The six-minute walk test (6MWT) is a simple, low cost, reliable, and valid method for evaluating the functional capacity of cardiac patients. However, its early use and safety following acute myocardial infarction (AMI) is recent and has been little investigated.
ObjectiveTo evaluate and to compare the safety and the cardiac behavior of early performance of the 6MWT in patients following uncomplicated AMI up to 4 days or more than 4 days after the event.
MethodsFollowing discharge from the Coronary Care Unit, 152 stable asymptomatic patients diagnosed with uncomplicated AMI performed the 6MWT. During the test, in addition to the distance walked, heart rate (HR), blood pressure (BP), and adverse events were also recorded. Electrocardiography was recorded using a Holter monitor in 105 patients. Patients were allocated considering two groups according to the number of days since AMI: Up to 4 Days Group and After 4 Days Group.
ResultsAll patients completed the 6MWT, 66 in the Up to 4 Days Group and 86 in the After 4 Days Group. The walking distance was similar in both groups (85% of the predicted value), as well as the physiological responses (increase in systolic BP and HR), reaching 63% (median) of maximum HR. Only 3.9% of patients had major complications (angina, drop in BP, or ventricular tachycardia), with no difference between the groups. None of the complications regarded as severe led to truly significant complications or death.
ConclusionThe 6MWT was proven to be safe and feasible for early functional evaluation following uncomplicated AMI.
The six-minute walk test (6MWT) is a simple, low-cost, valid and reliable method for evaluating functional capacity.1,2 This test is widely used in the clinical management of patients suffering from chronic lung3,4 and heart5,6 diseases, but its use in acute myocardial infarction (AMI) prior to hospital discharge is still recent and has been little investigated.7 A possible reason would be that the main guidelines for the 6MWT2 do not recommend its performance within 30 days of an AMI event. There is no evidence to support restricting the use of the 6MWT after a recent AMI.8
Early exercise testing after AMI can be used to assess functional capacity and the ability to perform tasks at home and at work, to evaluate the efficacy of medical therapy, and to assess the risk of a subsequent cardiac event.8 It is also important to initiate cardiac rehabilitation programs early, which is associated with decreased mortality9,10 and improved quality of life.9 The 6MWT may be a safe and viable option for the early evaluation of functional capacity following AMI,11 as it is a self-regulated effort test that can reflect the level of activities of daily living.1
The improvement in treatment strategies for AMI is reflected by hospitalization time and patients without complications are often discharged in less than 5 days,12 a fact that may hamper exercise testing before discharge. However, according to the guidelines of the American College of Cardiology/American Heart Association (ACC/AHA),8,13 submaximal exercise tests can be performed 3–5 days after AMI in patients without complications. Despite this, limited data is available on the safety of early exercise testing after AMI8 to support the performance of exercise testing before discharge.
Therefore, the objective of this study was to evaluate the safety of early performance of the 6MWT in patients following uncomplicated AMI from the moment of discharge from the Coronary Care Unit and to compare cardiac behavior between patients who performed the test up to 4 days or more than 4 days after the event. We hypothesized that the percentage of severe complications (i.e., angina, drop in blood pressure, and arrhythmias14 as identified by Holter) during the test would be less than 2% and that they would not be influenced by the time since AMI.
MethodsThe study was approved by the Research Ethics Committee of Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil (approval no. ETIC 0515.0.203.000-10) and developed at the University Hospital of UFMG from March 2011 to April 2013.
Possible candidates were identified among patients admitted to the Coronary Care Unit with a diagnosis of uncomplicated AMI (Killip class I or II),15 with or without ST-segment elevation (STE AMI or non-STE AMI) regardless of the reperfusion therapy – conservative, thrombolysis, percutaneous coronary intervention, or waiting for coronary artery bypass grafting. Different physicians using the same Coronary Care Unit protocol carried out the diagnosis. Furthermore, patients were required to meet the following inclusion criteria: age equal to or greater than 18 years, clinical and hemodynamic condition enabling discharge from the Coronary Care Unit and approval of the medical staff. The study did not include patients whose AMI event had taken place one week prior to the study or more, candidates with persistent arrhythmias (identified daily by electrocardiography), previous conditions associated with exercise intolerance (like pulmonary or peripheral arterial disease), signs and/or symptoms of angina at rest, unstable blood pressure levels, signs of active infection, or individuals/patients who presented changes that affected ambulatory ability. Killip class II patients with third heart sound and with extensive pulmonary crackles were also excluded.
