mechanism, account for the majority of all ankle sprains.3 Individuals who suffer from an ankle sprain often have difficulty attaining their pre-injury functional level and have a higher incidence of recurrent ankle sprains.4 Moreover, 40% go on to develop chronic ankle instability (CAI) within the first 12 months of sustaining the first ankle sprain.5 The term CAI is an umbrella term that includes mechanical and functional instability, along with residual symptoms including pain and giving away.6 Dynamic balance deficits are common in lower extremity injuries, especially in patients with CAI, resulting from damage to the afferent mechanoreceptors in the lateral ligament complex, causing somatosensory impairments.6,7
Poor dynamic balance leads to falls and repeated injuries following ankle sprain.4 Any dysfunction to the primary sensory systems (visual, vestibular, and somatosensory) results in balance deficits.8 Assessment of dynamic balance deficits in patients with CAI can generate valuable insight for clinicians; one simple method that assess dynamic balance is the Star Excursion Balance Test (SEBT).9 In addition to balance, performance on the SEBT requires strength, flexibility, range of motion (ROM), and proprioception.10,11 Individuals with CAI have been shown to exhibit significantly lower reach distances in the SEBT compared with healthy controls, perhaps also because of decreased ROM in the hip, knee, and ankle.9,10
Individuals with CAI are also reported to suffer from kinesiophobia and fear of re-injury in addition to the somatosensory and ROM deficits.12 Houston et al.12 described a heightened fear of re-injury during movements, ultimately resulting in diminished function and more disablement in this population.12 In the literature, there is little emphasis on the psychological aspects in ankle dysfunction such as CAI, although kinesiophobia and fear-avoidance are related to a poor prognosis in a variety of musculoskeletal conditions such as low back pain.13
Increased fear is used synonymously with a lack of confidence in performing motor tasks.14 Extrinsic motivation, such as verbal encouragement (VE), has been shown to improve confidence, which may decrease the fear of movement, and thereby enhance motor performance.15 Previous researchers have shown an increase in performance in motor tasks performed with VE, such as an increase in force production in elbow flexion when VE was given.16 This may be because VE can activate higher brain centers such as cerebral cortex and limbic system that can help an individual overcome the mental constraints developed because of the chronicity of the injury.16 Verbal encouragement during a motor task is also associated with greater attentional focus on the task, and subsequently better performance.15 Thus, we aimed to examine the effect of VE on a dynamic motor task (SEBT) in a group with CAI and compare those effects with a healthy control group. This will help us understanding if outside encouragement during the SEBT can change the performance of individuals with CAI on the SEBT to identify if limitations have a psychosocial component. We hypothesized that participants with CAI would perform better on the SEBT with VE as compared to No-VE by improving focus and confidence during the task.
MethodsThis case-control, repeated measure, laboratory study was approved by the Institutional Review Board of the University of Virginia (#19712)
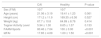
A total of 34 college aged recreationally active individuals (17 with CAI, 17 healthy) were recruited from a public university. An a-priori power analysis revealed that 16 participants were required to achieve 80% power at an alpha level of 0.05. We based our sample size on previous research by McKeon et al.,17 using the posteromedial reach of the SEBT in participants with CAI, an effect size of 1, a standard deviation of 0.14, and magnitude of difference of 0.14. Recreationally active was defined as participation in some form of physical activity at least 20 min a day, for at least three times a week.18Table 1 details the group demographics. Healthy controls were included if they met the following criteria: 1) no history of previous ankle sprains or any other lower extremity orthopedic injury or neurological injury, 2) reported a score of >95% on the Foot and Ankle Ability Sport Scale (FAAM-sports),19 and 3) <4 on the Identification of Functional Ankle Ability Instability (IdFAI).20 Inclusion criteria for the CAI group were: 1) history of at least one previous ankle sprain (initial sprain at least 1 year prior to participation) and 2) a score of <85% on FAAM-sports19 and a score of >10 on the IdFAI.20 In participants who reported bilateral CAI, the self-identified “worst ankle” was used as the test ankle. Exclusion criteria for both groups included any history of other lower extremity injuries or fracture, any balance disorders, or any neurological problems. Participants were matched based on sex, height, weight, and activity level. The study was conducted according to the Declaration of Helsinki and a written informed consent was obtained prior to participation. Participants completed demographic forms (age, sex, injury history sheet, activity level), and anthropometric measurements were taken (height, weight, limb length, dominant limb) prior to performing the SEBT.
Population demographics and anthropometrics.
Note. M/F, males/females; CAI, chronic ankle instability; FAAM, Foot and Ankle Ability Measure; IdFAI, Identification of functional ankle instability measure.
Values are mean ± standard deviation.
