Promoting exercise-related behavior change in rehabilitation is a challenge. The lack of integration between rehabilitation program prescriptions, behavior change interventions, and behavioral change theories is profound. Using behavior change theories properly is crucial for better adherence and promoting positive outcomes. Therefore, it is essential to bring theories that support the understanding of exercise-related behavioral change to the attention of rehabilitation practitioners.
ObjectiveThis masterclass article aims to provide the theoretical background of theories and strategies for exercise behavior change within the physical therapy context based on acknowledged behavioral change theoretical models.
MethodsThis is a narrative review that examines six behavior theories; five of them well-established, and a new (and promising) theory that has exhibited the most favorable outcomes in rehabilitation settings. The development process for this masterclass included conversations between authors, reviewing behavior theories, summarizing and discussing the theories' concepts and strategies for physical therapy.
ResultsThe included theories were self-determination theory, social-cognitive theory, the transtheoretical model, the theory of planned behavior, the health belief model, and the unifying theory of physical activity. Each theory offers a unique perspective on exercise behavior change within rehabilitation, exploring constructs such as motivation, self-efficacy, stages of change, behavioral intention, perceived threat, and the core elements of physical activity expression.
ConclusionThese theoretical models provide a foundation for understanding and developing strategies for promoting exercise behavior change in rehabilitation. Knowing and using these theories is important for respecting the patient's individuality.
Several position statements and guidelines highlight the importance of promoting exercise-related behavior change as a significant rehabilitation goal.1–4 In addition, other guidelines have suggested a few strategies.4,5 Despite all these efforts, all the pieces in this puzzle have not fully fit, and promoting behavior changes remains a challenge.
Even though substantial progress has been made, there remains a lack of integration among rehabilitation program prescriptions, behavior change interventions, and behavioral change theories.6 However, changing health behaviors represents one of the critical challenges1 and opportunities health providers face in society.7 Using behavior change theories properly is linked to better adherence and health promotion. However, some health care delivery systems face challenges in regard to behavior change. One major problem is a lack of expertise in this comprehensive approach. As a result, health care practitioners do not always effectively help people with chronic conditions change their behaviors.7
In recent years, many researchers have failed to promote exercise-related behavior change in many rehabilitation contexts.4,8 Only a few tried to change exercise-related behavior with interventions based on the behavior change theories.8 Recently, a study on people with chronic obstructive pulmonary disease (COPD) showed that only a small number of behavior change techniques have been used in exercise interventions (and are poorly reported when used) and trials aiming to reduce sedentary time.8 Therefore, it is essential to explicitly bring theories of exercise-related behavioral change to the attention of rehabilitation practitioners. Using these theories, models, and interventions with empowerment and mastery in rehabilitation research and practice is critical to achieving behavior change. In addition, this knowledge can support best practices and ensure that health professionals use evidence-based strategies to help patients change their behaviors. After that, we may have a broader understanding of better adherence and long-term effectiveness in promoting lifestyle change, functioning, health, and wellness.
The present manuscript explores five well-established behavior change theories and a new (and promising) one to help illustrate the potential efficacy of exercise-related behavioral change practices in rehabilitation. The following theories were selected for their influence in promoting positive rehabilitation outcomes: self-determination theory, social-cognitive theory, the transtheoretical model, the theory of planned behavior, the health belief model, and the unifying theory of physical activity.
Thus, this review aims to provide the theoretical background of theories and strategies for exercise behavior change within the rehabilitation context based on acknowledged behavioral change theoretical models.
MethodsThe present paper is a narrative review concerning the scientific examination of behavior theories that provide theoretical explanations and strategies for exercise behavior change within rehabilitation programs. While we acknowledge a nonsystematic review method, this work supports the idea that scientific debates have explanatory and call-for-action virtues. It is essential to acknowledge some conditions and interests informed in this review. First, the behavioral change conception within the rehabilitation context was based on professionals' interest originating from discomfort with the rationalities of existing exercise/rehabilitation interventions in academia.9 Attempting to express and challenge these discomforts might require an understanding of the role of some existing theories and how they are applied.
