Overweight and obesity are associated with musculoskeletal pain, particularly in the female population. However, regular resistance training may positively affect these complaints.
ObjectiveThe present study aimed to investigate between group differences in musculoskeletal pain in previously inactive women, allocated to three different resistance-training modalities available in health- and fitness clubs.
MethodsThis is secondary analysis from a single-blinded randomized controlled trial, including healthy women (aged 18–65) with a BMI (kg/m2) ≥25. The participants were allocated to 12 weeks (3 times/weekly) of either BodyPump (high-repetition low-load group session) (n=24), heavy load resistance training with a personal trainer (n=28), non-supervised heavy load resistance training (n=19) or non-exercising controls (n=21). Primary outcome was self-reported musculoskeletal pain in ten different body parts, measured with the Standardized Nordic Pain Questionnaire, at baseline and post-test. In addition, the study included sub-analyses of the participants when they were divided into high (≥28 of 36 sessions, n=38) and low (≤27 of 36 sessions, n=22) exercise adherence.
ResultsThe analysis revealed no between group differences in musculoskeletal pain in any of the ten body parts. The results did not change when the participants were divided into high versus low adherence.
ConclusionsTwelve weeks of BodyPump, heavy load resistance training with a personal trainer and non-supervised heavy load resistance training did not show any effect on self-reported musculoskeletal pain in overweight women.
Clinical Trial registration number: NCT01993953.
Being overweight (body mass index (BMI)≥25.0kg/m2) and obese (BMI≥30.0kg/m2) are common contributors to pain and disability in the musculoskeletal system,1–7 especially in the female population.3 With 40% of women worldwide classified as overweight8 and 15% as obese,9 the association between pain and BMI may evolve as an increasing challenge for the health care system.4
The pain-BMI association is primarily explained by increased mechanical load on joints and tissues, muscular inflammations and psychological issues.6,10,11 Consequently, individuals experience reduced physical ability and activity of daily living (ADL), as well as impaired quality of life.12 In addition, overweight and obese women have previously reported fear of pain or injuries during exercise as a major barrier for a more active lifestyle, as well as an important deterrent for adherence to exercise.6 However, physical activity, and especially resistance training, may prevent or reverse pain symptoms by increasing muscle mass, muscle strength and physical function,12–14 help stabilizing the joints, improve mobility and improve proprioception.4
Resistance training can be practiced in many different ways, e.g. with a large range in repetitions and loads, and in different exercise settings (individually and in groups). In the current physical activity recommendations, overweight and obese individuals are recommended to perform resistance training 2–3 times/week, with an intensity between 60 and 80% of maximal muscle strength.15 However, high-repetition low-load resistance training sessions in groups, e.g. BodyPump, are popular exercise programs for women.16 Worldwide, BodyPump is distributed to over 14000 fitness clubs, and weekly over 5 million individuals participate in a session.16 We have previously reported17 that 12 weeks of BodyPump was ineffective in improving muscle strength and body composition in overweight and obese women, compared to an inactive control group. In addition, we found that supervised heavy-load resistance training, in accordance with the American College of Sports Medicine (ACSM) recommendations, effectively improved muscle strength, and provided significantly higher exercise adherence, compared to non-supervised resistance training and BodyPump.17 However, we have not been able to find studies examining whether popular resistance training modalities, available in health- and fitness clubs, affect self-reported pain in overweight or obese women. Hence, the aim of this secondary analysis was to investigate the effect of three different resistance training modalities, compared to controls, on musculoskeletal pain, in overweight and obese women. Furthermore, we aimed to study whether the results were influenced by adherence to exercise.
Material and methodsStudy designThis is secondary analysis of a four armed assessor blinded randomized controlled trial (RCT).17 In the present study, primary outcome was to examine between group differences in musculoskeletal pain in previously inactive women with BMI≥25.0, allocated to twelve weeks of either BodyPump, heavy load resistance training with a personal trainer, non-supervised heavy load resistance training or no exercise. Secondarily, we examined whether there were differences in musculoskeletal pain between those reporting low versus high exercise adherence.