Patients who met the research criteria were identified within 24h of discharge from the Coronary Care Unit (even if they stayed in Coronary Care Unit waiting for a room) by means of medical record analysis, clinical evaluation, and discussion with the medical staff. When all of the criteria were met, the selected patient received clarification regarding the study and its objectives, risks, and benefits. Patients were then provided with an informed consent form and invited to participate in the study. At this time, depending on the number of days since AMI, patients were allocated into two groups: Up to 4 Days Group or After 4 Days Group. This cut-off point (4 days) was based on the time proposed by ACC/AHA Guidelines8,13 for conducting submaximal exercise tests after AMI.
Six-minute walk testThe 6MWT was conducted following the guidelines proposed by the American Thoracic Society (ATS)2 in a 30-m hallway adjacent to the Coronary Care Unit, marked by cones, and at a time with less circulation of people (“a real life condition”). The test was supervised by a physical therapist and the medical staff of the unit could be called if necessary. Heart rate (HR), blood pressure (BP), saturation of peripheral oxygen (SpO2), and perceived exertion were assessed before and after the test (at the end and after five minutes), by means of the cardio frequency meter (Polar®, FS2c, Finland), auscultatory method, wrist oximeter (Mindray®, PM50, China) and the modified Borg Scale, respectively. HR and SpO2 were also monitored during the test performance. Signs and symptoms of exertional intolerance (chest pain, intolerable dyspnea, leg cramps, staggering, diaphoresis, and pale or ashen appearance) and elevated HR (identified by the cardio frequency meter) higher than 85%HRmax in relation to the estimated HR for age (HRmax=220–age), were used as criteria to interrupt the test,15 even in patients using beta-blockers. In this case, patients were immediately evaluated by medical staff, and if necessary additional tests and medication were provided. In this case, patients would be excluded. A Holter monitor was used to record cardiac rhythm during all 6MWTs.
Due to the learning effect,1,2 the test was performed twice and the longest distance walked was used for recording purposes. Although the ATS2 determines a one-hour interval between tests, the second test was initiated as soon as hemodynamic variables returned to resting values and the patient felt able to repeat the test.11 The objective of this conduct was to make 6MWT usage more dynamic and, therefore, more appropriate for the hospital context.
Patients were instructed as follows2: You will walk as fast as possible for 6min, walking back and forth around the cones. You will probably get out of breath or become exhausted, but try not to stop. You are permitted to slow down if necessary according to your perception. You are also permitted to stop, and to rest if necessary, but the 6min will be continuously recorded. Standardized phrases of encouragement will be spoken every minute to inform you how much time there is remaining until the end of the test, for example “You are doing well, you have 5min to go.”
The metabolic equivalent of task (MET) was calculated based on walking speed using the formulas16: (1) VO2 (mLkg−1min−1)=0.1×velocity (mmin−1)+3.5mLkg−1min−1 (tests without inclination) and (2) 1 MET=3.5mLkg−1min−1.
Holter monitoringA three-channel CardioLight® Holter monitor was used (Cardios, São Paulo, Brazil) to monitor patients recruited between April 2012 and April 2013. Following Holter placement, the patient was asked to remain at rest for 10min in bed for trace recording. Afterwards, the patient was led to the hallway, where the 6MWT was carried out.
The Holter records were subsequently evaluated to identify arrhythmias (including extrasystoles), supraventricular (SVT) and ventricular tachycardia (VT) and/or atrioventricular blocks (AVBs), and transient ST-segment changes during the 6MWT, taking the at-rest moment and the routine morning electrocardiogram as reference. A single cardiologist, being unaware of when patients had experienced AMI, analyzed traces. At the end of the study, another independent cardiologist reviewed traces whose changes suggested ischemia.
SafetyIn order to evaluate the safety of the 6MWT, the following factors were analyzed and presented descriptively: HR behavior, BP, SpO2, subjective perceived exertion (SPE), signs and symptoms of exercise intolerance, and Holter recordings. The safety of the early performance of the 6MWT following AMI was also assessed considering the frequency of complications.
Expected complications were divided into: clinical, e.g., angina, dyspnea, and/or intense fatigue, nausea, profuse sweating, palpitations, dizziness, signs of diminished tissue perfusion (pallor, cyanosis, presyncope); hemodynamic, e.g., drop in BP (greater than 10mmHg),14 absence of a minimal increase in HR (less than 10bpm)14 and SpO2<85%; and electrocardiographic, e.g., emergence of severe arrhythmias14 during Holter monitoring (SVT, VT, AVBs, and transient ST-segment changes). Complications that could aggravate the patient's condition or require immediate action were considered as severe; namely, angina, signs of diminished tissue perfusion (pallor, cyanosis, presyncope), drop in BP, absence of a minimal increase in HR and emergence of severe arrhythmias during Holter monitoring (persistent SVT, VT, second and third-degree AVBs, and ST-segment elevation).