Articulating an essay is an exploratory and creative process biased by the experience and worldview of the researchers. Acknowledging these aspects, an approximate delineation of the essay development included: (a) conversations between the authors about why humans move; (b) reviewing the literature of various behavior theories for the underlying causes of physical activity/exercise maintenance; and (c) summarizing and discussing theories, concepts, and strategies to be applied within the rehabilitation context. The selected references were expanded with a literature search incorporating findings from pertinent studies to elucidate the effectiveness of these strategies across various systematic review studies for various conditions/diseases. The search strategy and the summary of the manuscripts found are presented in Supplementary material online.
We refer to exercise behavior change to talk about an area of interest, exercise psychology, that includes physical activity behavior, exercise behavior, and rehabilitation behavior. Thus, authors should be judicious on using the appropriate term when explaining the outcomes of interests (e.g., an intervention aimed at increasing step counts involves physical activity behavior change).
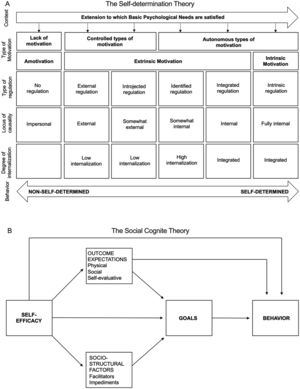
ResultsSelf-determination theoryPeople are centrally concerned with motivating themselves or others to act. Self-determination theory, introduced by Deci and Ryan,10 operates with four mini theories: basic psychological needs, cognitive assessment, causality orientations, and organismic integration. This theory explores motivation as a multifaceted concept based on three distinct qualities. These qualities, ranging from the least to the most self-determined, are amotivation, controlled motivation, and autonomous motivation. For self-determination theory, each motivation type has its regulations. Motivational regulations are the various mechanisms that reflect the quality of motivation toward a particular activity. Additionally, each regulation of the motivation continuum reflects reasons or perceived causes of action, known as the perceived locus of causality. It can range from impersonal, meaning that individuals do not see reasons behind their actions, to external (seen as external to or outside of one's control), and then to fully internal, indicating that individuals act from their own choices and volitions.10
Amotivation reflects a lack of intention (and motivation) and has no regulation (e.g., the patient does not see the point in exercising). The sense of obligation or the desire to achieve a goal drives controlled motivation. Researchers have further divided it into two forms of regulation. The first is external regulation, in which behavior is mainly motivated by the desire for rewards or to avoid punishment (e.g., the patient exercises because other people say they should). The second form, introjected regulation, occurs when individuals internalize their reasons for action, but their behavior is still controlled by external factors such as avoiding guilt or shame (e.g., the patient feels guilty when they do not exercise). Autonomous motivation is driven by pleasure, satisfaction, or the importance placed on an activity, and it has three forms of regulation. The first, identified regulation, occurs when behavior becomes valued, meaningful, and voluntarily engaged, although it still serves as a tool to achieve an objective (e.g., the patient values the benefits of exercise, and it is important to them). The second form, integrated regulation, is considered the most self-determined form of extrinsic motivation because it involves the full assimilation of regulations into the self-concept, including one's beliefs and personal needs (e.g., the patient considers exercise a fundamental part of who they are). The last is intrinsic regulation, which is the most self-determined form of behavior and reflects the drive to participate in an activity purely for enjoyment or satisfaction, without external or internal pressures (e.g., the patient finds exercise a pleasurable and fun activity). External, introjected, identified, and integrated regulations are considered extrinsic motivation, and intrinsic regulation is considered intrinsic motivation. According to self-determination theory, individuals can internalize behavioral regulation by fulfilling their psychological needs for autonomy, competence, and relatedness.11–13 Self-determination theory is summarized in Fig. 1A