Study populationParticipants were recruited via various social media channels and the homepage of the Norwegian School of Sport Sciences (NSSS). In total, 195 women contacted the principal investigator by phone or email. After aims and implications of the study were explained, eligibility criteria checked and a check-off health-profile scheme including health issues contraindicated for participation was fulfilled, a final sample of 143 participants were included. These participants were randomly allocated with concealed envelopes to either BodyPump (BP) (n=37), heavy load resistance training with a personal trainer (PT) (n=35), non-supervised heavy load resistance training (NS) (n=35) or a non-exercising control group (C) (n=36). An independent statistician performed block randomization, using a computer generated random numbers and an 8-persons block size, meaning that for every eight randomized person each block had two participants with the same intervention. The first 140 included participants were randomized with n=35 in each group. Then, three more participants were included, randomized from a new 8-person block, giving different n in the four groups. Eligibility criteria's included BMI≥25.0, ages between 18 and 65 years and not regularly exercising defined as “not performing regular structured exercise≥twice a week the last six months”.18 Using a inclusion screening scheme, participants were excluded if they had a history of diseases or injuries being contraindicated for the assessments or intervention (e.g. low back pain with radiation or osteoarthritis during the last six months, osteoporosis, secondary hypertension, history of coronary heart disease, stroke, arrhythmias, diabetes type 1 and neurological diseases). In addition, planned vacation or absence from exercise during the intervention period for >2 weeks, pregnancy, obesity surgery or psychiatric diseases were exclusion criteria's.
The study was prospectively registered in the Clinical Trial.gov Protocol Registration System (NCT01993953) and was approved by the Regional Committee for Medical Research Ethics Norway, Oslo (REK 2012/783). The procedures followed the World Medical Association Declaration of Helsinki, and all participants signed a written consent statement before entering the study.
Procedures and interventionsThe participants were prescribed three exercise sessions weekly for twelve weeks, and the exercises were performed in a real life setting. Participants in the BP group had free access to several health- and fitness clubs offering BodyPump during the intervention period, while participants in the PT and NS group exercised at the health- and fitness club at the university.
BodyPump is a pre-choreographed, strengthening workout session, guided by a LesMills certified instructor. Every third month Les Mills releases a new program, but they are all based on the same principles and have the same structure.16 During the intervention period, BodyPump release no.83 was present at all fitness clubs (Table 1). Each BodyPump session consists of ten music tracks, 4–6min each, including strengthening exercises targeting specific muscle groups. The participants exercise with a weight bar (1.25kg), plates (1, 2.5 or 5kg) and a step. In total, each 1-h session includes between 800 and 1000 repetitions, in the range of 50–100 repetitions in each muscle group. There are 1–2min rest periods between each track, used to change weights and prepare for the next exercises. Training loads were self-selected, based on technique and intensity guidance from the instructor, as well as experiences from previous exercise sessions.16
Exercise program BodyPump.
| Music nr. | Exercise | Volume (Reps) |
|---|---|---|
| 1 Warming-up | Straight leg deadlift, rowing, shoulder press, squat, lounges and bicepscurl | 88 |
| 2 Leg | Squat | 95 |
| 3 Chest | Bench press | 80 |
| 4 Back | Rowing, stiff legged deadlift, clean & press and power press | 75 |
| 5 Triceps | French press, tricepspress, pullover and overhead tricepspress | 78 |
| 6 Biceps | Bicepscurl | 68 |
| 7 Leg | Squat, lounges and squat jump | 72+24 jumps |
| 8 Shoulders | Push up, lateral raise, rowing and shoulderpress | 76+36 push up |
| 9 Stomach | Sit-ups, sit-ups to the side and side-plank | 51+30s |
The PT- and NS group followed a standardized nonlinear periodization program, including similar exercises as the BodyPump program. However, the number of repetitions and sets continuously varied; 8–10 repetitions in session one, 13–15 repetitions in session two and 3–6 repetitions in session three. In week 1–4 the participants performed two sets in all the exercise, in week 5–8 they performed 2–3 sets, and in week 9–12 they increased to 3–4 sets. The rest periods varied between 60 and 120s, with longest rest period in the heaviest sessions. At the beginning of each exercise session, the participants performed a 5–10min low intensity warm-up on a treadmill or cycle ergometer. Details of the program have been previously reported.17 The participants were instructed to perform repetition maximum (RM) in each set, with proper lifting technique. Sixteen personal trainers took part in the study, all educated with a bachelor degree in physical activity and health, including a personal trainer certificate from our university. Participants in the PT group exercised together with their personal trainer in all sessions, and received continuously advice on appropriate training loads and lifting technique, as well as support and motivation during exercise. Participants in the NS group exercised on their own, except of one introduction session with a personal trainer who introduced them to the exercise program (proper lifting technique, training loads and progression), and a follow-up session after six weeks of exercise.