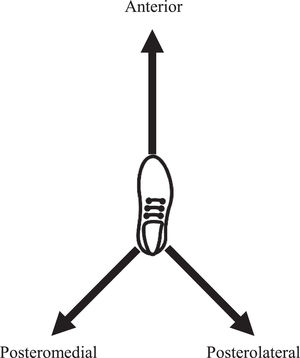
The SEBT is a reliable (ICC = 0.84 to 0.87) test for assessing dynamic balance in three specific directions: anterior, posteromedial, and posterolateral (Figure 1).21 Participants maintained their hands on their iliac crests while performing the task and were instructed to keep their foot flat on the ground while balancing on their stance limb, and reaching as far as they were able with the opposite limb. Measures were taken in each of the three directions without the participant transferring any weight on the reaching limb. While shod, they placed their feet so that their toe was at the zero mark of the anterior reach line for the anterior reach. For posteromedial and posterolateral reach distances, the heel was placed at the zero point of the anterior reach line. The distance from the zero mark to the point of toe touch was measured for each trial. Participants repeated a trial if one of the following occurred:1) stance foot lifted off the ground, 2) hands were removed from their iliac crest, 3) the reach foot did not touch the surface, 4) the reach foot applied or transferred body weight onto the floor, or 5) the participant lost their balance.21 Leg length was measured from the anterior superior iliac spine to the medial malleolus. The averages of the reach distances (cm) were divided by leg length and multiplied by 100 for each individual to normalize the SEBT scores.21 Normalization was done to control for the differences in the reach distances because the performance on the SEBT has been shown to be affected by leg length.21
Verbal encouragementFor VE, participants performed the same test but while being given commands like “go, go, go,” and “go as far as you can.” Participants were blinded to their reach distances during all trials, and to the overall purpose of the study. Verbal encouragement has been shown to change intrinsic motivational status, inducing putative greater motivation that consequently can affect maximal effort.22,23 Therefore, trial order was not randomized, consistently performing the No-VE condition first followed by the VE condition.
In lieu of a randomized order to mitigate a potential learning effect, a minimum of four practice trials were performed in each direction prior to the first No-VE test. Practice trials were completed until there was no observable change in reach distances between successive trials. Four to six trials has been shown to eliminate further learning effect.24 Similar methods have been used previously by Rendos et al.25 for this purpose. The average of the three measurements was used in the subsequent analysis. The same investigator with five years of experience using the SEBT in clinical and research settings administered all tests.
Data analysisDescriptive statistics were calculated using Minitab 17 (Minitab Inc. State College, PA). A two-sample independent t-test was used to compare demographics of the two groups. SPSS for Windows version 21.0 (SPSS Inc Chicago,IL) was used to run three separate 2 by 2 mixed-model repeated-measures Analysis of Variance (ANOVA) to assess differences in the two conditions (VE and no-VE) and between the healthy (n = 17) and CAI (n = 17) groups for each of the three SEBT reach distances (anterior, posteromedial, posterolateral). Cohen's d effect sizes were calculated to determine the magnitude of difference between the CAI and the healthy groups in the No-VE conditions and then in the VE condition. Effect sizes were interpreted as follows: <0.2 trivial; 0.2 to 0.4 small; 0.5 to 0.7 moderate; ≥ 0.8 large.26
ResultsThere were no statistically significant differences (p>0.05) with respect to height, weight and activity level between the two groups. But, FAAM-sports and IdFAI scores were significantly (p<0.05) higher in the CAI group compared to the healthy group (Table 1).
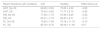
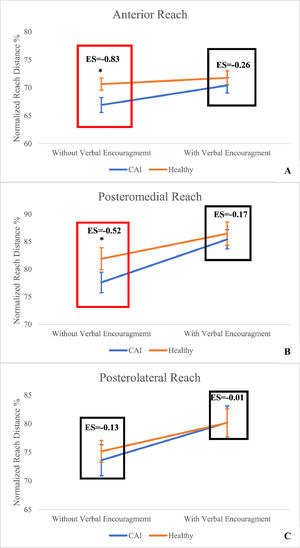
There was a statistically significant group (CAI, healthy) by condition (VE, No-VE) interaction for both the anterior (p = 0.02) and posteromedial (p = 0.04) reach directions (Fig. 2a and b) where the reach distances in the CAI group were less, especially when there was no verbal encouragement. There was no statistically significant interaction (p = 0.48) for the posterolateral direction reach distances (Fig. 2c). There was no statistically significant (p = 0.8) group main effect for posterolateral direction. However, there was statistically significant (p<0.05) main effect for condition for the posterolateral direction. Large effect size was observed in the No-VE condition for anterior reach d=−0.83 and posteromedial reach d=−0.52, which decreased to d= −0.26 and d=−0.17, respectively when VE was provided. A trivial effect size of d=−0.13 was found in no-VE condition for the posterolateral reach that further decreased to d = 0.01 under the VE condition (Table 2).
Reach distances and effect sizes.
ANT, anterior; CAI, chronic ankle instability; No-VE, No verbal encouragement; PL, posterolateral; PM, posteromedial; VE, with verbal encouragement.