A) Self-determination theory classifies motivation into a continuum of self-determination, ranging from lack of intention, to controlled motivation, to autonomous motivation. These motivational types are shaped by perceived regulations and the locus of causality, influencing behavior internalization. Fulfilling autonomy, competence, and relatedness needs leads to internalized behavioral regulation. Adapted from: Deci and Ryan, 1985.10 B) Social cognitive theory. Self-efficacy plays a crucial role, influencing behaviors, adaptation, and change. The arrows indicate that perceived efficacy influences human behavior both directly and indirectly, through affecting other key types of determinants. Adapted from: Bandura, 2017.66
This theory emphasizes a set of behaviors and skills that endow individuals with the ability to be causal agents concerning their futures, that is, to exhibit intentional behaviors.14 The theory is a way of understanding human motivation and personality. It focuses on how people naturally grow and regulate their behaviors. It uses an organismic perspective, considering how people naturally develop and change over time.15 Interventions theoretically based on self-determination theory can generate long-term behavioral changes, such as increased physical activity.16
Self-determination theory has recently attracted special attention, generating evidence across numerous domains. For example, a meta-analysis of self-determination theory techniques to promote motivation for health behavior change has been published recently.16,17 It showed that interventions grounded within this theory positively affect its constructs such as perceptions of autonomy support and satisfaction, competence satisfaction, motivation,16,17 health behaviors, and physical and psychological health.17 Some examples of the broader strategies of self-determination theory are providing choice, acknowledging the participant's perspective, providing a meaningful rationale, using noncontrolling language, having an intrinsic goal orientation, implementing behavioral practice/rehearsal, developing plans appropriate to one's ability, emphasizing responsibility, exploring reasons, providing optimal challenges, providing informational feedback, providing support and encouragement, identifying barriers, experiencing involvement, encouraging social support seeking, and cooperating with groups.16,18,19
Social cognitive theorySocial cognitive theory establishes that learning occurs through observation; thus, social learning occurs as a dynamic and reciprocal interaction between the individual's mind and the surrounding environment.20 Individuals acquire and maintain behaviors in unique ways, considering their past experiences and the social environment where behavior is to be performed, all of which will be considered when deciding whether action will be taken.21 Social cognitive theory has six constructs: reciprocal determinism (interaction between person, environment, and behavior), behavioral capability (ability to perform a behavior through knowledge), observational learning (to witness behavior and reproduce it), reinforcements (internal and external responses to behavior), expectations (anticipated consequences of behavior), and self-efficacy (level of confidence in the ability to perform a behavior successfully).21
Self-efficacy plays an important role in rehabilitation. It is a person's belief in their ability to successfully perform behaviors, manage their functioning, and control events that impact their life. It is a path to personal growth, adaptation, and change.22,23 Low self-efficacy is reflected by low confidence, reluctance to exercise appropriately, low medication compliance, and problems managing symptoms.23,24 For people with chronic conditions, interventions that support self‐management improve patient self‐efficacy. Boosting self‐efficacy could be a way to increase treatment adherence and outcomes in addition to reducing costs. However, it cannot succeed unless proper strategies are implemented to break barriers such as health literacy, access, support, and sustainable behaviors.25 The role of self-efficacy and other social cognitive factors regulating behavior, according to social cognitive theory, is illustrated in Fig. 1B. It illustrates how pathways involving perceived self-efficacy and other essential factors from social cognitive theory regulate behavior. Key factors, particularly self-efficacy, directly influence human behavior and impact other significant determinants.