Participants in the C-group were asked to continue their usual lifestyle and ADL. If they performed any exercise or physical activity, they were asked to report this in a similar training diary as the intervention groups. After post-test, all controls were offered BodyPump classes for twelve weeks, and one resistance training session with a personal trainer.
AssessmentsMusculoskeletal painMusculoskeletal pain was registered using the Standardized Nordic Pain Questionnaire (SNQ), developed to measure the prevalence of musculoskeletal pain and syndromes in epidemiological studies.19 The questionnaire registers whether the participants have experienced musculoskeletal pain in ten different anatomical body parts, during the last twelve months, and the last seven days. The participants self-reported the questionnaire at baseline (before randomization) with a blinded assessor present. At post-test, the same procedure was followed, but this time the participants were not blinded. For the purpose of the present study, responses to the last seven days were used as the primary outcome. In addition, responses the last twelve months were used in the descriptive analysis at baseline. The ten anatomical body parts included in the questionnaire were; head, neck, shoulder, elbow, wrist, low back, upper back, hip, knee and feet. All questions were formulated as e.g. “Have you ever during the last 12 months/7 days experienced pain in the…?”. Possible responses were yes or no, and those who answered “yes”, were categorized as having pain. The SNQ questionnaire have demonstrated adequate test-retest reliability (0–23% variation), and has previously been validated against clinical history with a variation between 0 and 20%.19
AdherenceThe participants self-registered adherence to exercise in a training diary. For the purpose of this study, high adherence was defined as ≥75% attendance to exercise (≥28 sessions of 36 possible), as this represented minimum two exercise sessions weekly. Low adherence was set at ≤75% (≤27 sessions of 36 possible).
Statistical analysisAnalyzes were done with SPSS statistics program, version 21 (IBM Corporation, Route, Somers, NY, USA). Background data are presented as means with standard deviations (SD), and data on self-reported pain is presented as numbers (n) with percentages (%). One-way ANOVA was used to analyze possible differences between the groups in background variables and primary outcome. An attrition rate analysis of baseline characteristics between completers and non-completers was made with an independent t-test. Because of a high drop-out and low exercise adherence among our participants, results are presented for completers only (i.e. per-protocol analysis). McNemar's test was used to analyze if there was a difference in the proportion of the participants (the three intervention groups collapsed together) reporting muscle pain in any of the body parts prior to, versus after the intervention. Chi-square test was used to analyze differences between the groups in self-reported pain (categorical data), as well as the differences in pain (yes/no) and high/low adherence. The percent difference between the groups was estimated with a 95% Wald confidence interval with Bonett–Price adjustment. Level of statistical significance was set at p<0.05.
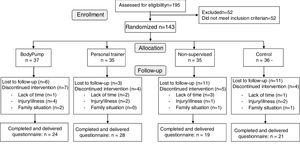
ResultsOf 143 women randomized, 92 completed the study (mean age 39 years±10, BMI 31±5kg/m2), with the following distribution: BP (n=24, 65%), PT (n=28, 80%), NS (n=19, 54%) and C (n=21, 58%) group (Fig. 1).
No statistically significant differences were found between the four groups in background data or musculoskeletal pain (Table 2), nor in the attrition rate analysis between completers and non-completers. Of totally 36 exercise sessions prescribed, adherence to exercise were 54% (±20) in the BP group, 83% (±15) in the PT group and 69% (±20) in the NS group. The adherence was significantly higher in the PT group compared to the BP group (29±5%, p≤0.001, 95% CI 15.5–41.5) and the NS group (13.8±5%, p=0.031, 95% CI 1.0–26.7), and in the NS group compared to the BP group (14.7±6%, p=0.041, 95% CI 0.5–28.9).
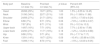
Demographic data of the participants in the BodyPump group (BP), personal trainer group (PT), non-supervised group (NS) and control group (C).
| Variable | BP (n=24) | PT (n=28) | NS (n=19) | C (n=21) |
|---|---|---|---|---|
| Age (year) | 38 (11) | 37 (9) | 42 (12) | 40 (12) |
| Weight (kg) | 83 (11) | 94 (21) | 85 (14) | 87 (15) |
| Height (cm) | 168 (6) | 169 (6) | 168 (6) | 167 (4) |
| BMI (kg/m2) | 30 (4) | 33 (6) | 30 (5) | 31 (5) |
| Children (yes) | 21 | 15 | 18 | 20 |
| Daily smoker | 9 | 2 | 4 | 4 |
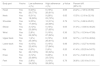
There were no between-group differences in musculoskeletal pain in any of the body parts at post-test (Table 3). Therefore, the prevalence of pain in the different body parts in the three intervention groups are collapsed and presented in Table 4. The analysis showed no statistical significant changes in reported pain from baseline to post-test. At baseline, the body parts with the highest reported pain was the neck, head, shoulder and lower back. At post-test, the highest prevalence was reported in the neck, shoulder, head and knees (Table 4).