Statistical analysisAs similar previous studies were not identified at the beginning of this study, the sample was analyzed considering the occurrence of 2% severe complications as significant. For alpha and beta errors set at 5% and for the one-tailed test (referred to the percentage of events), the calculated sample comprised 149 patients. In order to detect 5% arrhythmias during Holter monitoring, considering the same conditions, the calculated sample consisted of 59 patients.
Data were stored in a database built using EpiData software version 3.0 (www.epidata.dk – EpiData Association, Denmark) and analyzed using SPSS software version 17.0 for Windows (SPSS Inc., Chicago, IL, USA), considering α=5% as statistically significant. Categorical variables were described using absolute numbers and proportions and continuous variables, such as mean and standard deviation or median and interquartile range, and were represented according to their distribution. When both groups were compared, univariate analysis was performed using the chi-square test, Fisher's exact test, Student's t-test, and the Mann–Whitney test when appropriate.
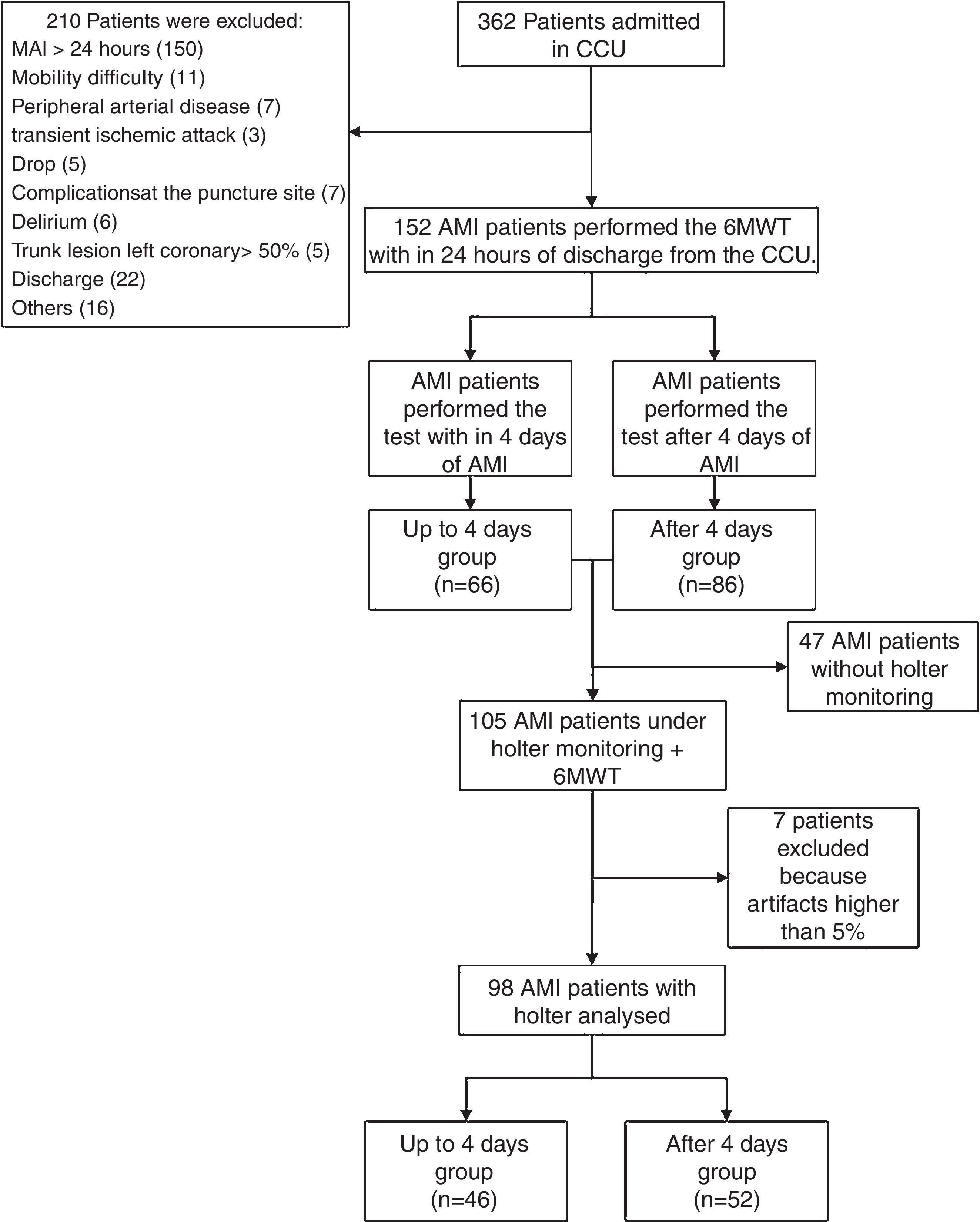
ResultsFig. 1 shows the flow chart with the number of participants.