Self-efficacy and other markers of increased vulnerability to suboptimal self-management in people with chronic diseases, such as unemployment or disability to work and multimorbidity, must be considered.26 Additionally, promoting self‐efficacy can improve the outcomes and quality of life for patients with chronic diseases.27 Two recent meta-analyses have described the relationship between self-efficacy and several important outcomes for patients with chronic respiratory diseases.28,29 In COPD, self-efficacy is moderately associated with functional exercise capacity and weakly to moderately related to physical activity, with the strength of the correlation coefficients varying according to the type of self-efficacy. The strongest correlation is between self-efficacy for exercise and functional exercise.28 In addition, a moderate positive relationship exists between self-efficacy and health-related quality of life, especially between exercise and COPD symptom-related self-efficacy.29
In the broader context of promoting physical activity among older people, a systematic review30 identified three essential behavior change techniques that have shown significant effects on increasing physical activity levels in community settings: identifying and solving barriers, providing rewards for successful behavior, and demonstrating the behavior. In addition, behavior change techniques such as "provide normative information about others' behavior," "provide information on where and when to perform a behavior," and "plan social support/social change" were significantly associated with smaller physical activity behavior change effect sizes.30 Two other systematic reviews assessed which behavior change techniques were related to changes in self-efficacy for physical activity31,32 and physical activity behavior32 in adult populations. Several techniques were effective, including receiving information about social and environmental consequences, committing to a goal, and understanding the emotional consequences of behavior.31 Other effective techniques include giving general information about behavior consequences, creating a plan of action, reinforcing progress, giving instructions, facilitating social comparison, and managing time.32 In adults who are obese, the techniques with larger effect sizes associated with positive changes in physical activity were "teach to use prompts/cues," "prompt practice," or "prompt rewards contingent on effort or progress toward behavior." For patients with heart failure, integrating the strategies of "successful performance/mastery experience," "vicarious experience," "verbal persuasion," and physiologic and affective states" can have positive effects on confidence and the ability to initiate exercise and recover from heart failure symptoms.33
Transtheoretical modelThe transtheoretical model, also called the stages of change model, was developed by Prochaska and Velicer34 to integrate constructs from leading theories of psychotherapy and behavior change.34 In the transtheoretical model, behavior change is conceptualized as a process that unfolds over time through the stages of change, with this being the model's central construct by which individuals progress and regress. There are 5 stages of behavior change (Fig. 2A): precontemplation (no intention of taking action in the next 6 months), contemplation (thinking about changing within the next 6 months), preparation (intending to take action in the next month), action (having made specific modifications within the past 6 months), and maintenance (taking action for 6 months to 5 years).35 Different intervention strategies are most effective for each stage of change at moving the person to the next stage and subsequently through the model. The model also includes 10 processes of change that people use to progress through the stages: consciousness-raising, dramatic relief, self- and environmental reevaluation, self- and social liberation, counterconditioning, stimulus control, contingency management, and helping relationships.34 In addition, the beliefs that people have about the advantages and disadvantages of making a behavior change (decisional balance), the ability to perform the behavior in specific situations (self-efficacy), and the intensity of urges to engage in a particular behavior when amid difficult situations (temptation) are other constructs of this model.34
A) The transtheoretical model and its 5 stages of behavior change. Each stage represents a distinct phase through which individuals progress over time. The model also incorporates 10 processes of change and additional constructs, including decisional balance, self-efficacy, and temptation. Adapted from Karloh et al.67 B) The theory of planned behavior diagram focuses on behavioral intention as the key driver of behavior. It incorporates 3 constructs and 3 components that influence intention, which, in turn, affect behavior. Adapted from: https://people.umass.edu/aizen/tpb.diag.htm.
The first study using the transtheoretical model investigated smoking cessation; however, over time, it has been extended to healthy lifestyle promotion studies, including physical activity.36 A previous systematic review37 showed that seven studies involving people with diabetes, breast cancer, and the general population in workplace interventions found significant short-term improvements in physical activity, but only one yielded important long-term findings. Mastellos et al.38 included only three studies that used the transtheoretical model for dietary and exercise modification in weight loss management for adults who were overweight or obese in their systematic review. These studies showed increased exercise duration and frequency, reduced dietary fat intake, and increased fruit and vegetable consumption. However, the small number of studies and their low quality did not allow for a robust conclusion to be drawn.38 A recent systematic review39 aimed to evaluate the effects of behavior change theory-based physical activity interventions for women with breast cancer. It included only five studies that used the transtheoretical model exclusively, and the overall analysis (with studies that used other theories) exhibited small to medium improvements in physical activity and health-related outcomes. However, not all theoretical constructs were linked to the interventions. For example, none of the included trials reported on the involvement of social support, despite this factor being a concept within the transtheoretical model.39 Authors from different systematic reviews36,37 revealed that few studies of physical activity interventions have been developed using all the transtheoretical model dimensions. They emphasized that the transtheoretical model is a model, and the stages of change are only its organizational constructs; thus, they should be combined with the other transtheoretical model constructs to assume explanatory power and increase the chances of success.