Self-reported musculoskeletal pain at baseline and post-test in the BodyPump group (BP), personal trainer group (PT), non-supervised group (NS) and control group (C). Differences between the groups analyzed with chi-square test, presented with p-value. Presented as numbers reporting pain (n)/of the total number of participants (n) in each group, and as percent (%).
| Body part | Baseline BP n (%) | PT n (%) | NS n (%) | C n (%) | p-Value | Post-test BP n (%) | PT n (%) | NS n (%) | C n (%) | p-Value |
|---|---|---|---|---|---|---|---|---|---|---|
| Head | 8/31 (26%) | 10/32 (31%) | 8/25 (32%) | 8/31 (26%) | 0.92 | 8/24 (33%) | 7/28 (25%) | 1/19 (5%) | 8/21 (38%) | 0.09 |
| Neck | 10/31 (32%) | 8/32 (25%) | 13/27 (48%) | 12/31 (39%) | 0.30 | 11/24 (46%) | 6/28 (21%) | 5/19 (26%) | 4/21 (19%) | 0.16 |
| Shoulder | 8/31 (26%) | 9/32 (28%) | 7/28 (27%) | 11/31 (35%) | 0.84 | 6/24 (25%) | 9/28 (32%) | 6/19 (32%) | 4/21 (19%) | 0.73 |
| Elbow | 1/31 (3%) | 1/32 (3%) | 4/25 (16%) | 2/30 (7%) | 0.20 | 0/24 (0%) | 4/28 (14%) | 5/19 (26%) | 2/21 (10%) | 0.07 |
| Wrist | 2/30 (7%) | 3/32 (9%) | 2/25 (8%) | 3/30 (10%) | 0.97 | 4/24 (17%) | 4/28 (14%) | 0/19 (0%) | 2/21 (10%) | 0.32 |
| Upper back | 4/30 (13%) | 6/32 (19%) | 4/25 (16%) | 4/30 (13%) | 0.92 | 0/24 (0%) | 5/28 (18%) | 2/19 (11%) | 2/21 (10%) | 0.20 |
| Lower back | 8/31 (26%) | 7/32 (22%) | 9/27 (33%) | 10/30 (33%) | 0.96 | 2/24 (8%) | 5/28 (18%) | 4/19 (21%) | 3/21 (14%) | 0.67 |
| Hip | 5/31 (16%) | 2/32 (6%) | 2/25 (8%) | 3/30 (10%) | 0.60 | 0/24 (0%) | 3/28 (11%) | 0/19 (0%) | 1/21 (5%) | 0.20 |
| Knee | 2/34 (6%) | 5/32 (16%) | 6/25 (24%) | 2/30 (7%) | 0.13 | 3/24 (13%) | 8/28 (29%) | 5/19 (26%) | 2/21 (10%) | 0.25 |
| Feet | 2/32 (6%) | 5/32 (16%) | 3/25 (12%) | 5/30 (17%) | 0.59 | 2/24 (8%) | 4/27 (15%) | 2/19 (11%) | 4/21 (19%) | 0.73 |
The number of participants that reported musculoskeletal pain in the different body parts at baseline and post-test, with the three intervention groups collapsed. Reported as number participants reporting pain (n)/total number of participants (n), and percent (%). Differences from baseline to post-test, analyzed with McNemar's test are presented with p-value, and percent group differences (%) estimated with a 95% Wald confidence interval with Bonett–Price adjustment.