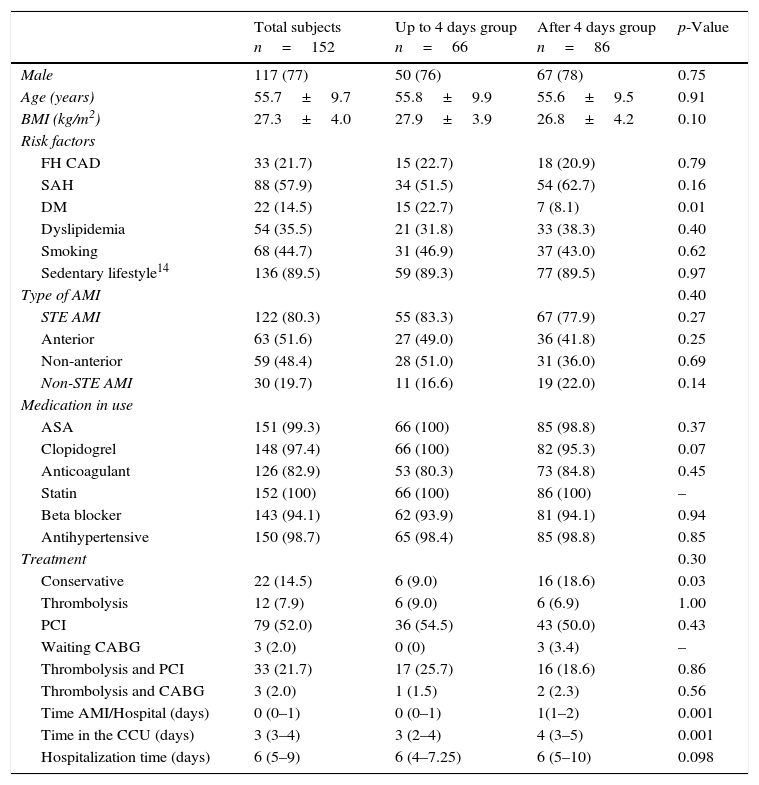
The sample (n=152) was comprised of mainly middle-aged, hypertensive, sedentary, and overweight men (Table 1). Most patients had experienced their first AMI (87.5%), predominantly an STE AMI (80.3%), and had up to 2 injured coronary arteries (73.7%). Only 1.3% of the patients did not undergo catheterization. Two patients had less than 50% left main coronary artery lesions. Most patients were classified as Killip class I upon admission and did not display signs of ventricular dysfunction throughout hospitalization, in accordance with the median ejection fraction of 54% (45–63%) measured by echocardiography. Diastolic function, however, was predominantly abnormal; 55.9% of the patients had abnormal relaxation patterns, 17.1% had pseudonormal relaxation patterns, and 0.7% displayed restrictive filling patterns.
Characteristics and clinical data of patients with acute myocardial infarction who performed the six-minute walk test.
| Total subjects n=152 | Up to 4 days group n=66 | After 4 days group n=86 | p-Value | |
|---|---|---|---|---|
| Male | 117 (77) | 50 (76) | 67 (78) | 0.75 |
| Age (years) | 55.7±9.7 | 55.8±9.9 | 55.6±9.5 | 0.91 |
| BMI (kg/m2) | 27.3±4.0 | 27.9±3.9 | 26.8±4.2 | 0.10 |
| Risk factors | ||||
| FH CAD | 33 (21.7) | 15 (22.7) | 18 (20.9) | 0.79 |
| SAH | 88 (57.9) | 34 (51.5) | 54 (62.7) | 0.16 |
| DM | 22 (14.5) | 15 (22.7) | 7 (8.1) | 0.01 |
| Dyslipidemia | 54 (35.5) | 21 (31.8) | 33 (38.3) | 0.40 |
| Smoking | 68 (44.7) | 31 (46.9) | 37 (43.0) | 0.62 |
| Sedentary lifestyle14 | 136 (89.5) | 59 (89.3) | 77 (89.5) | 0.97 |
| Type of AMI | 0.40 | |||
| STE AMI | 122 (80.3) | 55 (83.3) | 67 (77.9) | 0.27 |
| Anterior | 63 (51.6) | 27 (49.0) | 36 (41.8) | 0.25 |
| Non-anterior | 59 (48.4) | 28 (51.0) | 31 (36.0) | 0.69 |
| Non-STE AMI | 30 (19.7) | 11 (16.6) | 19 (22.0) | 0.14 |
| Medication in use | ||||
| ASA | 151 (99.3) | 66 (100) | 85 (98.8) | 0.37 |
| Clopidogrel | 148 (97.4) | 66 (100) | 82 (95.3) | 0.07 |