Theory of planned behaviorThe theory of planned behavior presupposes that behavioral intention is the primary determinant of behavior, barring any environmental constraints and deficiency in skills.40 When Ajzen41 developed this theory, he hypothesized that human behavior is guided by three constructs: behavioral, normative, and control beliefs.41 The first construct links the behavior of interest to expected outcomes and experiences and is expected to produce a favorable or unfavorable attitude toward the behavior. The second reflects the perceived pressure to engage in a particular behavior exerted by significant and reference individuals or groups. The third construct is the presence of factors that may facilitate or hinder the performance of the behavior and give rise to perceived behavioral control or self-efficacy. The perception of behavioral control moderates the impact of attitudes toward the behavior (whether it is viewed as positive or negative) and subjective norms on one's intention to engage in the behavior, including perceptions of whether others believe the behavior is appropriate. The more favorable the attitude and subjective norm and the greater the perceived control are, the stronger the person's intention to perform the behavior in question. Therefore, people are expected to carry out their intentions when the opportunity arises if they have sufficient control over their behaviors. Thus, behavioral intention is assumed to be the immediate antecedent of behavior. Furthermore, as behavioral control is perceived, it can expand the extent to which a person has the skills, resources, and other prerequisites needed to perform the behavior (actual behavioral control) and contribute to predicting behavior.41,42 This theory is schematized in Fig. 2B.
A systematic review suggested that theory-based interventions (including the theory of planned behavior) effectively promote physical activity.43 Ajzen44 recommends that interventions targeting behavior change using the theory of planned behavior should be designed and directed at one or more of its determinants: attitudes, subjective norms, or perceived behavioral control. He argues that these factors should produce changes in behavioral intentions under appropriate circumstances and with adequate control over the behavior.43 Senkowski et al.40 suggest that theory of planned behavior interventions should consider cognitive and affective beliefs and outcome expectations related to physical activity when targeting attitudes in the elderly population. In addition, positive and supportive interactions with significant others and health care providers could be emphasized rather than focusing on health consequences. The most frequently used behavior change techniques for physical activity interventions in theory of planned behavior studies for older adults were goal setting, action planning, and credible source. Goal setting and action planning were used in most studies and delivered through booklets, online guidance, or group discussions. Credible source involves a presentation of verbal or visual communication in favor of or against a behavior by someone regarded as credible to the target population, such as a health professional, minister, personal coach, or celebrity.40
Evidence shows that implicit attitudes toward physical activity were significantly correlated with physical activity behavior, with a small effect size in the general population and persons submitted to rehabilitation programs, such as patients with respiratory conditions and survivors of endometrial cancer.45 In pulmonary rehabilitation, patients who clinically improved their exercise functional capacity at the end of the program were characterized by having higher implicit attitudes at baseline than other patients.46 In addition, perceived behavioral control over physical activity and sedentary behavior increased during rehabilitation, whereas explicit attitudes did not change. Social norms for sedentary behavior significantly increased, but those for physical activity did not, with intentions toward physical activity but not those toward sedentary behavior higher at the end of pulmonary rehabilitation. Implicit attitudes came to more strongly favor physical activity over sedentary behavior.47 Positive changes in self-reported physical activity and the components of the theory of planned behavior were observed in the intervention group of a randomized controlled trial that aimed to increase physical activity using an educational program based on the theory of planned behavior in military members who were overweight or obese.48
Health belief modelThe health belief model was developed in the 1950s to investigate why people fail to undertake preventive health measures.49,50 The health belief model addresses the individual's perceptions of the threat posed by a health problem (susceptibility, severity), the benefits of avoiding the threat, and the factors that influence the decision to act (barriers, cues to action, and self-efficacy). The health belief model addresses 6 constructs influencing people's decisions about preventing, tracking, and controlling disease. The theory establishes that people are ready to act when they have met the following conditions: first, believing they are susceptible to a condition (perceived susceptibility); second, believing that the behavior has serious consequences (perceived severity); third, believing the action will reduce their vulnerability to the condition or its severity (perceived benefits); fourth, believing that the benefits outweigh the costs of action (perceived barriers); fifth, being exposed to factors that lead to action (clue to action); and last, being confident in their ability to act successfully.51 Practitioners should base their efforts on understanding the target population's susceptibility to the health problem, whether they believe it to be serious, and whether they believe action can reduce the threat at an acceptable cost when applying the health belief model.51 This theory is summarized in Fig. 3A.
