There is a lack of longitudinal studies investigating the association between cervical flexion posture during smartphone use (commonly referred to as text neck [TN]) and neck pain (NP).
ObjectiveTo investigate whether TN is a risk factor for NP, considering the influence of lifestyle and psychosocial factors.
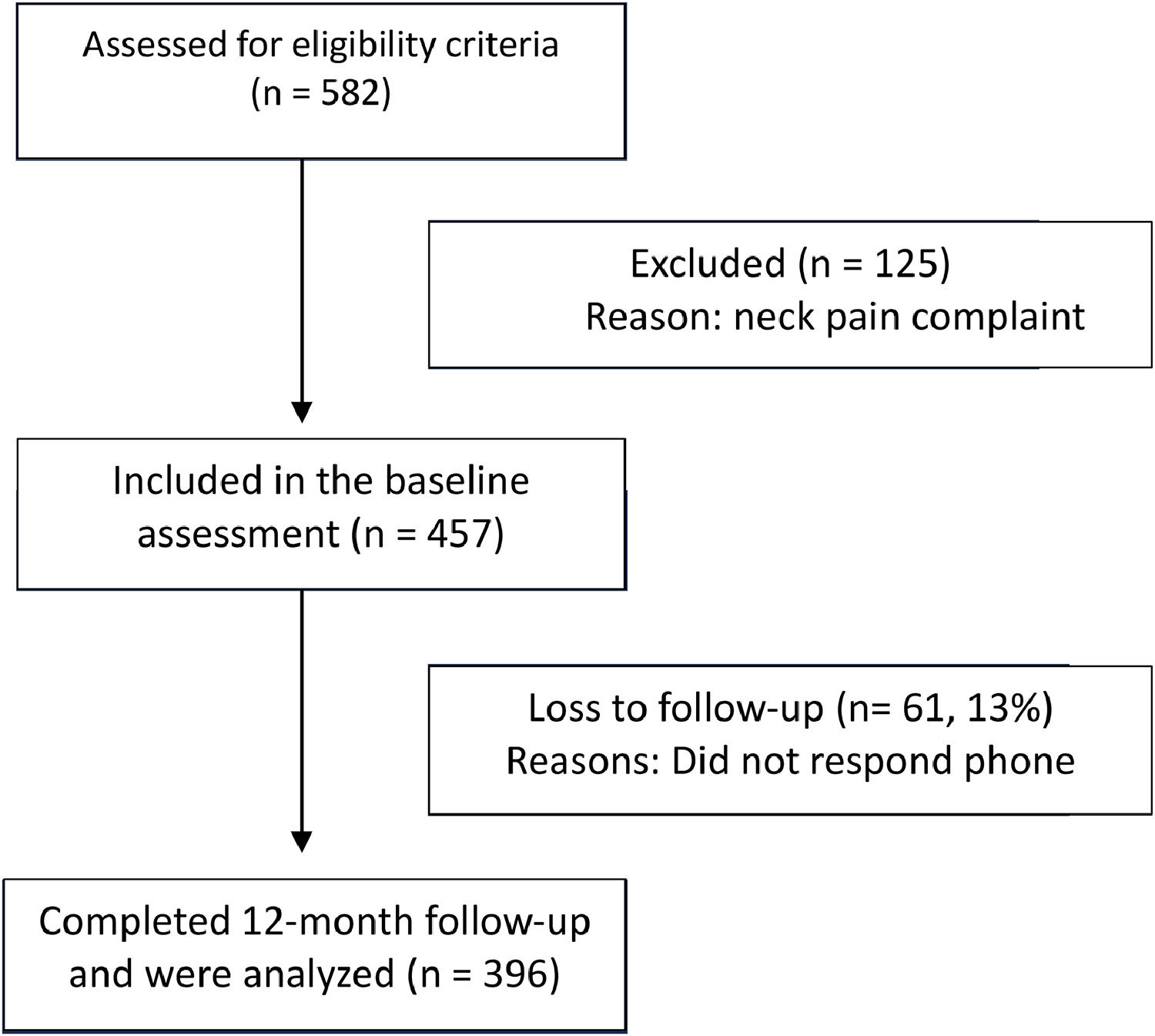
MethodsA 12-month longitudinal study. The sample consisted of 457 volunteers of both sexes, aged between 18 and 65 years, without NP. Sociodemographic, anthropometric, lifestyle, psychosocial, and smartphone-use data were collected through a self-reported questionnaire. TN was assessed objectively at baseline by measuring the cervical flexion angle using the cervical range of motion device (CROM) with participants standing and sitting while texting on their smartphones. One year after the initial assessment, participants were assessed regarding the point prevalence and frequency of NP.