| Body part | Baseline n/n total (%) | Post-test n/n total (%) | p-Value | Percent diff. (95% CI) |
|---|---|---|---|---|
| Head | 26/88 (29%) | 16/71 (23%) | 1.00 | 1.5% (−9.55 to 12.45) |
| Neck | 31/90 (34%) | 22/71 (31%) | 1.00 | 0% (−11.88 to 11.88) |
| Shoulder | 24/89 (27%) | 21/71 (30%) | 0.66 | −4.5% (−17.93 to 9.24) |
| Elbow | 6/88 (7%) | 9/71 (13%) | 0.06 | −7.6% (−14.99 to 0.07) |
| Wrist | 7/87 (8%) | 8/71 (11%) | 1.00 | 0% (−10.3 to 10.3) |
| Upper back | 14/87 (16%) | 7/71 (10%) | 0.23 | 7.7% (−2.93 to 17.86) |
| Lower back | 24/90 (27%) | 11/71 (16%) | 0.18 | −1.2% (−12.23 to 9.88) |
| Hip | 9/88 (10%) | 3/71 (4%) | 1.00 | 0% (−7.17 to 7.17) |
| Knee | 13/91 (14%) | 16/71 (23%) | 0.09 | −10.4% (−20.88 to 0.59) |
| Feet | 10/89 (11%) | 8/70 (11%) | 1.00 | −1.5% (−12.03 to 9.05) |
Sub analyses of participants divided in high (n=38) and low (n=20) exercise adherence and report of musculoskeletal pain, is presented in Table 5. Irrespective of group allocation, there were no statistically significant difference in prevalence of bodily pain between those with high versus low adherence to exercise.
Differences in self-reported musculoskeletal pain (yes/no) and high (≥75%) versus low (≤75%) exercise adherence. Analyzed with chi-square test, and presented with p-value. Differences between the groups estimated with a 95% Wald confidence interval with Bonett–Price adjustment, presented with percent % and 95% CI.
| Body part | Yes/no | Low adherence n (%) | High adherence n (%) | p-Value | Percent diff. (95% CI) |
|---|---|---|---|---|---|
| Head | Yes No | 6 (23%) 20 (77%) | 6 (19%) 26 (81%) | 0.69 | 24.2% (−7.09 to 39.58) |
| Neck | Yes No | 8 (31%) 18 (69%) | 9 (28%) 23 (72%) | 0.83 | 15.5% (−2.18 to 32.18) |
| Shoulder | Yes No | 9 (35%) 17 (65%) | 10 (31%) 22 (69%) | 0.79 | 12.1% (−5.68 to 29.01) |
| Elbow | Yes No | 3 (12%) 23 (88%) | 5 (16%) 27 (85%) | 0.65 | 31.0% (−13.80 to 46.20) |
| Wrist | Yes No | 2 (8%) 24 (92%) | 5 (16%) 27 (84%) | 0.36 | 32.7% (−15.34 to 47.99) |
| Upper back | Yes No | 1 (4%) 25 (06%) | 6 (19%) 26 (81%) | 0.08 | 32.7% (−14.70 to 48.64) |
| Lower back | Yes No | 4 (15%) 22 (45%) | 5 (16%) 27 (84%) | 0.98 | 29.3% (−12.27 to 44.40) |
| Hip | Yes No | 0 (0%) 26 (100%) | 2 (6%) 30 (94%) | 0.20 | 41.4% (−25.25 to 54.75) |
| Knee | Yes No | 3 (12%) 23 (88%) | 9 (28%) 23 (72%) | 0.12 | 24.1% (−5.22 to 41.44) |
| Feet | Yes No | 2 (8%) 24 (92%) | 3 (10%) 28 (90%) | 0.79 | 36.8% (−20.18 to 51.01) |
Assessed for eligibility n=195.
The present study investigated the effect of musculoskeletal pain in untrained women with BMI≥25.0, after twelve weeks of either BodyPump, heavy load resistance training with a personal trainer or non-supervised heavy load resistance training. None of the exercise modalities had effect on musculoskeletal pain, compared to inactive controls, and there were no difference between those with low and high adherence.
The present study included healthy women, and participants with a history of diseases or injuries contraindicated for resistance training were excluded. Hence, we assumed a low to moderate prevalence of musculoskeletal pain at baseline. However, 57 of the 143 participants reported pain in the SQN at baseline, in one or more body parts, with the head, neck, shoulder and lower back being the four most affected body parts. One reason for this, may be that the inclusion screening scheme contained specific diagnoses only (such as low back pain with radiation, osteoarthritis, osteoporosis, secondary hypertension, history of coronary heart disease, stroke, arrhythmias, diabetes type 1 and neurological diseases). Thus, musculoskeletal pain reported in the SQN at baseline, was not considered to be too severe by either the researcher or the participants in the study. Importantly, there were no group differences in self-reported pain in the SQN at baseline, in any of the body parts. In addition, the number of participants reporting pain in one or more body parts in the present study are comparable with prevalence of musculoskeletal pain in the general adult population.20,21 Cimmino et al.20 report that 14–47% of the general population are affected of musculoskeletal pain at any given time, and Stone and Broderick21 report that obese individuals have 20% more daily pain than normal-weighed individuals. In addition, the most affected body parts in our study group have all previously been reported with high risk of pain in overweight and obese individuals.22–25 However, comparison of pain between studies is difficult, due to differences in the definition used, study population and measurement methods.26
The overweight-pain association is related to factors as a sedentary lifestyle, reduced physical function and low muscle strength.2,4,27 Interestingly, several studies have found that resistance training effectively reverse or improve pain symptoms in overweight individuals,1,2,5,6 particularly low-back pain.2,13,14 In the present study, low back pain was non-significantly reduced with 11% from baseline to post-test. Lack of power, low back pain with radiation as one of the exclusion criteria's, low responsiveness of the questionnaire or the content of the program, which had no special focus on treating low back pain, might be explanations why our reduction was somewhat smaller than in other studies.