A) The health belief model proposes that individuals' perceptions regarding health issues, their assessment of the advantages and obstacles linked to acting, and their confidence in their ability to act collectively elucidate their involvement in health-enhancing actions. Adapted from: Rosenstock, Strecher and Becker.50 B) The unifying theory of physical activity offers a holistic view of physical activity, emphasizing embodied practice beyond health concerns. It posits human urges as central to physical activity expression. Supportive conditions for these urges, along with contextual influences, drive meaningful and fulfilling physical activity engagement. Adapted from: Matias and Piggin, 2022.61
The health belief model has been used for several health approaches, including self-care education and to predict and explain physical activity.52 This theory has been applied in several ways related to increasing physical activity, including the identification of determinants of physical activity at various ages and the cultural origins and factors associated with physical activity among middle-aged women53 and older adults.54 In addition, recent systematic reviews explored using the health belief model to predict health behavior, including vaccination or preventive behavior against COVID-1955–57 and cancer screening.58 It is hypothesized that people with higher perceived susceptibility, higher perceived benefits, and higher self-efficacy can be placed in lower-barrier groups more likely to engage in behaviors that promote health.55 The model has also been used to develop successful health communication interventions by framing messages in terms of the health belief model variables to change health behaviors,57 including adopting preventive behaviors in patients with a primary diagnosis of an acute coronary syndrome.59
Furthermore, one study has used the health belief model to assess the health beliefs of adults with multiple sclerosis and the relationship between health beliefs and physical activity behavior.60 The authors concluded that individuals with multiple sclerosis believe they can benefit from physical activity and remain healthy even in the context of their disease. However, they also acknowledge that their disability levels limit their exercise capabilities. Given that self-efficacy and perceived activity benefits are essential determinants of physical activity, health promotion efforts should be directed at these modifiable factors.60
Unifying theory of physical activity (UTPA)The unifying theory of physical activity is an emerging model that promotes a perspective of physical activity that moves beyond health-dominated narratives and toward a holistic view of physical activity as an embodied practice. It assumes that movement is inherent in human life.61 Physical activity is a function of organism-environment interactions. Thus, movement provides bodily existence (physical activity understanding), and the human body is the primary site of becoming conscious. The unifying theory of physical activity argues that human urges (the 4 physical activity urges are – to feel, to explore, to transform, and to connect) are at the core of the expression of physical activity. Conditions that support those urges are the basis for informing ongoing physical activity and its quality and sustaining behavior with a powerful sense of meaning. Supporting physical activity urges could grow/animate basic psychological needs and essential motivations. The unifying theory of physical activity model recognizes contextual elements (the social, political, and situated quality of physical activity) influencing physical activity urges and subsequent expression. Additionally, the theory argues that every expression of physical activity has three features (potential, distinct, and integrated) that should be considered to guarantee human harmony when expressing physical activity.61 The unifying theory of physical activity is summarized in Fig. 3B.