Values are mean ± standard deviation for reach distances as a% of leg length.
To our knowledge, this is the first study to investigate the effects of extrinsic motivation given as VE on SEBT performance in individuals with CAI. Consistent with previous work,27,28 we found the CAI group to have lower reach distances than healthy controls. The results of the study showed that the two groups responded differently to VE (Fig. 2A and B). Providing VE resulted in a statistically significant greater improvement of reach distance in the CAI group compared to the control group for the anterior and posteromedial reach distances. This difference in response may indicate a psychological component, often overlooked, when testing reach performance on the SEBT for the CAI group. We did not find a statistically significant interaction for the posterolateral direction. However, we did observe statistically significant improvement in posterolateral reach distance for both CAI and healthy group.
Although deficits in reach distances are often attributed to deficits in dynamic balance or ROM in individuals with CAI,9,29 there may also be psychological constraints associated with the pathology. Thus, comparing reach distances with and without VE helped discern this effect. The CAI group demonstrated poor performance on reach distance of the SEBT with No-VE, but an improvement was seen following VE. Therefore, the differences between the injured and healthy group have considerable clinical importance while interpreting the SEBT. The magnitude of difference (effect sizes) between the two groups for anterior and posteromedial reach distances became smaller when VE was given and the CAI group performed more like the healthy group when VE was given (Fig. 2A and B). It was also interesting to note that reach distance for both groups increased for posterolateral direction and the two groups did not behave differently to VE for posterolateral direction. The difference in performance because of VE in anterior and posteromedial direction between the two groups that was not seen in the posterolateral direction may be because of greater ability of the anterior and posteromedial directions to detect reach difference deficits in people with CAI.27,28
Previous investigation have shown that patients with CAI have higher fear of movement compared to healthy people.12 It is also shown that psychological stresses and mood disturbances can affect postural control.30 Furthermore, psychological stresses like anxiety can alter the postural control resulting in greater postural instability.30 Ohno et al.30 found that there was positive correlation between anxiety levels and the center of pressure (COP) sway in participants. In our study, VE purportedly helped participants in the CAI group to reduce their fears and increase their confidence, as evidenced by the lack of difference in performance with VE. Similarly, it has been shown previously that there was an increase in the mean peak force in the elbow flexors when VE was given to the participants.16 VE increases motivation, and is processed in cerebral cortex and limbic system, breaking the mental barriers developed over the period of time because of injury.16 Similar to maximal force, maximal reaching distance may also require a certain aspect of motivation, while fear of movement, speculatively, may limit dynamic postural control in patients with CAI.
Patients with CAI use less movement through their hip, knee, and ankle while performing SEBT than healthy participants, which may affect their performance on the SEBT.10 Another potential explanation of differences in performance between two groups is that VE might have also reduced the discomfort associated with the limitations in ROM, subsequently allowing increases in the maximal distance. Research has demonstrated that hearing a sudden loud noise decreases supraspinal inhibitions and therefore enhance performance.16 It has also been reported that VE increases the focus on the motor task and also increases the activity in higher brain centers.15 This provides the potential explanation of how VE might have helped the participants with CAI to overcome fear avoidance that has been previously reported in this group of patients,12 and possibly was the reason in increase in reach measurements. These results also raise concerns on the validity of the SEBT as a test for detecting proprioceptive differences. Previously observed differences in SEBT performance of patients with CAI have been primarily attributed to proprioceptive deficits that may not be true based on current findings. It also directs the clinicians and researchers to develop new dynamic balance testing procedures that can challenge fast acting mechanoreceptors, and test proprioception.7,18,31
There are certain limitations to these findings. At this time, it is also unclear how the personality type of an individual can contribute to their psychological barriers that they may have developed because of injury. It is possible that certain individuals may develop a confrontation strategy to their injury and may not consider it very serious, consequently not reducing their physical activity while others may exaggerate the injury in their mind and develop fear of movement. Personality type was not assessed in this study and could have impacted current findings. In addition, we did not measure lower extremity ROM and strength and do not know if participants displayed lower extremity impairments in these variables. Although, we tried to eliminate the learning effect by providing enough practice trials for the SEBT performance but still lack of randomization remains one of the limitations of this study. Another limitation of this study is using a large effect size of 1 for calculating the sample size which may have resulted in underpowering this study. Future research should focus on determining the relationship between the severity of injury (Grade1, Grade 2, Grade 3 ankle sprain) and its effect on injury-related fear and kinesiophobia. It will also be interesting to examine if there is any change in the perception of effort of certain physical tasks after injury that may affect individual`s physical activity levels.
ConclusionThere was a significant group by condition interaction for anterior and posteromedial reaches which shows that the performance of participants with CAI was more influenced by VE as compared to healthy controls. The differences in dynamic balance between the two groups became inconspicuous when VE was given to both groups. Clinicians and researchers should acknowledge the psychological stresses that patients experience post-injury while interpreting the results of the SEBT.