ResultsOf the total, 396 (87 %) participants completed the one-year follow-up. NP was reported by 40 (10 %) participants. Multiple logistic regression analysis showed that TN did not increase the chance of NP (standing OR [95 % confidence interval] = 1.0 [0.97, 1.04]; sitting OR = 1.01 [0.98, 1.04]) or frequency of NP (standing OR = 1.01 [0.99, 1.03]; sitting OR = 1.00 [0.99, 1.02]) after baseline. However, low sleep quality (OR = 1.76 [1.17, 2.63]) and insufficient level of physical activity (OR = 2.41 [1.03, 5.65]) increased the chance of NP.
ConclusionCervical flexion posture during smartphone use was not a risk factor for NP or frequency of NP, but low sleep quality and insufficient levels of physical activity were.
Neck pain (NP) is the fourth cause of disability in the world,1 being one of the main chronic conditions regarding years lived with disability in the age group between 25 and 74 years of age.2 There is a hypothesis that the flexed posture of the neck and head adopted for reading and typing while using a smartphone – called text neck – is harmful and is related to neck pain and other physical symptoms. Recently, a scoping review3 showed that the cervical flexion posture adopted during smartphone use is the defining characteristic of the term text neck. Brazil is ranked as one of the countries with the highest smartphone usage. Brazilian people spend 32 % of their time awake on their smartphones daily. This percentage increases to 56 %, approximately 9 h and 32 min, taking into account the screen time of smartphones and computers combined.4
The relationship between NP and smartphone use emerged by one single computational model study which suggested the premise that the greater the neck flexion, the greater the overload.5 This theory, based exclusively on biomechanics, does not consider that pain is modulated by several factors and must be underpinned in a multidimensional way.6,7 Aspects such as depression, anxiety, sleep quality and level of physical activity are frequently described as risk factors for NP.8–11 In fact, more risk factors are found in psychosocial than physical dimensions for a first episode of NP.12
Previous cross-sectional studies did not find an association between NP and text neck, with students aged 18 to 21 and among adults after quantitative assessment of cervical flexion with a CROM inclinometer in standing and sitting.13 Bertozzi et al.14 also did not find an association between neck posture and time spent on smartphones with NP or disability. A longitudinal study did not find an association between time spent texting on mobile devices and new cases of NP.15 Furthermore, the same study showed that smartphone usage increases the risk of new cases of pain in the hand and fingers. To our knowledge, there is no longitudinal study investigating the association between text neck and neck pain. Hence, the aim of this study was to investigate whether text neck is a risk factor for neck pain, considering the influence of psychosocial and lifestyle factors. Our hypothesis was that text neck is a risk factor for neck pain.
MethodsDesignLongitudinal observational study with 12-month follow-up using a self-reported questionnaire and objective assessment of posture while texting on a smartphone using inclinometer measure at baseline. The follow-up evaluation was carried out after one year through telephone contact, via e-mail, or social networks. This study followed the recommendations of the STROBE Guidelines – Strengthening the Reporting of Observational Studies in Epidemiology.16 The funders played no role in the design, conduct, or reporting of this study.
ParticipantsThe sample consisted of 457 volunteers without neck pain, aged between 18 and 65 years of both sexes. Data were collected by researchers in a tent located in a busy area of the Augusto Motta University Center in Rio de Janeiro from November 2018 to November 2019. Participants were invited to participate through advertising boards next to the evaluation tent.