| Anticoagulant | 126 (82.9) | 53 (80.3) | 73 (84.8) | 0.45 |
| Statin | 152 (100) | 66 (100) | 86 (100) | – |
| Beta blocker | 143 (94.1) | 62 (93.9) | 81 (94.1) | 0.94 |
| Antihypertensive | 150 (98.7) | 65 (98.4) | 85 (98.8) | 0.85 |
| Treatment | 0.30 | |||
| Conservative | 22 (14.5) | 6 (9.0) | 16 (18.6) | 0.03 |
| Thrombolysis | 12 (7.9) | 6 (9.0) | 6 (6.9) | 1.00 |
| PCI | 79 (52.0) | 36 (54.5) | 43 (50.0) | 0.43 |
| Waiting CABG | 3 (2.0) | 0 (0) | 3 (3.4) | – |
| Thrombolysis and PCI | 33 (21.7) | 17 (25.7) | 16 (18.6) | 0.86 |
| Thrombolysis and CABG | 3 (2.0) | 1 (1.5) | 2 (2.3) | 0.56 |
| Time AMI/Hospital (days) | 0 (0–1) | 0 (0–1) | 1(1–2) | 0.001 |
| Time in the CCU (days) | 3 (3–4) | 3 (2–4) | 4 (3–5) | 0.001 |
| Hospitalization time (days) | 6 (5–9) | 6 (4–7.25) | 6 (5–10) | 0.098 |
Values presented as frequency (percentage), mean±standard deviation and/or median (interquartile range). AMI, acute myocardial infarction; ASA, acetyl salicylic acid; BMI, body mass index; CABG, coronary artery bypass grafting; CAD, coronary artery disease; CCU, Coronary Care Unit; DM, diabetes mellitus; FH, family history; non-STE AMI, AMI without ST-segment elevation; PCI, percutaneous coronary intervention; SAH, systemic arterial hypertension; STE AMI, AMI with ST-segment elevation; time AMI/Hospital, time in days between AMI and admission to the hospital.
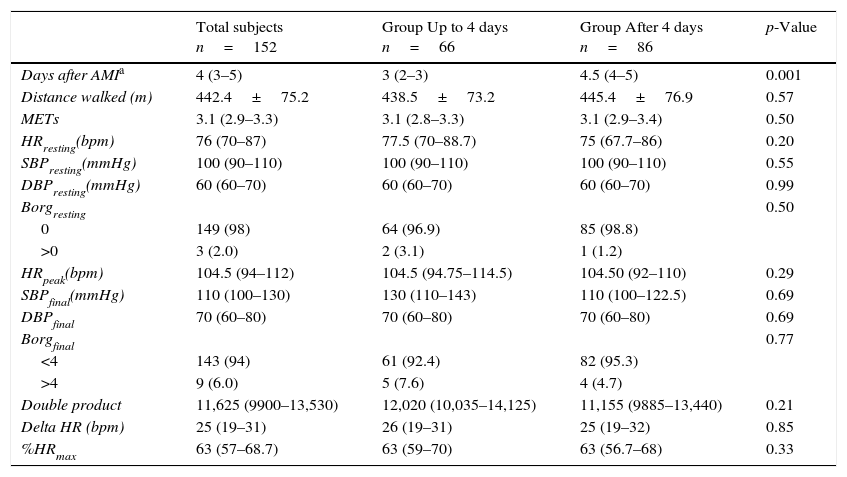
All patients completed the 6MWT. Patients walked a mean distance of 442.4m during the 6MWT, which corresponds to 85% of the expected distance (515.7m)17 (Table 2). During the test, BP and HR displayed physiological behavior, elevating during exertion and gradually returning to baseline values during rest. The elevation was mild, considering the entire patient sample. There was no statistical difference between groups for the variables assessed.
Clinical and hemodynamic behavior of patients with AMI subjected to the six-minute walk test.