The unifying theory of physical activity presents a framework for understanding human movement and physical activity that focuses on the fundamental principles behind why people are active rather than focusing on only health-related goals. According to the unifying theory of physical activity, physical activity can help people become more aware of their movements and purposefully act in the world, leading to personal fulfillment, utilizing one's full potential, cultural interaction, and integrating emotions and ideas. Rather than just burning calories, physical activity can provide meaningful experiences that fulfill basic human needs. However, supportive conditions are necessary for this human aptitude to thrive.61
The urge to feel leads individuals to seek sensory experiences connected to their values, desires, and memories. The unifying theory of physical activity highlights the importance of integrating movement and emotions within physical activity. This theory views physical activity as a feeling-based experience and stresses the importance of acknowledging the range of emotions that can accompany it. While behavior can be intrinsically rewarding and bring happiness and satisfaction, it can also involve negative emotions such as suffering, fear, and anguish.62 For physical activity to be sustained, individuals must experience immediate and emotional outcomes.61,63
The urge to explore reflects the human desire to explore and venture into the unknown. This desire is rooted in the idea that exploration is a crucial part of human existence,62 with personal growth occurring on the boundaries of our corporal existence. Considering exploration as a patient's urge is particularly important for physical therapy. For instance, physical therapists deal with spatiality.64 To support exploration, they should give patients space, not focus on deficits, and help patients understand the social, political, and cultural boundaries that constrain their actions.
The urge to transform is not based on solely the natural physical transformations that occur throughout an individual's life but rather arises from the interplay between physical activity and creation. Allowing the individual to participate, create, and be autonomous. Evidence from a meta-analysis shows that interventions based on supporting basic human needs, including autonomy support strategies, can foster high-quality motivation and positive changes in health behaviors.16,17
The urge to connect is rooted in the human need for belonging and spirituality. Engaging in physical activity enables an individual to experience a holistic interaction between the physical, mental, emotional, and spiritual aspects of living, leading to deeper awareness and integration. This connection can occur internally with oneself, externally with others, and even with the material and spiritual world.61
It is suggested that individuals are motivated to act/move and enhance their consciousness about the world when these urges are fulfilled. Animating urges is the basis for fulfilling basic psychological needs and essential motivations. This high quality of motivation allows engagement in activities, improved performance, and creativity; then, the individual acquires an understanding of physical activity. Health-related aspects are the most distal of the individual's desires.
The unifying theory of physical activity is promising in managing patients in rehabilitation settings.6 By recognizing the urges that underlie physical activity, health professionals can gain a pedagogical understanding of what aspects of social life should be emphasized to promote physical activity and what should be avoided. Health professionals should ask themselves a series of questions regarding their prescribed treatments. For instance, whether their intervention allows patients to act authentically and explore various emotions or whether it encourages patients to challenge themselves and discover new things in the world. Another example is whether the intervention provides opportunities for transformation, creation, and learning. Additionally, health professionals should consider whether their intervention enables patients to connect with others, the environment, and culture.6 Answering these questions can help health professionals design interventions that promote physical activity while considering the patient's social and personal needs.61
DiscussionThis review aims to enhance the knowledge of promoting effective exercise-related behavioral change among rehabilitation specialists. The insights presented will aid professionals in effectively guiding their patients toward successful outcomes. Unfortunately, this knowledge has been poorly addressed in most of Brazil's graduation and postgraduation programs, and rehabilitation professionals tend to believe that the behavior change process will occur in a nonintentional manner.
Although we acknowledge significant advancements, there is still a long road ahead, as illustrated in the field of pulmonary rehabilitation. While recent work on modern pulmonary rehabilitation4 has contributed to this area, we note that the components identified through their Delphi process incorporate only two behavior change techniques: goal setting and physical activity counseling. Although the delivery methods of 'shared decision-making between patients and health care professionals' and 'regular contact between health care professionals and patients' were also mentioned, the current behavior change literature indicates that these strategies alone are unlikely to promote behavioral change successfully. 'Shared decision-making' represents only one strategy among many that can be utilized to enhance behavioral-related variables. Other strategies include recognizing the participant's perspective, providing justification, adjusting language style, orienting with intrinsic objectives, providing structural facilitation, emphasizing responsibility, and exploring reasons for behavior.