Assessment measuresAt baseline, a questionnaire was applied containing identification of the research participant with sociodemographic (name, age, and sex) and anthropometric (weight and height) questions. To exclude participants with neck pain at baseline, they were asked: “Do you have neck pain today?” the answer options were: “Yes” or “No”. The amount of time the participant is exposed to smartphone use was assessed through the question, “On a typical weekday, how many hours a day do you spend reading, texting, and playing games on your smartphone?” with nine answer options, the first of which began with, “I only use my smartphone to talk”, and then the answers varied according to the time spent using the smartphone from, “<1 hour per day”, to, “About 7 or more hours per day”. Regarding concerns about their postures, we asked, “Do you worry about your body posture?”, “Do you think your posture is adequate when typing on your smartphone?”, and, “Do you worry about your posture on your smartphone when typing?”, the response options were, “very often”, “often”, “once in a while”, “rarely”, or “never”. We also evaluated visual problems, as the individual's posture can be altered due to the fact that they have compromised visual acuity without the necessary corrections, so we asked, “Do you have vision problems?”, with the answer options, “Yes”, or, “No” and also, “Do you have vision problems and do you wear glasses (or contact lenses)?”, the answer options were, “Yes”, “No” or, “I use them, but I forgot”.
Lifestyle was assessed with questions about physical activity, smoking, sleep quality, and dependence on smartphone use. The short version of the International Physical Activity Questionnaire (IPAQ) assessed the level, weekly frequency, and daily workload of activities, classifying the individual as: sedentary, insufficiently active, active, or very active.17 Smoking was assessed using the question “In the last 30 days, how many days did you smoke cigarettes?” with eight response options ranging from, “I never smoked”, to, “Every day in the last 30 days”. Sleep quality was assessed with the question: “Did you have trouble sleeping in the last month?” with four response options: “none”, “a little”, “some”, or “serious”. Furthermore, the questionnaire also included the Smartphone Addiction Scale18 and psychosocial factors such as anxiety, depression, social isolation, and stress.19
Text neck was assessed by measuring the flexion angle of the cervical spine, with the assumption that the greater the cervical flexion angle, the greater the text neck. It was measured while typing on the smartphone using an inclinometer (CROM – Cervical Range of Motion). The reliability and validity of the CROM were established by Capuano-Pucci20 and Tousignant,21 respectively. The CROM measures cervical range of motion for flexion and extension, lateral flexion, and rotation using three separate inclinometers, each in a sagittal, frontal, and transverse plane, respectively. We only assessed the cervical flexion degree. The participant was instructed to stand on a cross marked on the floor. In the upright position, the CROM device was placed as if putting on a pair of glasses. The participant was asked to send a text message to someone via their smartphone, simulating daily use. The cervical angle measurement with the CROM inclinometer was recorded with the participant in an orthostatic and seated position (Fig. 1). The evaluator was blind to the participants' responses regarding NP results.
The one-year follow-up was carried out by telephone call or text message and included only questions regarding the complaint of neck pain and the frequency of neck pain: “Do you have neck pain today?” The answer options were: “Yes” or “No” and frequency of neck pain: “How often have you had neck pain?” The response options were: “Very often”, “Often”, “Once in a while”, “Rarely”, or “Never”. These responses were dichotomized for regression analysis into 1 – Never and Rarely, and 2 – Occasionally, Often, and Very often.
Sample sizeThis study required a minimum sample size of 430 participants to provide a power of 80 % and an alpha of 5 %, considering a prevalence of 16 % of neck pain in the exposed group and 6 % of neck pain in the non-exposed group at the one-year follow-up.22 Based on the study of Damasceno et al. ,23 the percentage of participants exposed to text neck was 40 %. The estimated sample size also allowed a limit of 15 % loss of follow-up.
Data analysisAll analyzes were performed using version 0.99.486. from RStudio (https://posit.co). Participant characteristics were described using proportions, means, and standard deviations. Four logistic regression models were carried out. The two first evaluated standing text neck, psychosocial variables (anxiety and depression), and lifestyle variables (level of physical activity and quality of sleep) as independent variables with prevalence of neck pain and frequency of neck pain as dependent variables, respectively. The two second ones evaluated sitting text neck and the same psychosocial and lifestyle variables as independent variables with the same dependent variables. Potential confounders, including age, sex, time using the device, and smartphone dependence, were included in the logistic regression models according to what the literature describes as potential risk factors for neck pain and variables related to smartphone use. The significance level adopted in the study was 5 %.