| Total subjects n=152 | Group Up to 4 days n=66 | Group After 4 days n=86 | p-Value | |
|---|---|---|---|---|
| Days after AMIa | 4 (3–5) | 3 (2–3) | 4.5 (4–5) | 0.001 |
| Distance walked (m) | 442.4±75.2 | 438.5±73.2 | 445.4±76.9 | 0.57 |
| METs | 3.1 (2.9–3.3) | 3.1 (2.8–3.3) | 3.1 (2.9–3.4) | 0.50 |
| HRresting(bpm) | 76 (70–87) | 77.5 (70–88.7) | 75 (67.7–86) | 0.20 |
| SBPresting(mmHg) | 100 (90–110) | 100 (90–110) | 100 (90–110) | 0.55 |
| DBPresting(mmHg) | 60 (60–70) | 60 (60–70) | 60 (60–70) | 0.99 |
| Borgresting | 0.50 | |||
| 0 | 149 (98) | 64 (96.9) | 85 (98.8) | |
| >0 | 3 (2.0) | 2 (3.1) | 1 (1.2) | |
| HRpeak(bpm) | 104.5 (94–112) | 104.5 (94.75–114.5) | 104.50 (92–110) | 0.29 |
| SBPfinal(mmHg) | 110 (100–130) | 130 (110–143) | 110 (100–122.5) | 0.69 |
| DBPfinal | 70 (60–80) | 70 (60–80) | 70 (60–80) | 0.69 |
| Borgfinal | 0.77 | |||
| <4 | 143 (94) | 61 (92.4) | 82 (95.3) | |
| >4 | 9 (6.0) | 5 (7.6) | 4 (4.7) | |
| Double product | 11,625 (9900–13,530) | 12,020 (10,035–14,125) | 11,155 (9885–13,440) | 0.21 |
| Delta HR (bpm) | 25 (19–31) | 26 (19–31) | 25 (19–32) | 0.85 |
| %HRmax | 63 (57–68.7) | 63 (59–70) | 63 (56.7–68) | 0.33 |
Values presented as frequency (percentage), mean±standard deviation, and median (interquartile range). AMI, acute myocardial infarction; DBP, diastolic blood pressure; HR, heart rate; MET, metabolic equivalent of task; SBP, systolic blood pressure.
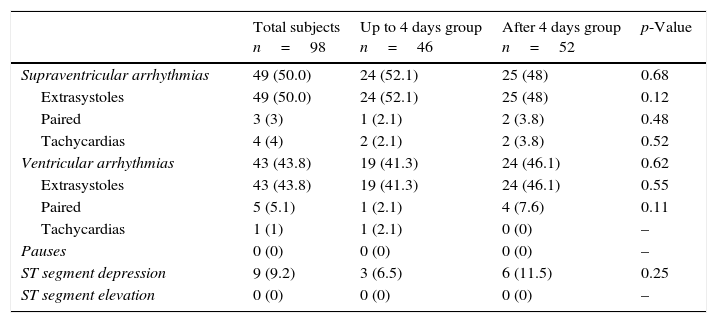
One hundred and five 6MWTs were performed under Holter monitoring. Among these, 7 Holter analyses were excluded due to the percentage of artifacts being higher than 5%. Therefore, 98 6MWTs were considered for analysis (Table 3).
Arrhythmias identified by Holter monitoring of patients with acute myocardial infarction during the six-minute walk test.
| Total subjects n=98 | Up to 4 days group n=46 | After 4 days group n=52 | p-Value | |
|---|---|---|---|---|
| Supraventricular arrhythmias | 49 (50.0) | 24 (52.1) | 25 (48) | 0.68 |
| Extrasystoles | 49 (50.0) | 24 (52.1) | 25 (48) | 0.12 |
| Paired | 3 (3) | 1 (2.1) | 2 (3.8) | 0.48 |
| Tachycardias | 4 (4) | 2 (2.1) | 2 (3.8) | 0.52 |
| Ventricular arrhythmias | 43 (43.8) | 19 (41.3) | 24 (46.1) | 0.62 |
| Extrasystoles | 43 (43.8) | 19 (41.3) | 24 (46.1) | 0.55 |
| Paired | 5 (5.1) | 1 (2.1) | 4 (7.6) | 0.11 |
| Tachycardias | 1 (1) | 1 (2.1) | 0 (0) | – |
| Pauses | 0 (0) | 0 (0) | 0 (0) | – |
| ST segment depression | 9 (9.2) | 3 (6.5) | 6 (11.5) | 0.25 |
| ST segment elevation | 0 (0) | 0 (0) | 0 (0) | – |
Values presented as number of patients (percentage).
Supraventricular arrhythmias, particularly extra systoles, were the prevalent finding in Holter monitor analyses, having been observed in 49 patients. Supraventricular tachycardia was rare and there were only 4 non-persistent cases, which occurred in 2 patients from each group (HR 138bpm: 3 beats, HR 179bpm: 3 beats, HR 148bpm: 3 beats, HR 125bpm: 4 beats). Ventricular arrhythmias were also prevalent, particularly extra systoles. Only one patient suffered from non-sustained ventricular tachycardia, belonging to the Up to 4 Days Group (HR 109bpm: 5 beats, the greatest; and HR 114bpm: 3 beats, the fastest). Transient ST-segment changes were observed in 9 patients. These arrhythmias were observed only during the 6MWT.