This manuscript aims to evoke a critical discussion in the rehabilitation community. The one-size-fits-all approach to promoting behavioral change across all populations is impractical. Instead, effective approaches might need to include the varying motivational, self-efficacy, stages of change, and physical activity urge profiles of individuals based on their personal input. Background contextual affordances are strongly related to patients' learning experiences. In addition, providing a positive learning experience through a supportive environment will likely push patients toward exercise-related behavioral changes. In addition, behavioral-related variable assessments should consider the person's needs and adapt rehabilitation programs.65 Finally, behavior change techniques must be prescribed intentionally and objectively, like any other exercise-related intervention and be experienced together with exercises.
The process of promoting effective exercise-related behavioral change is a considerable challenge, and three points need to be made. First, a theory provides a partial understanding of a complex reality. Second, promoting behavior change toward positive outcomes requires a partial understanding of multiple theories. Third, health care professionals must be judicious in studying and applying human behavior theories.
Behavioral change is a complex and multifaceted process that involves many individual and environmental factors. Rehabilitation practitioners may need to understand multiple theories and strategies to guide their interventions to achieve the best possible outcomes for their patients. Table 1 presents a summary of concepts from each theory discussed in the present essay.
Behavioral change theories and their essential takeaways for rehabilitation practitioners.
| Theory | Important Points to Remember |
|---|---|
| Self-Determination Theory10–13 |
|
| Social-Cognitive Theory20,21 |
|
| Transtheoretical Model34,35 |
|
| Theory of Planned Behavior40,41 |
|
| Health Belief Model49,50 |
|
| Unifying Theory of Physical Activity61 |
|
While this essay presents arguments that encourage action and clarify scientific debates, it is important to note that it is not a systematic review and may be subject to bias based on the experiences and perspectives of the researchers. Nevertheless, there is a pressing need for papers that synthesize behavior change theories and disseminate this information to inspire further research and its application in clinical settings.
ConclusionsSelf-determination theory explores how supporting basic psychological needs can foster high-quality forms of motivation. Social-cognitive theory stresses self-efficacy, which is critical in influencing health behavior. The transtheoretical model offers an approach in which behavior change occurs through the stages of change. The theory of planned behavior considers behavioral intention a primary determinant of behavior. The health belief model evokes the individual's perceptions of the threat posed by a health problem, the benefits of avoiding the threat, and the factors influencing the decision to act. The unifying theory of physical activity is very recent and the first theory developed specifically for the physical activity area; it assumes that there are 4 core elements of the expression of physical activity. To achieve behavioral change in rehabilitation, it is crucial for practitioners to learn and implement theories and strategies within interventions related to exercise-related behavioral change.
AcknowledgmentsJMO is supported by a PhD grant from Coordenação de Aperfeiçoamento de Pessoal de Nível Superior e Programa de Suporte à Pós-Graduação de Instituições de Ensino Particulares - CAPES/PROSUP, Brazil (grant number - 88887.634756/2021-00). FFL is supported by Post-Doctoral fellowship from Fundação de Amparo à Pesquisa do Estado de São Paulo – FAPESP, Brazil (grant number 2021/04198-6). DHAP is supported by a PhD grant from Fundação de Amparo à Pesquisa do Estado de São Paulo – FAPESP, Brazil (grant number 2021/03745-3). KCF is supported by a personal grant from Fundação Nacional do Desenvolvimento do Ensino Superior Particular – FUNADESP, Brazil (grant number 5301164). CRFC is supported by Conselho Nacional de Pesquisa e TEcnologia (CNPq) grant 312.279/2018-3 and Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) grant 2018/17788-3.