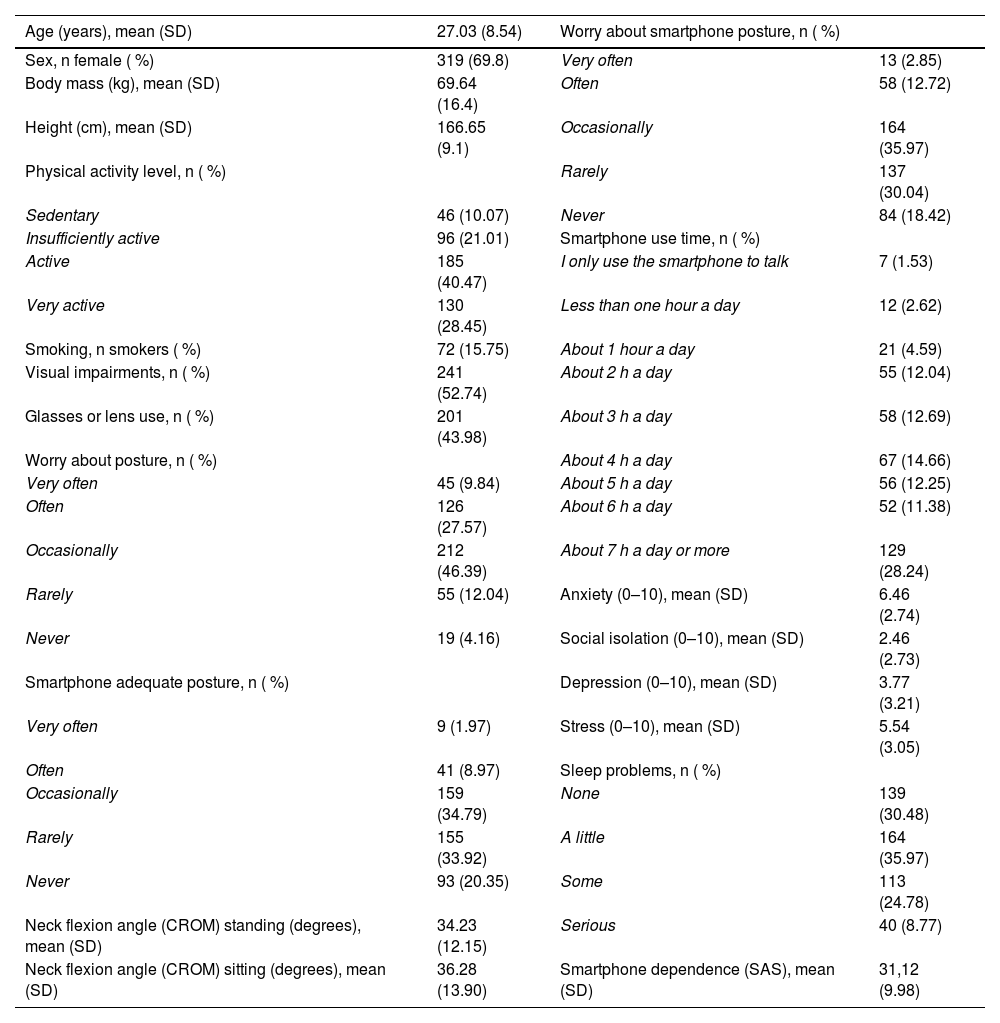
ResultsOf the total, 396 (87 %) participants completed the one-year follow-up (Fig. 2) The presence of NP on the day of reassessment was reported by 40 (10 %) participants. The frequency of NP was “very often” in 4 (1 %), “often” in 20 (5 %), “occasionally” in 129 (33 %), “rarely” in 158 (40 %), and “never” in 85 (21 %) volunteers. The average age was 27 (SD=9) years and 319 (70 %) were female. The average cervical flexion angle of participants using the smartphone was 34° (SD=12°) in the standing posture and 36° (SD=14°) in the sitting posture. Time of use, level of physical activity, concerns about posture, smartphone dependence, and other psychosocial factors are also described in Table 1.
Participants' characteristics (n = 457).