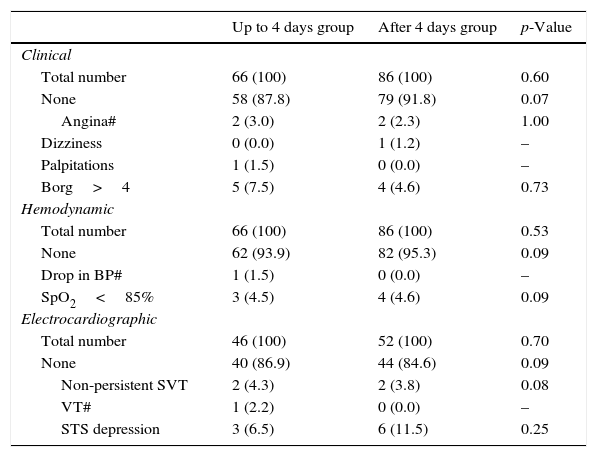
The frequency of clinical and hemodynamic complications was analyzed considering 152 patients, since the whole sample performed the 6MWT. The frequency of electrocardiographic complications, on the other hand, was analyzed considering 98 patients.
Considering the whole sample (152 patients), 37 (24.34%) had some type of complication during the test and six (3.9%) patients displayed a complication classified as severe (see Table 4 complications marked with #), four (2.6%) from Up to 4 Days Group and two (1.3%) from the After 4 Days Group (p=0.17). Further complications were observed in 31 (20.4%) patients, 14 (9.2%) from the Up to 4 Days Group and 17 (11.2%) from the After 4 Days Group (Table 4). None of the complications regarded as severe led to truly significant complications or death. No other outcomes, such as signs of diminished tissue perfusion, nausea, profuse sweating, or absence of a minimal increase in HR, were identified.
Complications displayed by patients with acute myocardial infarction subjected to the six-minute walk test.
| Up to 4 days group | After 4 days group | p-Value | |
|---|---|---|---|
| Clinical | |||
| Total number | 66 (100) | 86 (100) | 0.60 |
| None | 58 (87.8) | 79 (91.8) | 0.07 |
| Angina# | 2 (3.0) | 2 (2.3) | 1.00 |
| Dizziness | 0 (0.0) | 1 (1.2) | – |
| Palpitations | 1 (1.5) | 0 (0.0) | – |
| Borg>4 | 5 (7.5) | 4 (4.6) | 0.73 |
| Hemodynamic | |||
| Total number | 66 (100) | 86 (100) | 0.53 |
| None | 62 (93.9) | 82 (95.3) | 0.09 |
| Drop in BP# | 1 (1.5) | 0 (0.0) | – |
| SpO2<85% | 3 (4.5) | 4 (4.6) | 0.09 |
| Electrocardiographic | |||
| Total number | 46 (100) | 52 (100) | 0.70 |
| None | 40 (86.9) | 44 (84.6) | 0.09 |
| Non-persistent SVT | 2 (4.3) | 2 (3.8) | 0.08 |
| VT# | 1 (2.2) | 0 (0.0) | – |
| STS depression | 3 (6.5) | 6 (11.5) | 0.25 |
Values presented as frequency (percentage). BP, blood pressure; SpO2, peripheral oxygen saturation; STS, ST-segment; SVT, supraventricular tachycardia; VT, ventricular tachycardia; 6MWT, six-minute walk test. #Severe complications: angina, drop in BP, and VT.
This study suggests that the 6MWT is safe for evaluating patient HR following AMI, even when administered early. During the test, hemodynamic variables displayed physiological behavior of the heart rate and blood pressure. Some types of complications were observed in around 24% of patients. However, severe complications were observed only in 3.9% and disappeared when exercise ceased without any kind of intervention. There were no relevant statistical differences between groups. Therefore, we found no literature-based7,18,19 or experimental reason to justify the absolute contraindication of early performance of the 6MWT in patients following AMI.
In this sense, Sancho et al.7 evaluated the functional capacity of 23 patients from the fourth to the sixth day following AMI in the Coronary Care Unit and concluded that the 6MWT is a safe, simple, well-tolerated, and low-cost test for evaluating functional capacity. Moreover, Nogueira et al.18 carried out the 6MWT after exercise testing (the Bruce protocol) in 25 patients and concluded that the test provides a safe, reliable, and reproducible measure of the functional capacity of stable patients after uncomplicated AMI, even when performed within one week of the event.
Recently, a low frequency of serious adverse events during the 6MWT was found in hospitalized cardiac patients when administered two days after admission. Of the 30 patients, 13.3% had adverse effects considered as severe. However, the classification of severity was different and the sample included patients with higher risk, such as heart failure patients.19 Despite the higher identified percentage of severe complications during the test than the hypothesized percentage (3.9 and 2%, respectively), the frequency was still low and more than that, it did not lead to clinical complication or death.