Unfortunately, the present study had a high drop-out rate. As Herbert et al.28 state that more than 85% of the participants should been assessed and obtained in the main outcome when implementing intention-to treat analysis (ITT),28 we used completers only in the present analysis. In total, seven participants from the three intervention groups dropped out because of illness/injury (Fig. 1). We do not know whether these were exercise-induced injuries, as most of the participants did not give any reason for drop-out. As much as 20 participants were lost to follow-up without reporting reason, the majority of these from the NS group. In addition, the exercise adherence was low in the BP and NS group, which may have affected the outcomes. However, the results did not change when we compared participants with high and low adherence. High drop-out from exercise and low exercise adherence are well-known challenges in overweight and obese individuals.2,6 Interestingly, Zdziarski et al.2 emphasized that exercise modifications, as low load as an alternative of high load resistance training, could reduce acute exercise induced pain, and possibly increase exercise adherence among obese individuals.2 This was not observed in the present study, as the BP group, representing low load resistance training, had significantly lower exercise adherence, compared to the two heavy load groups (PT and NS). However, the fact that our participants exercising with a personal trainer had higher adherence, compared to non-supervised exercise, corresponds with previous findings.6 Arikawa et al.6 compared supervised (month 1–4) and non-supervised (month 5–24) resistance training in untrained overweight and obese women, and found significantly higher adherence during the supervised period.6 Thus, support and motivation from certified personal trainers might be a key-factor to avoid drop-out and increase exercise adherence in this study group.6
Stidsen et al.29 investigated musculoskeletal issues among fitness club members, using the same questionnaire as the present study (SQN). They found that 56% of totally 500 new fitness club members reported musculoskeletal pain in one or more body parts when joining the club, and 77% of these stated that pain was one of the main reasons why they joined the club.29 Thus, it is important to investigate the effect of pain during and after popular exercise modalities available in health- and fitness clubs, especially in risk groups like overweight and obese. Therefore, even though none of the three exercise modalities in the present study significantly reduced self-reported pain after 12 weeks of exercise, we find it important to highlight that no adverse effect was seen. Hence, the resistance training modalities in the present study may all be appropriate for overweight women. This knowledge is important to e.g. physical therapists aiming to include or recommend resistance training among overweight or obese patients. However, it is important to emphasize that resistance training may induce immediate exercise induced pain and give temporary delayed onset muscle soreness (DOMS).30
Strengths of the present study were use of a randomized controlled design, blinded investigator and use of a validated questionnaire. The study had a high external and ecological validity, as the exercise training was performed in a real-life setting, under pragmatic conditions. In addition, all participants followed the same standardized exercise programs, and the personal trainers followed the same standardized instructions. Limitations in the study are the high drop-out and the low exercise adherence in the BP and NS group. In addition, the SNQ do not distinguish between intensity and type of pain. Therefore, the participants may have interpreted the definition of musculoskeletal pain differently, and e.g. confused stiffness, DOMS, fatigue and functional limitations. Questionnaires including pain intensity e.g. the visual analog scale for pain, numeric rating scale for pain, McGill pain questionnaire or the short form 36 bodily pain scale,31 could have given more detailed information.
To conclude, our study showed no between- or within group changes in self-reported musculoskeletal pain after twelve weeks of either BodyPump (high-repetition low load resistance training), heavy load resistance training with a personal trainer or non-supervised heavy load resistance training.
Funding/support statementThe present study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors have no conflicts of interest relevant to this article.
We thank all the participating women, and Ingar Holme and Morten Fagerland for statistical advice.
This paper is part of a Special Issue on Women's Health Physical Therapy.