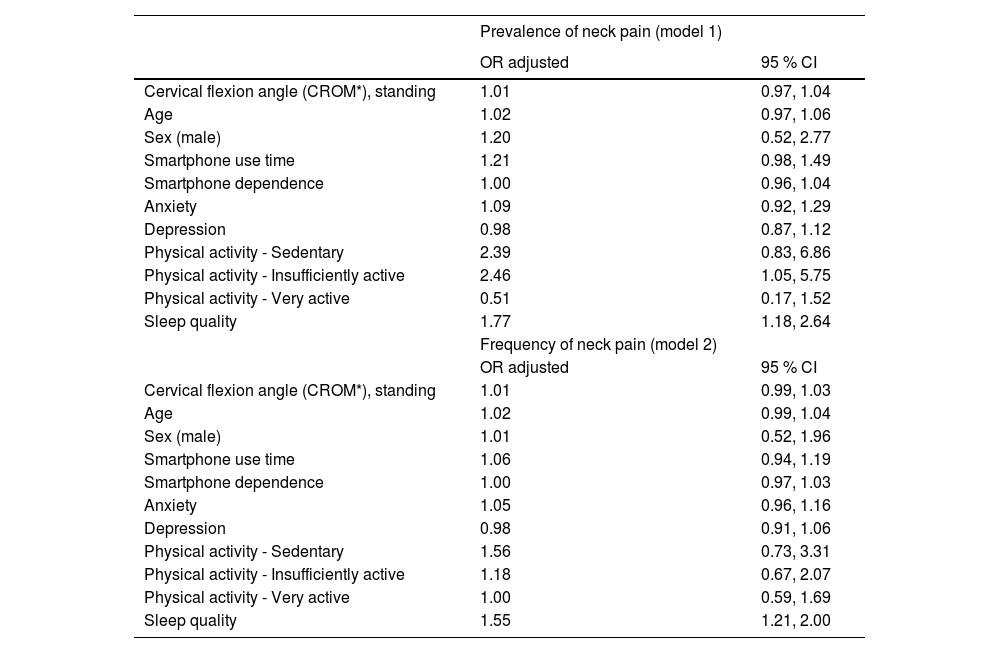
Multiple logistic regression analysis showed that the cervical flexion angle of participants standing using a smartphone did not increase the chance of NP (odds ratio [OR] = 1.01; 95 % confidence interval [CI]: 0.97, 1.04) or frequency of NP (OR = 1.01; 95 % CI: 0.99, 1.03) one year after baseline. Sleep quality increased the chance of NP (OR = 1.77; 95 % CI: 1.18, 2.64) and frequency of NP (OR = 1.55, 95 % CI: 1.21, 2.00). When compared to active participants, those who were insufficiently active had increased chances of NP (OR = 2.46; 95 % CI: 1.05, 5.75). Although it was not statistically significant, there is a suggestion that sedentary individuals have an increased chance of NP (OR = 2.39; 95 % CI: 0.83, 6.86) when compared with physically active participants (Table 2).
Odds ratio (OR) for the association between text neck while standing - assessed by cervical flexion angle - with prevalence of neck pain (model 1) and frequency of neck pain (model 2) considering potential confounders for each model.
| Prevalence of neck pain (model 1) | ||
|---|---|---|
| OR adjusted | 95 % CI | |
| Cervical flexion angle (CROM*), standing | 1.01 | 0.97, 1.04 |
| Age | 1.02 | 0.97, 1.06 |
| Sex (male) | 1.20 | 0.52, 2.77 |
| Smartphone use time | 1.21 | 0.98, 1.49 |
| Smartphone dependence | 1.00 | 0.96, 1.04 |
| Anxiety | 1.09 | 0.92, 1.29 |
| Depression | 0.98 | 0.87, 1.12 |
| Physical activity - Sedentary | 2.39 | 0.83, 6.86 |
| Physical activity - Insufficiently active | 2.46 | 1.05, 5.75 |
| Physical activity - Very active | 0.51 | 0.17, 1.52 |
| Sleep quality | 1.77 | 1.18, 2.64 |
| Frequency of neck pain (model 2) | ||
| OR adjusted | 95 % CI | |
| Cervical flexion angle (CROM*), standing | 1.01 | 0.99, 1.03 |
| Age | 1.02 | 0.99, 1.04 |
| Sex (male) | 1.01 | 0.52, 1.96 |
| Smartphone use time | 1.06 | 0.94, 1.19 |
| Smartphone dependence | 1.00 | 0.97, 1.03 |
| Anxiety | 1.05 | 0.96, 1.16 |
| Depression | 0.98 | 0.91, 1.06 |
| Physical activity - Sedentary | 1.56 | 0.73, 3.31 |
| Physical activity - Insufficiently active | 1.18 | 0.67, 2.07 |
| Physical activity - Very active | 1.00 | 0.59, 1.69 |
| Sleep quality | 1.55 | 1.21, 2.00 |