Patients walked a reasonable distance during the 6MWT (85% of the expected distance), considering the proximity to the event and factors such as inappropriate floor and footwear and the circulation of people in the hallway. This condition reflects the real life condition that will be found in the majority of the hospitals that administer the test. Furthermore, although the main instruction for the test was to “walk as fast as possible, without running”,2 some patients clearly feared exertion and many did not walk at their maximum tolerated speed. Another factor mentioned by patients was their insecurity in walking after having undergone catheterization through the femoral artery. Many of them performed the test within 24h of the procedure. In these cases, the medical staff was asked to assess thoroughly the puncture sites. There were no related complications. In addition, in patients with STE AMI treated with fibrinolysis, the addition of 6MWT assessment pre-discharge to the traditional risk score improved the prediction of cardiovascular events at the 3-month follow-up.11
In association with the physiological behavior of the hemodynamic variables during the 6MWT, median peak HR was low – 104bpm, which corresponds to 63% of the maximum age-estimated HR and reflects the submaximal nature of the test.2 It must be considered that the level of the test, even with submaximal effort, can be higher than daily living tasks for some patients. However, in this study, the level of effort required for the test is consistent with that of basic activities of daily living (3.14 METS),1,2 such as showering or changing clothes.
Median resting HR was 76bpm, despite the fact that most patients were taking beta-blockers. A possible reason is the coincidence between the recently started medication and the early performance of the test. Nonetheless, the beta-blockers may have influenced the mild rise in HR and BP during exertion.14 Consequently, the median value of the double product was low,20 representing myocardial oxygen consumption, an extremely important variable during this stage of recovery following AMI.12
Although electrocardiographic complications were the most prevalent overall, 85.7% of the patients did not show electrocardiographic changes stemming from exertion during Holter monitoring. Nine patients displayed ST-segment depression during the 6MWT, a sign of low-load ischemia given that median energy expenditure for the test was 3.14 METs. Among all complications, this complication is noteworthy because it is a strong indicator of a poor prognosis.14
Between-group comparisonsThe number of patients with diabetes was higher in the Up to 4 Days Group. Nevertheless, it did not compromise the distance walked nor did it exacerbate complications. Another difference between groups was the higher number of days in the Coronary Care Unit in the After 4 Days Group. It could suggest the presence of some complications that could influence the results. However, some patients spent more days in the Coronary Care Unit waiting for tests and waiting for a room when discharged from Coronary Care Unit. Despite this, both groups presented few complications.
The decision to perform a comparison in this study between the 6MWT in the Up to 4 Days Group and in patients in the After 4 Days Group was based on three factors. Firstly, the 4-day limit for performing submaximal tests was established in the literature based on exercise testing.8,13 As the 6MWT is self-regulated and carried out on the ground, it requires much less effort2 and is compatible with activities of daily living.1,2 Our data confirmed this. Secondly, given the new technologies used for treating AMI, patients without complications stemming from the event are often discharged from the hospital in less than five days.12,14 In our study, median hospitalization time was 6 days. Finally, other studies have used the 6MWT to evaluate patient functional capacity following recent uncomplicated AMI.7,18
LimitationsSome limitations must be considered. Our data collection was not completely uninterrupted and not all patients underwent Holter monitoring, which was only available for the final 105 candidates. However, the profile of patients admitted to the Coronary Care Unit is fairly homogeneous, suggesting the validity of our results. The population studied was predominantly characterized by patients with up to 2 injured coronary arteries and without any significant left ventricular dysfunction, and therefore our results cannot be transposed to populations with a more severe clinical profile. This is an observational performance study and information from multicenter randomized clinical trials would be desirable to validate our results. However, we are unaware of any initiative with such objectives, and our results therefore constitute robust evidence in favor of the safety of performing the 6MWT shortly after AMI.
Clinical implicationsOur results indicated the safety of the 6MWT and, in association with other studies,7,19 may support including the test in protocols for the hospital management of AMI. According to our study, Coronary Care Unit discharge seems to be the ideal moment for performing the 6MWT. Meanwhile, it may be more feasible to perform it prior to hospital discharge. In addition, the possibility of using a simple and practical test that may reveal high prognostic signs, such as ST-segment changes, can help make a more assertive case for driving these patients.
ConclusionThe 6MWT is a safe instrument for evaluating patient function capacity following uncomplicated AMI. During the test, hemodynamic variables displayed a physiological behavior and 3.9% of the patients displayed some type of important complication, none of which led to an unfavorable outcome. Moreover, the performance and safety of the test by the Up to 4 Days Group resembled those of the After 4 Days Group. Therefore, there is no experimental or literature-based evidence to justify the absolute contraindication of the early performance of the 6MWT in this population. The availability of a safe and viable instrument for the early evaluation of these patients’ functional capacity may facilitate their inclusion in cardiac rehabilitation programs.
Conflict of interestThe authors declare no conflicts of interest.