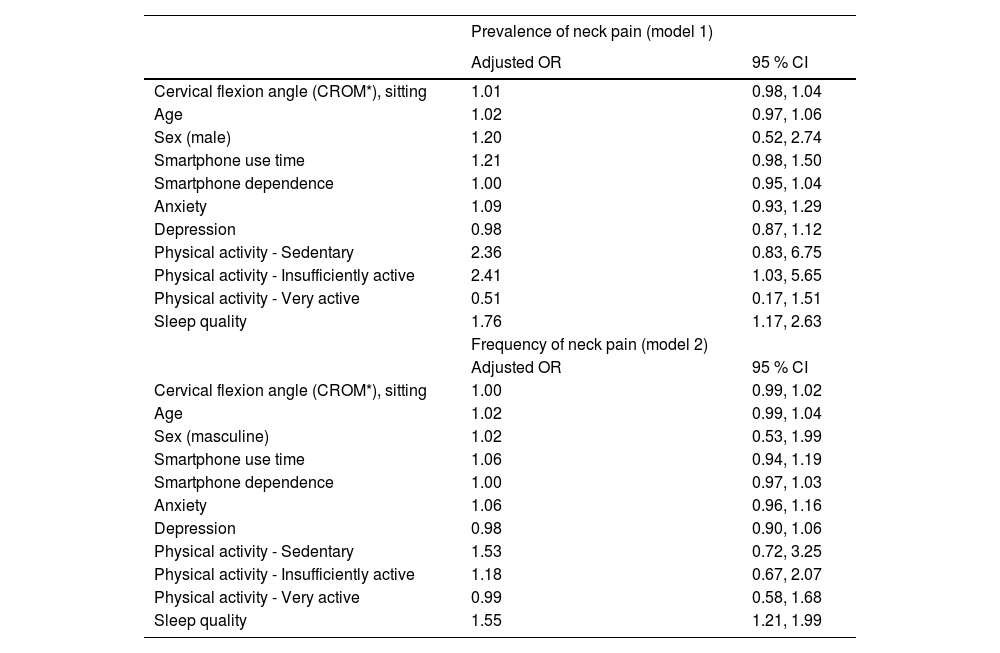
The same was observed with participants in a sitting posture while using a smartphone. Text neck did not increase the chance of NP (OR = 1.01; 95 % CI: 0.98, 1.04) or frequency of NP (OR = 1.00; 95 % CI: 0.99, 1.02) one year after baseline. Regarding the potential confounders, sleep quality increased the chance of NP (OR = 1.76; 95 % CI: 1.17, 2.63) and frequency of NP (OR = 1.55, 95 % CI: 1.21, 1.99). When compared with active participants, those who were insufficiently active had an increased chance of NP (OR = 2.41; 95 % CI: 1.03, 5.65), (Table 3).
Odds ratio (OR) for the association between text neck while sitting - assessed by cervical flexion angle – with prevalence of neck pain (model 1) and frequency of neck pain (model 2) considering potential confounders for each model.
| Prevalence of neck pain (model 1) | ||
|---|---|---|
| Adjusted OR | 95 % CI | |
| Cervical flexion angle (CROM*), sitting | 1.01 | 0.98, 1.04 |
| Age | 1.02 | 0.97, 1.06 |
| Sex (male) | 1.20 | 0.52, 2.74 |
| Smartphone use time | 1.21 | 0.98, 1.50 |
| Smartphone dependence | 1.00 | 0.95, 1.04 |
| Anxiety | 1.09 | 0.93, 1.29 |
| Depression | 0.98 | 0.87, 1.12 |
| Physical activity - Sedentary | 2.36 | 0.83, 6.75 |
| Physical activity - Insufficiently active | 2.41 | 1.03, 5.65 |
| Physical activity - Very active | 0.51 | 0.17, 1.51 |
| Sleep quality | 1.76 | 1.17, 2.63 |
| Frequency of neck pain (model 2) | ||
| Adjusted OR | 95 % CI | |
| Cervical flexion angle (CROM*), sitting | 1.00 | 0.99, 1.02 |
| Age | 1.02 | 0.99, 1.04 |
| Sex (masculine) | 1.02 | 0.53, 1.99 |
| Smartphone use time | 1.06 | 0.94, 1.19 |
| Smartphone dependence | 1.00 | 0.97, 1.03 |
| Anxiety | 1.06 | 0.96, 1.16 |
| Depression | 0.98 | 0.90, 1.06 |
| Physical activity - Sedentary | 1.53 | 0.72, 3.25 |
| Physical activity - Insufficiently active | 1.18 | 0.67, 2.07 |
| Physical activity - Very active | 0.99 | 0.58, 1.68 |
| Sleep quality | 1.55 | 1.21, 1.99 |
The present longitudinal study showed that text neck was not a risk factor for NP or frequency of NP. On the other hand, psychosocial factors such as level of physical activity and quality of sleep seem to be more relevant in NP.
These results corroborate the cross-sectional studies by Damasceno et al.23 who evaluated the self-perception of the posture of 150 young people aged 18 to 21, Bertozzi et al.14 who analyzed categories of pain and disability in 238 students aged 18 to 30, and Correia et al.13 who evaluated 582 volunteers aged 18 to 65 years measuring the angle of the cervical spine while using a smartphone in standing and sitting positions, as none of them found an association between text neck and NP.
A longitudinal study with 686 participants showed that neck posture at age 17 was not a risk factor for persistent NP at age 22 in men, while in women, more relaxed postures were a protective factor for NP.24 Pain is multifactorial and influenced by a complex interaction of biopsychosocial factors.25–27 Individuals who reported problems sleeping had an increased chance of having NP. Initial studies show that low-quality sleep can cause or increase the intensity of pain,28 decreasing the pain thresholds and tolerance levels29 and that it can be a double pathway, where pain also leads to poor sleep quality.30
Another important factor that increased the chance of developing NP was the level of physical activity, in which insufficiently active individuals are more susceptible to pain compared to physically active individuals. Physical inactivity seems to be a mediator of the relationship between chronic pain and mortality.31 While regular physical activity prevents hyperalgesia through the activation of opioids and serotonin, anti-inflammatory cytokines reduce the activity of nociceptors. Physically active individuals commonly have better mental health and psychological well-being, while inactive individuals are more likely to experience depression and anxiety,32–34 as well as an increase in the likelihood of NP in young people.10 Furthermore, in some manifestations of pain, there is no superiority between types of exercise, so, ideally these people should be encouraged to practice the exercise that brings them some pleasure to promote adherence.35
LimitationsSome strengths of the study are the longitudinal design with 12-month follow-up, along with the potential biopsychosocial confounding factors included in the analysis. The main limitation of this study was the failure to differentiate between acute and chronic stages of NP. Additionally, we used a single question regarding pain on the day of the one-year follow-up. We chose this question because it is the least influenced by memory and covers acute and chronic neck pain. Although our age range was 18 to 65 years, the average age was relatively young (27 years). It is also important to highlight that the monitoring period for the participants took place during the COVID-19 pandemic in 2020, possibly leaving people to be more sedentary. The question of whether participants start to adopt a better posture after experiencing neck pain (NP) was addressed with our longitudinal design. However, it remains unknown whether the neck posture participants adopted during the study task is significantly different from their habitual posture when texting on a smartphone.
This 12-month longitudinal study contributes to the existing literature on the topic by reinforcing that text neck is not a risk factor for NP. Other factors such as sleep quality and level of physical activity seem to be more relevant. These results challenge the belief that flexed neck posture during smartphone use leads to NP. This linear causal relationship reasoning based solely on injuries or structural changes to justify pain is outdated. Future studies should investigate the influence of smartphone use before sleep on neck pain, as well as whether text neck increases the risk of neck pain in older adults.
ConclusionCervical flexion posture during smartphone use was not a risk factor for NP or frequency of NP, but low sleep quality and insufficient levels of physical activity were.
None to declare.
This study was supported by the Fundação Carlos Chagas Filho de Apoio à Pesquisa do Estado do Rio de Janeiro (FAPERJ, No E-26/211.104/2021) and Coordenação de Aperfeiçoamento de Pessoal (CAPES, Finance Code 001; No 88881.708719/2022–01, and No 88887.708718/2022–00).